Translate this page into:
Eccrine angiomatous hamartoma – A rare painful skin tumor
*Corresponding author: Niveditha M, Department of Dermatology, Venereology, and Leprosy, Government Medical College, Thrissur, Kerala, India. nivedithapknm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Niveditha M, Prathap P, Asokan N. Eccrine angiomatous hamartoma – A rare painful skin tumor. J Skin Sex Transm Dis. 2024;6:156-9. doi: 10.25259/JSSTD_66_2023
Abstract
We report a 68-year-old male with a progressively enlarging, reddish raised painful lesion on the right arm for the previous 3 years. The starch iodine test was positive, dermoscopic findings were yellowish-brown globules on an erythematous background. Biopsy from the lesion showed the presence of eccrine glands, hair follicles, and lobules of capillary sized vessels surrounding hair follicles in the dermis. On immunohistochemistry, epithelial membrane antigen (a marker for eccrine gland) and CD31 (endothelial marker) were positive. A final diagnosis of eccrine angiomatous hamartoma (EAH) was made. There should be a high index of suspicion about EAH if the skin lesions are reddish and tender with associated localized sweating.
Keywords
Painful
Skin tumor
Eccrine angiomatous hamartoma
INTRODUCTION
Eccrine angiomatous hamartoma (EAH) is a rare nevoid proliferation of normal eccrine glands, small blood vessels, and occasionally other elements such as fatty tissue and pilar structures with variable clinical manifestations.[1] Here, we report a case of EAH, which presented as a painful skin tumor.
