Translate this page into:
Granuloma faciale – A case report
*Corresponding author: Sumi Thomas, Aster DMPC, Al Muteena, Deira - 25570, Dubai, United Arab Emirates. sumithomas1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thomas S. Granuloma faciale – A case report. J Skin Sex Transm Dis 2021;3(1):91-3.
Abstract
Granuloma faciale is a rare localized idiopathic inflammatory skin disorder that manifests as reddish-brown or violaceous papules, plaques, or nodules. It usually occurs in middle-aged adults and is rare in children. We are reporting a case of granuloma faciale in a 31-year-old male.
Keywords
Granuloma faciale
Inflammatory skin disorder
Grenz zone
INTRODUCTION
Granuloma faciale is a benign, chronic inflammatory dermatosis that presents as single or multiple violaceous or reddish-brown papules, plaques, or nodules ranging in size from a few millimeters to several centimeters.[1] The most common site is the face. A clear grenz zone, mixed dermal inflammatory infiltrate, and vascular damage are the histopathology findings. In the absence of treatment, the lesions may persist indefinitely. Spontaneous resolution is rare. Response to treatment is variable, and hence, the treatment can be challenging.
CASE REPORT
A 31-year-old man presented with an asymptomatic, gradually enlarging reddish lesion on the root of the nose of 6 months duration. The patient did not give any significant medical history or history of trauma, irradiation, or photosensitivity.
General examination was within normal limits. Dermatological examination showed a single erythematous, indurated plaque of 2 cm × 3 cm size with well-defined borders. The surface of the lesion was smooth with prominent follicular orifices and telangiectasia [Figure 1]. Anemia (hemoglobin: 11g/dl and mean corpuscular volume: 74 femtoliters) and raised erythrocyte sedimentation rate (66 mm/h) were the abnormalities noted in complete hemogram. Serology for antinuclear antibodies was negative. Histopathological evaluation showed the separation of the epidermis from the dermis. Dermis showed mild fibrosis and dense inflammatory infiltrate composed of lymphocytes, plasma cells, neutrophils, and occasional eosinophils [Figure 2]. There were no evident vascular changes. No granuloma was seen. No fungal elements were seen in Giemsa stain.

- Erythematous plaque with follicular prominence and telangiectasia on the root of the nose.
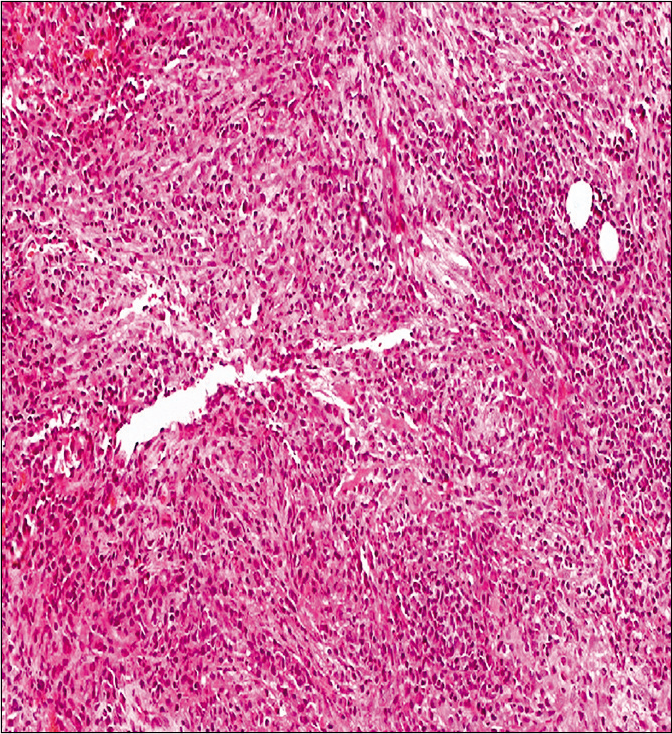
- Biopsy from the erythematous plaque showing mild dermal fibrosis and mixed inflammatory infiltrate composed of lymphocytes, plasma cells, neutrophils, and occasional eosinophils (H and E, ×100).
