Translate this page into:
Dermatodaxia mimicking knuckle pads
*Corresponding author: Yasmeen Jabeen Bhat, Department of Dermatology, Venereology and Leprosy, Government Medical College, Srinagar, Jammu and Kashmir, India. yasmeenasif76@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Angmo R, UI Islam MS, Bhat YJ. Dermatodaxia mimicking knuckle pads. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_17_2025
Dear Editor,
We report the case of a 14-year-old male patient who presented with a pattern of recurrent self-injuries involving his fingers and hands. It was noted that the behavior resulted from a prolonged practice of biting his skin as a coping mechanism during episodes of stress, anxiety, or boredom. Over the past 1-2 years, the patient observed an increase in the size of the lesions and subsequently sought consultation at our outpatient department for cosmetic concerns. He had not sought any medical advice before this visit. He sometimes resorted to chewing on these areas to respond to heightened tension. The onset of this behavior dates back to when he was 8 years old, with no reported history of substance abuse. The patient had no significant medical history or family history of similar complaints. Notably, no additional skin lesions were identified on other parts of his body.
Cutaneous examination showed multiple well-defined skin-colored to brownish hyperkeratotic and lichenified plaques, variable in size and shape, measuring 1–1.5 cm in diameter, distributed bilaterally on the dorsal surfaces of the proximal interphalangeal, distal interphalangeal, and metacarpophalangeal joints. Dermoscopy revealed structureless yellowish areas with increased skin marking and surrounding erythema [Figure 1a-d]. Hair, nails, and mucosae were normal.
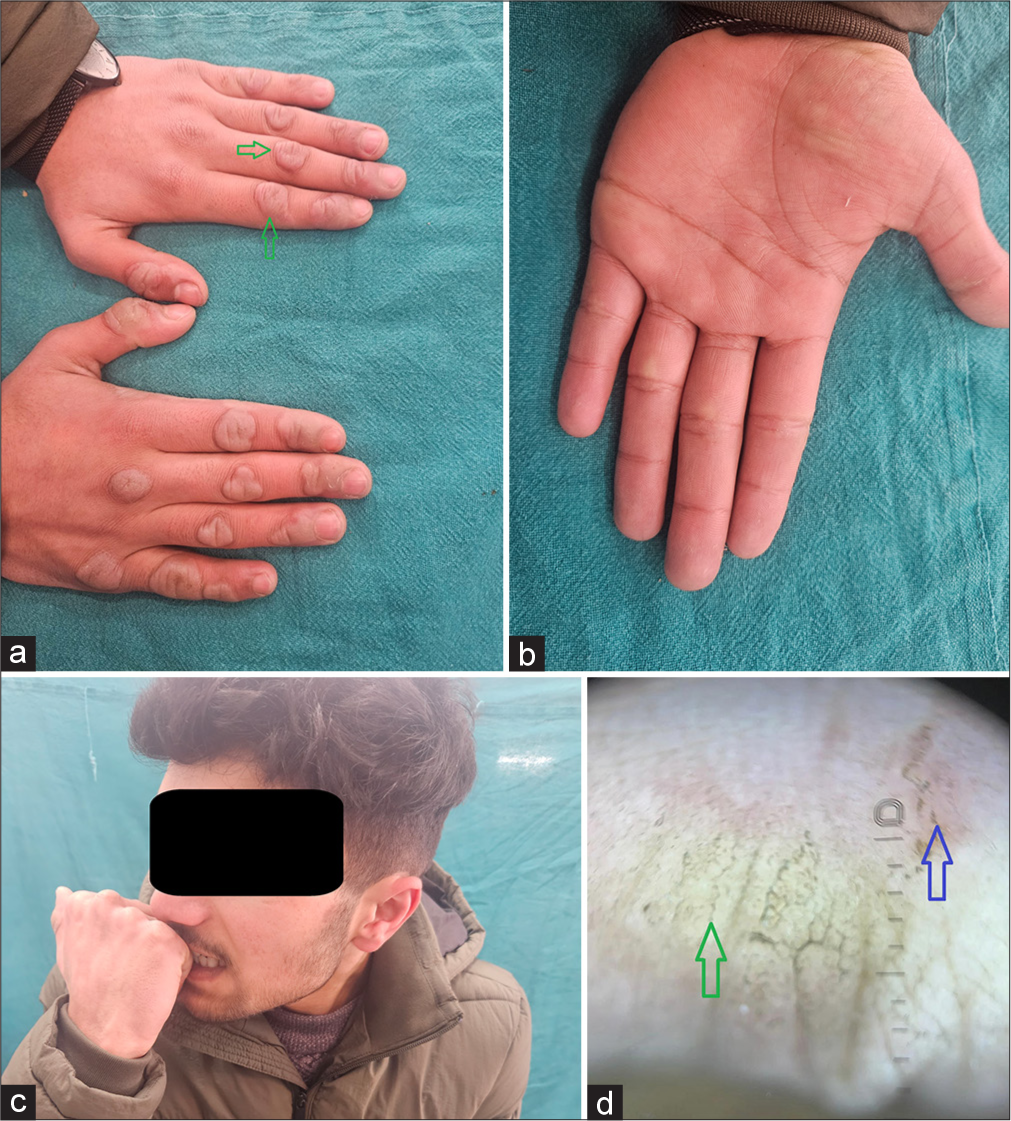
- Multiple skin-colored hyperkeratotic plaques (green arrow) over the dorsal and palmer aspect of hands and fingers bilaterally, mainly over joints with rough surfaces and thick adherent brown scales; (c): patient demonstrating the technique he would use to bite the skin; and (d): dermoscopy showing structureless yellowish areas (green arrow) with increased skin marking and surrounding erythema (blue arrow) (DermLite, DL5, ×10).
Based on the history and clinical and dermoscopic examination, a diagnosis of calluses due to dermatodaxia was made. The lesions were treated with topical keratolytic and moisturizers. The patient was referred to the psychiatrist for further assessment. He was treated as a case of obsessive-compulsive disorder (OCD), treated with selective serotonin reuptake inhibitors and antipsychotics, and planned for habit reversal treatment/training.