CASE REPORT
A 68-year-old male presented to the dermatology outpatient department with a progressively enlarging, reddish raised lesion on the right arm for the previous 3 years. Over a period, similar lesions appeared adjacent to it. There was pain and increased sweating on the lesional skin. There was no history of itching or bleeding from the lesion. He had diabetes mellitus and was taking tablet metformin 500 mg for the previous 5 years. On examination, there was a well-defined, tender, reddish non-blanching plaque with a purplish hue, of 7 × 5 cm size on the right arm, with seven satellite erythematous papules of 0.3 × 0.3 to 1 × 1 cm around it [Figure 1]. On pressing, the surface of the plaque exuded drops of a transparent, colorless fluid. Starch iodine test demonstrated increased sweating on the lesional skin compared to the normal skin [Figure 2]. On dermoscopy, yellowish-brown globules on an erythematous background were noted [Figure 3].

- Well-defined, tender, reddish, non-blanching plaque with a purplish hue of 7 × 5 cm size on the right arm, with seven satellite erythematous papules of 0.3 × 0.3– 1 × 1 cm around it.

- Increased sweating in lesional skin on starch iodine test (blue arrow).
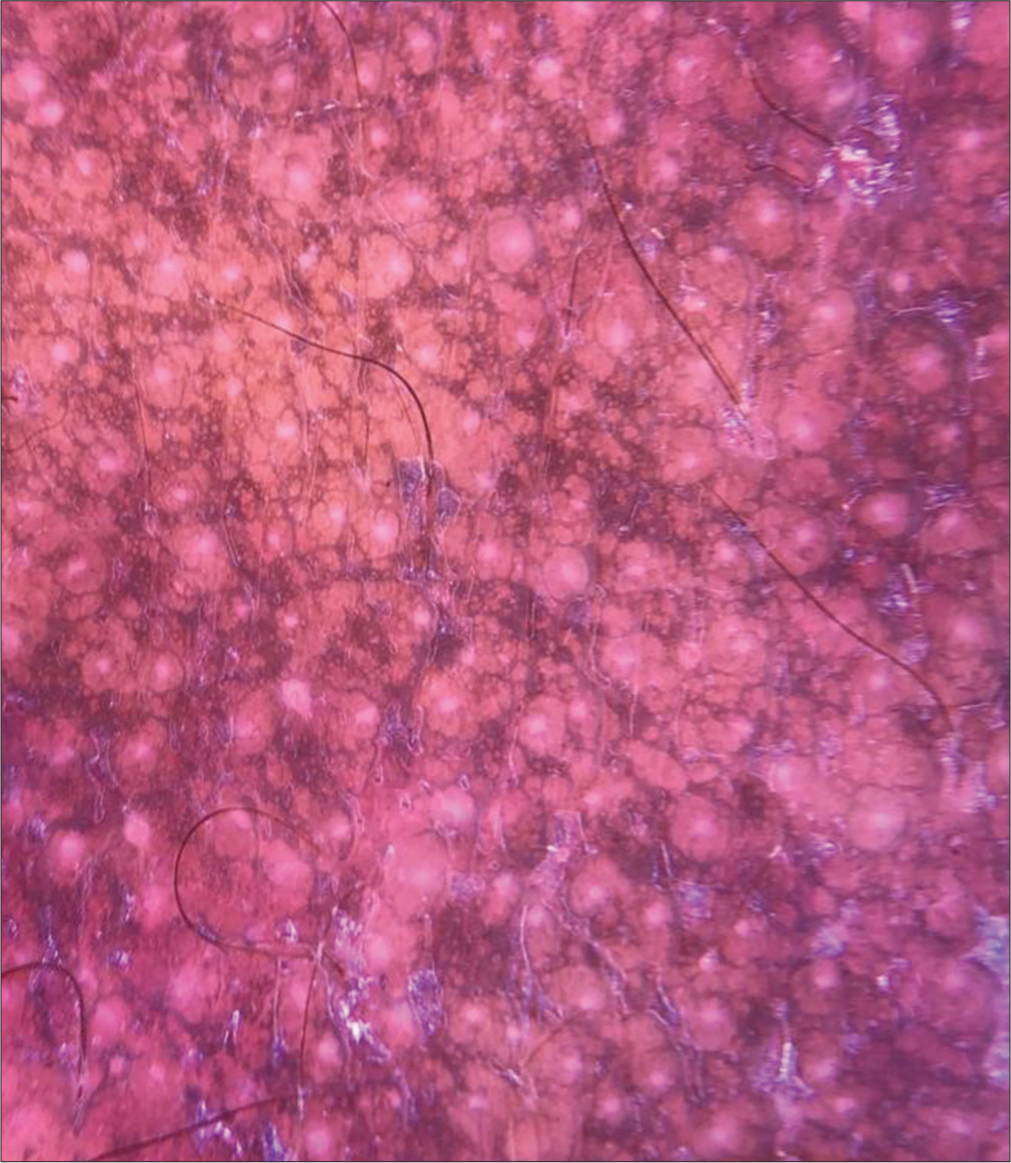
- Dermoscopy showing yellowish-brown globules on an erythematous background (DermLite 4, ×10).
