Translate this page into:
Cutaneous leishmaniasis among tribals in a Northern district of Kerala
*Corresponding author: T. V. Shailaja, Department of Dermatology, District Hospital Nilambur. Malappuram, Kerala, India. shailajapramod1971@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shailaja TV, Sindhu CB, Balakrishnan S, Shubin C, Siani P. Cutaneous leishmaniasis among tribals in a Northern district of Kerala. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_82_2024
Abstract
In Kerala, cases of cutaneous leishmaniasis (CL) were seen mainly as imported from Middle-Eastern countries. Recently, many indigenous cases were reported from parts of the Western Ghats. This case series describes cases from routine dermatology surveys in tribal schools and hostels, contact surveys of the index cases, and cases attending the Outpatient Department from August 2022 to July 2023. The index case was detected as part of a school survey and was confirmed using histopathology and polymerase chain reaction (PCR). Following this, surveys were conducted in different tribal colonies in search of contact cases. We studied a total of 16 patients with asymptomatic skin lesions ranging from plaques to nodules without any systemic involvement. All sixteen cases were positive for PCR for leishmaniasis and the species Leishmania donovani (LD) was identified from all of them. Histopathology showed LD bodies in nine cases. Patients were treated with either systemic antifungal alone or with a combination of systemic antifungal with cryotherapy. All the patients responded well to treatment. Patients treated with fluconazole and cryotherapy showed better response. We conclude that active and passive surveillance in endemic areas will help in early detection cases of CL addressing their continued presence in the Western Ghats. Diagnosis can be confirmed with histopathology and PCR analysis.
Keywords
Cutaneous leishmaniasis
Leishmania donovani
LD bodies
Polymerase chain reaction
INTRODUCTION
Leishmaniasis, though endemic in more than 88 countries in Africa, Asia, Europe, and North and South America, is classified as one of the most neglected tropical diseases by the World Health Assembly.[1] The clinical presentation of leishmaniasis in humans ranges from visceral leishmaniasis (VL) cutaneous leishmaniasis (CL), mucocutaneous, zoonotic cutaneous, and post-kala-azar dermal leishmaniasis. CL in India is confined to hot and dry northwestern regions and the Thar desert of Rajasthan. The first imported cases of CL were reported from Kerala in 1988.[2] Indigenous cases were reported in subsequent years from Malappuram,[3] Trivandrum, and Kollam districts in the state.[4,5]
Leishmaniasis is a vector-borne disease caused by protozoan parasites of the genus Leishmania spp. The disease manifests as asymptomatic papules and plaques, which show granulomatous inflammation in histopathology. The disease mimics leprosy in its clinical presentation, which is endemic in countries that have a higher prevalence of CL, making an accurate diagnosis quite challenging and may result in misdiagnosis and delay in treatment. The diagnostic test for CL is PCR for Leishmania donovani (LD) in tissue specimens, which is often not available in many of the peripheral centers of the developing world where the disease is prevalent. Although the diagnostic gold standard of CL is the demonstration of LD bodies, this is not a sensitive test.[6] At present, rapid diagnostic tests and polymerase chain reaction (PCR) are being used for the diagnosis of this disease.[7]
We report here a series of 16 cases of CL from tribal colonies.
The continued presence of leishmaniasis in parts of Kerala poses a threat to the leishmaniasis elimination and maintenance program.