Dermatodaxia derived from a Greek word (derma-skin and daxia-bitting), is categorized as an OCD. Based on the new international classification of psychodermatalogical disorders, dermatodaxia is categorized under the subgroup of OCD-related disorders.[1,2] It describes people who habitually bite their skin but do not consume the skin they have bitten. Dermatodaxia can be an isolated body-focused repetitive behavior or occurs with other related disorders such as dermatillomania, trichotillomania, and onychophagia.[1-3]
Initially, the affected individual was called a wolf-biter, which was later modified as dermatophagia in which a person chews and consumes their own skin. Later on, it was changed to a more appropriate term called dermatodaxia.[3] Dermatodaxia is usually asymptomatic, unilateral, and affects a solitary site. Individual lesions typically appear as lichenified, callous-like, and thick nodules. The forearm, hands, and fingers are the most common dermatodaxia sites. The knuckles may or may not be involved. Uncommon sites include elbows, knees, feet, or nasal bridges.[2,4]
These need to be differentiated from knuckle pads, which occur due to repetitive friction or can be idiopathic. Knuckle pads, present as well-demarcated soft to firm, smooth lesions with absent repetitive behavioral history, showing a variable or slow response to therapy.[2,4] The diagnosis of dermatodaxia is done by meticulous history and examination, including dermoscopy and histopathological analysis, wherever deemed necessary. Dermoscopy can differentiate them with findings of irregularly thickened skin, erosions, scaling crusting, linear or dotted vessels, and inflamed areas in dermatodaxia, while homogenous thickened skin with sparse or absent vascular structures in knuckle pads. Histopathology can reveal non-specific findings of hyperkeratosis, acanthosis, dilated capillaries, and dermal fibrosis in dermatodaxia. Knuckle pads show more or less similar histopathology with absent vascular changes.[4]
Treatment includes behavioral therapy addressing underlying stress or compulsive habits. Protective measures such as gloves or bandages were to prevent further trauma. Topical therapy, including keratolytics and moisturizing agents, can be tried. Corticosteroids can be used in case of inflammation. Psychopharmacological management, including selective serotonin reuptake inhibitors with cognitive behavioral therapy for habit reversal, forms an important cornerstone of treatment.[1,4]
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- The classification of obsessive-compulsive and related disorders in the ICD-11. J Affect Disord. 2016;190:663-74.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatophagia simulating callosities. Dermatol Psychosom Dermatol Psychosom. 2003;4:42-3.
- [CrossRef] [Google Scholar]
- Dermatophagia or dermatodaxia? J Am Acad Dermatol. 2005;53:365.
- [CrossRef] [PubMed] [Google Scholar]