Hemogram, liver function tests, and renal function tests were normal. Viral markers for serum human immunodeficiency virus, hepatitis B virus surface antigen and anti-hepatitis C virus were negative. Ultrasonogram of the skin and soft tissue of the right upper arm showed the presence of multiple vascular channels in the subcutaneous plane with high resistant flow in the region of the plaque without extension into intramuscular space. Biopsy from the lesion showed the presence of eccrine glands, hair follicles, and lobules of capillary-sized vessels encircling hair follicles in the dermis [Figure 4]. On immunohistochemistry, epithelial membrane antigen (a marker for the eccrine gland) and CD31 (endothelial marker) were positive [Figures 5 and 6].
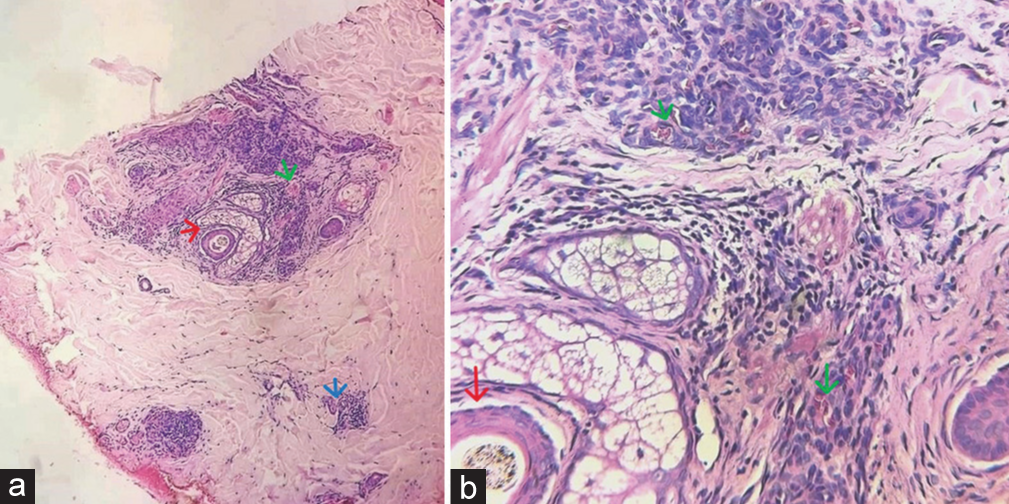
- (a): Biopsy from the plaque on right arm showing eccrine glands (blue arrow), hair follicles (red arrow), and lobules of capillarysized vessels (green arrow) encircling the hair follicle in the dermis (Hematoxylin & eosin, ×100); (b): Histopathology from the plaque on right arm showing lobules of capillary-sized vessels (green arrow) encircling the hair follicle in the dermis (Hematoxylin & eosin, ×400)
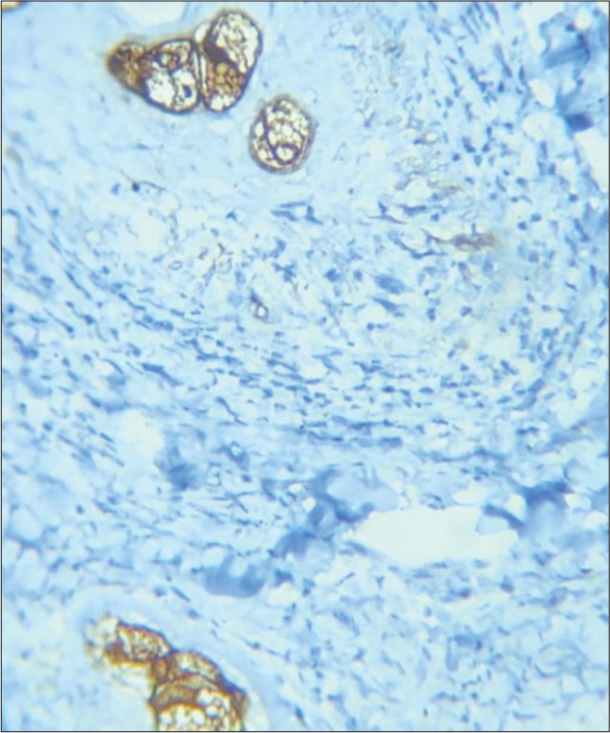
- Biopsy from plaque on right arm cells showing positive for epithelial membrane antigen (Immunohistochemistry, ×20).
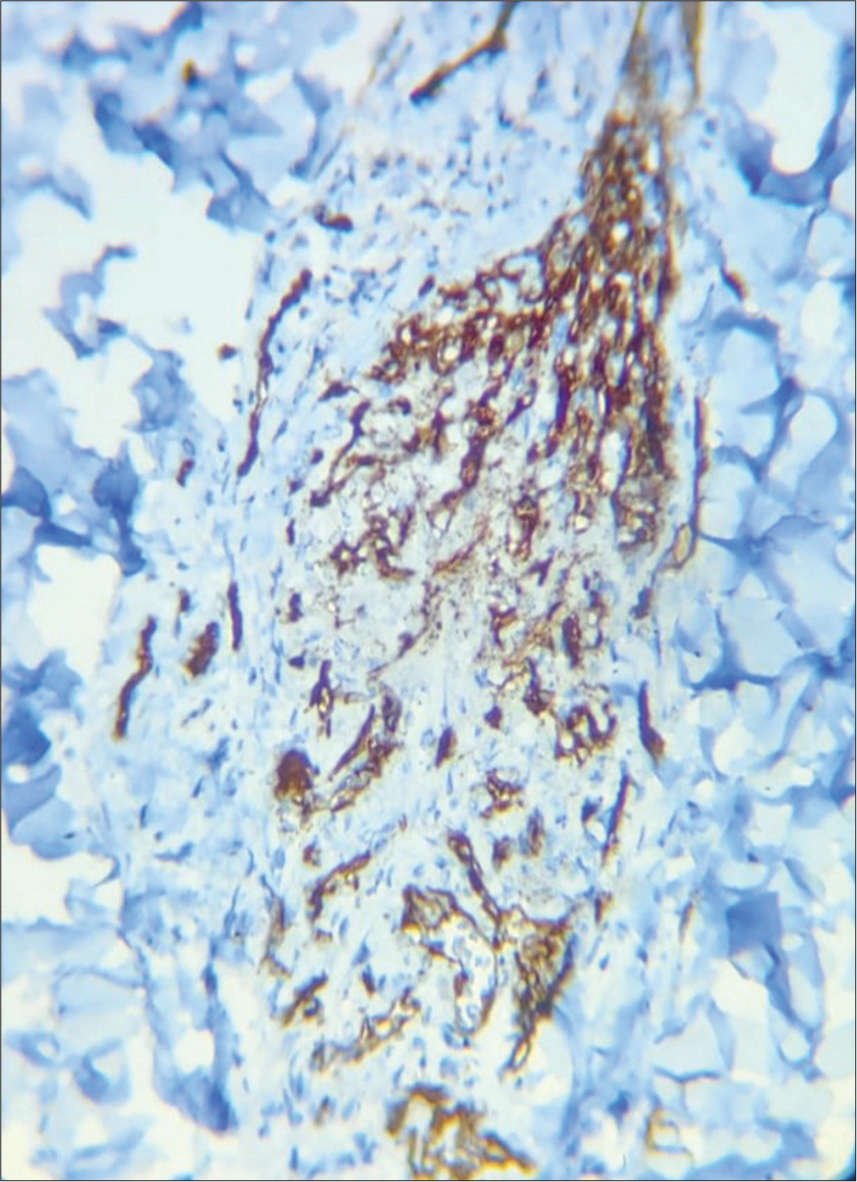
- Biopsy from plaque on right arm cells showing positive for CD 31 (Immunohistochemistry, ×40).