CASE REPORT
Our institution is a secondary-level hospital in the public sector conducting specialty outpatient departments (OPDs) in dermatology, in addition to other OPDs. School surveys were conducted in tribal schools and hostels of the district between August 2022 and July 2023 by the Department of Dermatology as a part of a routine camp for the detection of Leprosy. The index case was detected in a school camp, and a few more cases from other camps were conducted in the tribal hostel. The index case was a 13-year-old boy who presented with an asymptomatic nodule on the forearm noticed on examination, from which a biopsy was taken considering Hansen’s disease and CL as differential diagnoses. Biopsy revealed granulomatous inflammation with plenty of LD bodies. A skin biopsy was taken and sent for PCR and reported as positive. Contact screening was conducted and we got the second case from the same colony. The dermatology camp was conducted in another nearby tribal hostel. Students were screened for asymptomatic papules, plaques, and nodules. Patients were referred to our institution and a biopsy was taken for histopathology and PCR. Subsequently contact surveys were conducted in tribal colonies where the Leishmaniasis-positive cases resided. In addition, patients diagnosed from the Dermatology OPD of our hospital during the same period were also included. All cases were evaluated clinically on an outpatient basis by the dermatologist. Tissue samples were sent for histopathological examination to the nearest tertiary care center. In addition, a skin biopsy was sent for PCR study at Vector Control Research Center (VCRC) Kottayam. A 5-mm punch biopsy was taken for histopathology report, as well as a PCR study. Specimen for histopathological examination was sent to our district’s tertiary care hospital in 10% formalin, and for PCR analysis, the specimen was taken in normal saline and sent to VCRC Kottayam, including a blood sample in ethylene diamine tetra acetic acid. Histopathology slides were stained with routine hematoxylin and eosin and special stains Geimsa and periodic acid-schiff for identifying LD bodies and PCR for Leishmania and species identification. Deoxyribonucleic acid (DNA) sequence-based PCR was done for Leishmania.
The data from individual cases were entered in MS Excel and analyzed using descriptive statistics. The study was approved by the Institutional Ethics Committee (IEC/GMCM/131, dated May 18, 2024). Written informed consent was obtained for the biopsy procedures from patients. Patient anonymity has been maintained throughout the study. Data from the positive cases are presented as case series.
A total of 16 cases of CL were detected from the surveys conducted at tribal schools and tribal colonies during the time period. Fifteen out of the 16 cases were detected during school surveys carried out by our health center in two tribal schools and subsequent contact surveys carried out in the residential areas of the positive cases. One patient, a 12-year-old child, was brought to our dermatology OPD for treatment of his skin lesions. Skin biopsy was taken from all cases and sent for histopathology. Histopathology in all cases showed granuloma. Only four cases had inclusion bodies suggestive of LD bodies. PCR using multiple genetic markers was positive in all cases. Species were identified as LD complex in 16 cases based on DNA sequencing. All of the 16 cases were diagnosed as CL as they showed PCR positivity for Leishmania.
Of the 16 patients, 15 were tribals. Age ranged from 10 to 47 years, with a mean age of 19.4 years (SD ± 10.5 years). The majority (56.25%) were males. Duration of disease ranged from 8 months to 4 years. Thirteen patients had single lesions (81.2%) disease, whereas 3 (18.8%) had more than one lesion. The main sites affected were exposed areas such as the leg (5.26%), trunk (5.26%), forearm (4.20%), arm (3.15%), thigh (2.10%), and face (1.5%). The distribution of sites affected is given in Figure 1. Nine patients (56.25%) presented with nodular skin lesions and others (7, 43.75%) manifested with plaques. Clinical images of various types of skin lesions are given in Figures 2a and b. None of the skin lesions showed ulceration. None of the affected patients showed any systemic involvement. All lesions were asymptomatic, and no sensory impairment was detected over the lesions.