With these clinical and histopathology findings, a diagnosis of granuloma faciale was made. The patient was prescribed topical betamethasone dipropionate cream (0.05%) in the morning and tacrolimus 0.1% ointment at night along with hematinics. After 2 months of treatment, there was a mild reduction in induration and erythema of the lesion.
DISCUSSION
Granuloma faciale is a rare disease of unknown etiology which is more common in middle-aged men. “Granuloma faciale” is a misnomer because granuloma formation is not a histopathology feature of this disease.[2] Vasculitis is a common histopathology finding suggesting that granuloma faciale may be a localized form of cutaneous small vessel vasculitis. Hypersensitivity reactions, actinic exposure, infections, trauma, and radiation are the proposed etiological factors.[3,4] Although the most common presentation is a solitary plaque on the face as in our case, multiple skin lesions and extra facial involvement may also occur. The most common sites for facial lesions are the forehead, cheeks, and the nose. Prominent follicular orifices and telangiectasia are usually present. Rhinophyma, like lesions and keloidal lesions, are seen rarely.[5,6] There are reports that associate granuloma faciale with eosinophilic angiocentric fibrosis, affecting the sinus tract and the upper respiratory airways.[7]
Characteristic histopathology is a diffuse and polymorphous inflammatory infiltrate involving the upper half of the dermis composed of neutrophils, eosinophils, lymphocytes, histiocytes, and plasma cells. A thin zone of uninvolved papillary dermis (grenz zone) separates the epidermis from the inflammatory infiltrate. Dermal fibrosis, often presenting as concentric fibrosis around blood vessels, is another common finding. The frequent observation of vascular damage (perivascular inflammatory infiltrate, leukocytoclasis, and extravasated red blood cells) supports the theory that granuloma faciale may be a localized form of cutaneous small vessel vasculitis.[1]
Differential diagnoses include sarcoidosis, cutaneous lymphoma, pseudolymphoma, discoid lupus erythematosus, erythema elevatum diutinum, and granulomatous rosacea.
Although granuloma faciale is a benign and usually asymptomatic disorder, the chronic course and cosmetic disfigurement are distressing to the patients. Topical tacrolimus, cryotherapy, and topical or intralesional corticosteroids are the commonly used first-line therapies.[8,9] Topical tacrolimus is well tolerated with fewer side effects. Other treatment options include pulsed dye laser, oral dapsone, and intralesional rituximab.
CONCLUSION
Granuloma faciale should be considered in the differential diagnosis of persistent erythematous plaques on the face. Skin biopsy can help to reach a correct diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Granuloma faciale: A clinicopathologic study of 66 patients. J Am Acad Dermatol. 2005;53:1002-9.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum-a chronic leukocytoclastic vasculitis microscopically indistinguishable from granuloma faciale? J Cutan Pathol. 2011;38:876-83.
- [CrossRef] [PubMed] [Google Scholar]
- Granuloma faciale: A clinicopathological study of 11 Cases. J Am Acad Dermatol. 2004;51:269-73.
- [CrossRef] [PubMed] [Google Scholar]
- Keloidal granuloma faciale after CO2 laser treatment for melanocytic naevus. J Eur Acad Dermatol Venereol. 2009;23:611-2.
- [CrossRef] [PubMed] [Google Scholar]
- Rhinophyma-like granuloma faciale. J Eur Acad Dermatol Venereol. 2006;20:881-2.
- [CrossRef] [PubMed] [Google Scholar]
- A rare case of keloidal granuloma faciale with extra-facial lesions. Indian Dermatol Online J. 2013;4:27-9.
- [CrossRef] [PubMed] [Google Scholar]
- Concurrent granuloma faciale and eosinophilic angiocentric fibrosis. Br J Dermatol. 2005;153:851-3.
- [CrossRef] [PubMed] [Google Scholar]
- Topical tacrolimus in the treatment of granuloma faciale. Int J Dermatol. 2010;49:1463-5.
- [CrossRef] [PubMed] [Google Scholar]
- Granuloma faciale: Successful treatment of nine cases with a combination of cryotherapy and intralesional corticosteroid injection. Int J Dermatol. 1997;36:548-51.
- [CrossRef] [PubMed] [Google Scholar]