DISCUSSION
The popular mnemonic for painful skin tumors is “BLEND TAN EGG”, which includes blue rubber bleb nevus, leiomyoma, eccrine spiradenoma, neuroma, dermatofibroma, tufted angioma, angiolipoma, neurilemmoma, endometriosis, granular cell tumor, and glomus tumor.[2]
Among these tufted angioma and eccrine spiradenoma were considered as differential diagnosis. EAH, reactive angioendotheliomatosis, and Kaposi sarcoma were also considered in the differential diagnosis.
EAH is a rare benign vascular tumor first described by Lotzbeck in 1859. The term eccrine angiomatous hamartoma was coined by Hyman et al.[3] The disease is more common in childhood, is usually solitary, and more commonly follows an acral distribution. It presents as an angiomatous lesion generally asymptomatic but can be associated with pain, focal hyperhidrosis, and hypertrichosis. There are hyperkeratotic and verrucous variants. Histologically, it is characterized by a dermal proliferation of blood vessels and well-differentiated eccrine secretory and ductal elements. EAH does not have any malignant potential nor do they resolve spontaneously. Dermoscopic patterns reported are multiple yellow, confluent nodules having a popcorn shape, in a background of erythema and linear and arborizing blood vessels (popcorn pattern)[4] and brown globules, in a background of erythema, and a pseudoreticular depigmentation around the globules (spitzoid pattern).[5]
EAH is histopathologically characterized by an increased number of eccrine glands in the superficial dermis, with blood vessels between and around the glands and ducts. Vessels vary in size but are predominantly small and lined by endothelial cells. Other areas of the dermis show smooth muscle bundles, fat cells, and focal areas of myxoid change.
In a retrospective series of EAH of ten patients by Shin et al., 70% of patients experienced pain and tenderness on the lesion.[6] Lin et al. reported that pain (60%) was the most common features associated with EAH.[1]
Tufted angioma presents as slowly expanding, mottled, red-to-purple patches and firm plaques superimposed with papules and nodules on neck, shoulders, trunk or groins with pain, tenderness, and localized hyperhidrosis and hypertrichosis. The usual age of presentation is during infancy or childhood, with a majority of lesions arising before the age of 5 years. Histologically, it is characterized by multiple, discrete lobules of tightly packed capillaries in a cannonball pattern within the dermis and sometimes in subcutis.[2] The dermoscopic finding of tufted angioma is skin-colored to light pink structureless areas.[7]
Eccrine spiradenoma commonly presents as a painful, blue-colored, solitary nodule but may rarely present as multiple nodules or in a linear or zosteriform pattern. Histopathology of eccrine spiradenoma shows deeply basophilic stained, sharply marginated lobules lying freely in the dermis. Two types of epithelial cells are present – small cells with dark peripheral nuclei and pale cells with central nuclei. A characteristic appearance is the “blue balls” in the dermis.[2] On dermoscopy, eccrine spiradenoma shows a structureless pattern with blue clods and a vascular pattern with serpentine, branched vessels.[8]
Reactive angioendotheliomatosis present as multiple erythematous or hemorrhagic macules, papules and plaques on trunk and limbs. Systemic associations such as bacterial endocarditis, peripheral vascular atherosclerotic diseases, cryoglobulinemia, liver and renal disease, antiphospholipid antibody syndrome, amyloidosis, and sarcoidosis can be present. Histologically, multifocal proliferation of capillaries with plump endothelial cells is present in dermis and subcutaneous tissue.[9]