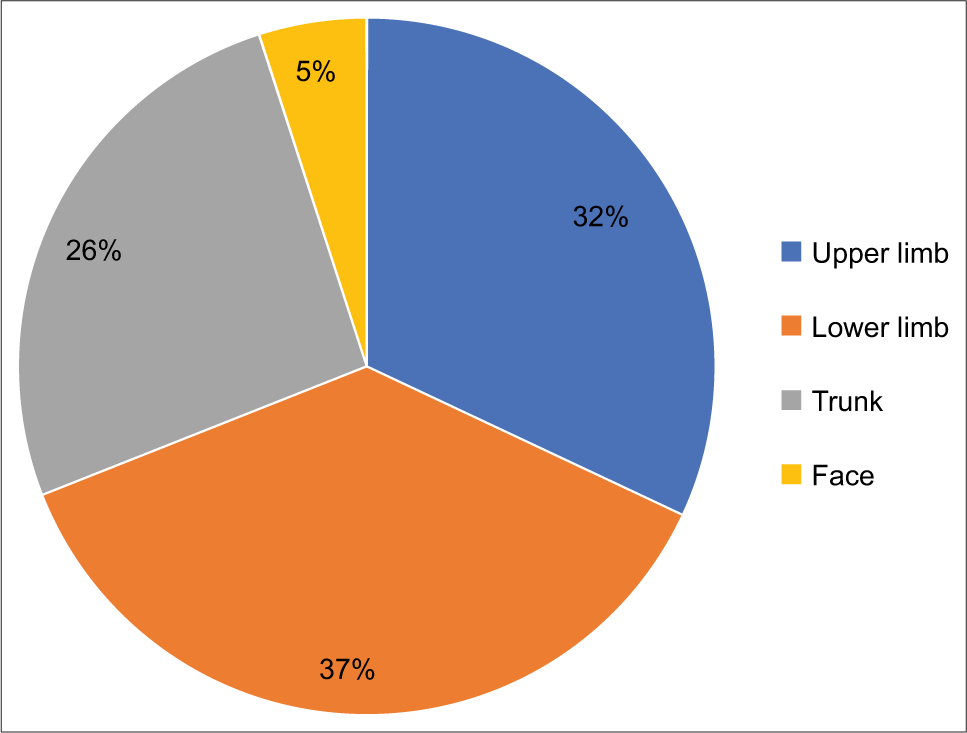
- Site of involvement of skin lesions.

- (a) Erythematous plaque on the tip of nose, pre-treatment; (b): Verrucous plaque on elbow, pre-treatment.
Histopathology revealed granulomatous inflammation [Figure 3] in all cases, with intra-cytoplasmic inclusion bodies in nine cases (56%). Tissue smear showed LD bodies in five patients (30%). Testing for Leishmania antibody with the rapid diagnostic kit – rK39 was negative in all cases.
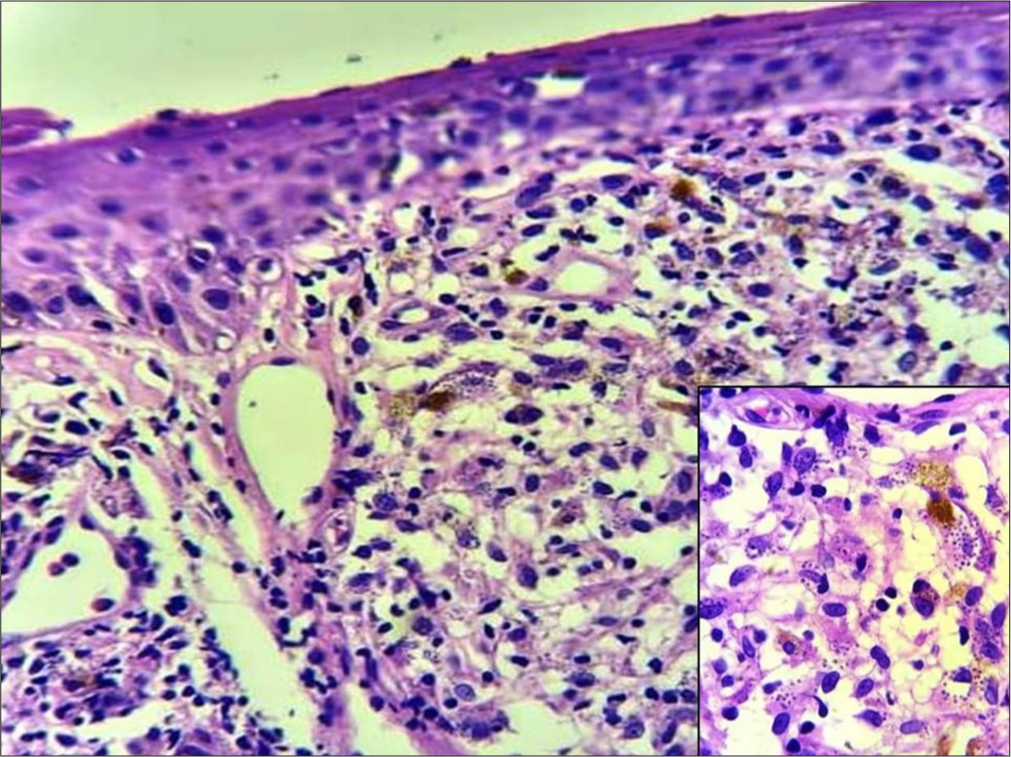
- Histopathology of skin biopsy from a nodule on the forearm shows atrophic epidermis and granulomatous inflammation in the dermis with numerous leishmania amastigotes (inset) in hematoxylin and eosin stain (×1000).
Seven patients were treated with oral fluconazole (6 mg/kg) for 4 weeks and liquid nitrogen cryotherapy (weekly three cycles). Two patients received oral itraconazole (100 mg bd for 4 weeks) and cryotherapy (3 cycles weekly), and the remaining seven patients received oral fluconazole for 4 weeks. All patients showed a reduction in the size of the lesion on follow-up. Patients treated with cryotherapy and fluconazole showed better response as observed by a faster reduction in the size of lesions [Figures 4a and b]. Entomology survey was conducted in the hostel and the colonies by the vector control unit of the district, and the vector Phlebotomus argentipes was identified from the colonies. The clinical details, laboratory findings, and treatment details of our patients are given in Table 1.

- (a) Erythematous plaque on the tip of nose post-treatment; (b): Verrucous plaque on elbow post-treatment.
| Sl No. | Age | Sex | Clinical presentation | Skin smear | HPR | PCR | RK39 | Treatment given | Response |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 13 | M | Nodule forearm | Negative | Granuloma with LD bodies | + | neg | Fluconazole+cryotherapy | Lesion reduced |
| 2 | 23 | M | Plaque ankle | Negative | Lymphocytes and LD bodies | + | neg | Fluconazole+cryotherapy | Lesion reduced |
| 3 | 20 | M | Plaque back | Positive | Granuloma with LD bodies | + | neg | Fluconazole+cryotherapy | Lesion reduced |
| 4 | 12 | F | Plaques leg and wrist | Negative | No LD bodies | + | neg | Fluconazole+cryotherapy | Lesion reduced |
| 5 | 13 | F | Nodule thigh | Negative | No LD bodies | + | neg | Fluconazole+cryotherapy | Lesion subsided |
| 6 | 13 | M | Nodule trunk | Negative | No LD bodies | + | neg | Fluconazole+cryotherapy | Lesion reduced |
| 7 | 23 | M | Plaque leg and chest | Negative | No LD bodies | + | neg | Itraconazole+cryotherapy | Lesion reduced |
| 8 | 12 | M | Plaque face | Negative | Granuloma and LD bodies | + | neg | Itraconazole+cryotherapy | Lesion reduced |
| 9 | 35 | F | Plaque forearm | Positive | Granuloma and LD bodies | + | neg | Fluconazole | Lesion reduced |
| 10 | 32 | F | Nodule arm | Positive | Granuloma and LD bodies | + | neg | Fluconazole | Lesion reduced |
| 11 | 15 | M | Plaque arm | Negative | Granuloma and LD bodies | + | neg | Fluconazole | Lesion reduced |
| 12 | 11 | F | Nodules body and leg | Negative | Granuloma seen No LD bodies |
+ | neg | Fluconazole | Lesion reduced |
| 13 | 11 | F | Nodule arm | Negative | Granuloma seen No LD bodies |
+ | neg | Fluconazole | Lesion reduced |
| 14 | 47 | F | Nodule leg | Negative | Granuloma seen No LD bodies |
+ | neg | Fluconazole | Lesion reduced |
| 15 | 20 | M | Nodule thigh | Positive | Granuloma and LD bodies | + | neg | Fluconazole | Lesion reduced |
| 16 | 10 | M | Nodule trunk | Positive | Granuloma and LD bodies | + | neg | Fluconazole | Lesion reduced |
PCR: polymerase chain reaction, LD: Leishmania donovani
DISCUSSION
CL caused by LD has been reported from many parts of India and Kerala.[3-5,8,9] The age of the affected in our series (10– 47 years) was lower than that noted in previous studies.[4,8]
This could be explained by the fact that most of our patients were identified from school surveys conducted. Fifteen out of the 16 cases belonged to the tribal population, which could be a reflection of the data collected from surveys in tribal schools and contact surveys of positive cases. It is possible that the delay in seeking treatment in many patients could be due to the asymptomatic nature of the disease. Two of the affected were siblings, which was consistent with a previous report from Sri Lanka.[10] All except three had lesions on limbs or face. The three patients with lesions on the trunk were men and this could be attributed to the clothing pattern of men in the area.[8] None had mucosal involvement, which was contrary to certain previous studies.[4,8] LD was identified as the causative organism in all patients consistent with literature from India and Sri Lanka.[4,8,10]
In our series, 15/16 cases were detected through a school survey and contact survey of positive cases. This suggests that the actual caseload in the community remains unknown, and most of the cases remain undetected. Moreover, the possibility of these lesions being misdiagnosed as leprosy lesions cannot be ruled out. One of the cases gave a history of being treated for multibacillary leprosy, which underscores the importance of histopathology in dermatological conditions. Active case finding by school surveys and contact surveys in areas reporting sporadic cases is essential for meeting the target of elimination of leishmaniasis in India.