Kaposi sarcoma is a multifocal endothelial proliferation caused by human herpes virus 8. Four main subtypes are classic type, endemic, iatrogenic, and acquired immunodeficiency syndrome-associated. Cutaneous lesions consist of dark blue or purple patches, plaques, or nodules, usually in extremities, ears or nose. Histologically, in the patch stage, there is a mild increase in the number of vessels, arranged horizontally, dissecting through the collagen bundles, around adnexa, and surrounding preexisting vessels, along with lymphoplasmacytic infiltrate, extravasated red blood cell, and hemosiderin deposition. The plaque stage has vessels lined by plump endothelial cells surrounded by spindle cells. In the tumor stage, there are circumscribed masses of spindle cells with slit-like spaces.[10] Bluish-reddish coloration, multicolored areas showing various colors of the rainbow spectrum, scaly surface, and small brown globules are the dermoscopic findings in Kaposi sarcoma.[11]
A final diagnosis of EAH was made based on the morphology of the lesion, starch iodine test, dermoscopic, biopsy, and immunohistochemistry findings. Treatment is indicated in EAH if there is severe pain, excessive sweating, or progressive growth, or for cosmetic concerns. Surgery is the treatment of choice. An excisional biopsy may be curative for small tumors but, a wider surgery may be needed for larger lesions. Botulinum toxin, to control excessive sweating, and polidocanol 1% (a sclerosing agent) injection into the vascular component of the tumor are other treatment options.[12]
CONCLUSION
To conclude, we report this case because EAH is a rare cause of tender skin lesions. To the best of our knowledge, only <100 cases have been reported in the literature. The older age of onset, multiplicity of lesions, and absence of hypertrichosis are other unusual features of this case. Since pain and tenderness are common features of EAH, we suggest adding EAH to the mnemonic “BLEND TAN EGG” and changing it to “BLENDE TAN EGG.” There should be a high index of suspicion about EAH if the skin lesions are reddish and tender with associated localized sweating.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Neelakandhan Asokan is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Eccrine angiomatous hamartoma: A retrospective study of 15 cases. Chang Gung Med J. 2012;35:167-77.
- [CrossRef] [Google Scholar]
- Painful tumors of the skin-from ENGLAND to LEND AN EGG to BLEND TAN EGG. Indian J Dermatol Venereol Leprol. 2019;85:231-4.
- [CrossRef] [Google Scholar]
- Dermoscopy of eccrine angiomatous hamartoma: The popcorn pattern. JAAD Case Rep. 2018;4:165-7.
- [CrossRef] [Google Scholar]
- Dermoscopy of eccrine angiomatous hamartoma: The spitzoid pattern. JAAD Case Rep. 2018;4:835-6.
- [CrossRef] [PubMed] [Google Scholar]
- Eccrine angiomatous hamartoma: A review of ten cases. Ann Dermatol. 2013;25:208-12.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic analysis of vascular malformations and tumors based upon dominant vascular dermoscopic features: A retrospective analysis from a tertiary care center of East India. Cureus. 2022;14:e26292.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopic pattern of a spiradenoma. Dermatol Pract Concept. 2012;2:39-40.
- [CrossRef] [PubMed] [Google Scholar]
- Soft tissue tumours and tumour like conditions: Reactive angioendotheliomatosis In: Griffiths EM, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook's textbook of dermatology (9th ed). UK: WILEY Blackwell; 2016.
- [Google Scholar]
- Kaposi sarcoma In: Griffiths EM, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook's textbook of Dermatology (9th ed). UK: WILEY Blackwell; 2016.
- [Google Scholar]
- Dermoscopy of Kaposi's sarcoma: Areas exhibiting the multicoloured “rainbow pattern”. J Eur Acad Dermatol Venereol. 2009;23:1128-32.
- [CrossRef] [PubMed] [Google Scholar]
- Eccrine angiomatous hamartoma: A report of 2 Cases. Actas Dermosifiliogr. 2011;102:289-92.
- [CrossRef] [PubMed] [Google Scholar]