The clinical lesions were erythematous and skin-colored nodules and plaques. None of them showed ulceration at the time of presentation. Erythematous papules were noted as the main type of lesion in other studies.[5] They also had ulcerated nodules, which are lacking in our cases. Noduloulcerative plaques were the main lesions reported in a study from Kashmir.[8]
Even though split-skin smear identified LD bodies in five cases, all cases showed chronic granulomatous inflammation and were positive for Leishmania bodies in eight cases. PCR was positive in all cases confirming the diagnosis. The species identification showed LD in all cases. This corroborates the findings of several studies which indicate LD as one of the major causative organisms in India and Sri Lanka.[4,5,9]
The various treatment modalities of CL are pentavalent antimony compounds (amphotericin B and miltefosine). Alternate drugs include ketoconazole, fluconazole, and itraconazole.[11] Physical modalities such as liquid nitrogen cryotherapy, heat therapy, and paramomycin ointment topically are also described.[12]
Our patients were treated with fluconazole and itraconazole for 6–8 weeks and topical ketoconazole/amphotericin B ointment. Seven patients received liquid nitrogen cryotherapy in 2 weekly intervals along with this. Patients treated with cryotherapy had better responses with good clearance of lesions. A study comparing fluconazole and cryotherapy with cryotherapy alone observed a reduction in the size of lesions more in patients who received fluconazole, even though it was not statistically significant.[13]
Limitations
Tribal areas are difficult to reach, and hence a more active search for cases among the tribal colonies was not possible due to the lack of resources; however, recommendations to the district health authorities have been made by the team. A small sample size of the study is also a limitation of our study.
CONCLUSION
CL cases still persist in certain pockets of the state. Undiagnosed cases may still persist in difficult-to-reach areas and marginalized populations due to their limited contact with the health system. Active search of cases and contact surveys should be strengthened among these population. This will help in detection of more cases, thereby controlling the disease, and to achieve and maintain the target of elimination.
Ethical approval
The research/study was approved by the Institutional Review Board at Government Medical College, Manjeri, number IEC/GMCM/131, dated May 18, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Leishmaniasis. The global health observatory. World Health Organization. Available from: https://www.who.int/data/gho/data/themes/topics/gho-ntdleishmaniasis [Last accessed on 2024 Oct 15]
- [Google Scholar]
- Two cases of cutaneous leishmaniasis seen in Trivandrum. Indian J Dermatol Venereol Leprol. 1988;54:161-2.
- [Google Scholar]
- Indigenous cutaneous leishmaniasis. Indian J Dermatol Venereol Leprol. 1990;56:228-9.
- [Google Scholar]
- Cutaneous leishmaniasis caused by Leishmania donovani in the tribal population of the agasthyamala biosphere reserve forest, Western Ghats, Kerala, India. J Med Microbiol. 2015;64:157-63.
- [CrossRef] [PubMed] [Google Scholar]
- Searching for cutaneous leishmaniasis in tribals from Kerala, India. J Glob Infect Dis. 2010;2:95-100.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous leishmaniasis: A 2022 updated narrative review into diagnosis and management developments. Am J Clin Dermatol. 2022;23:823-40.
- [CrossRef] [PubMed] [Google Scholar]
- Performance of rapid rk39 tests for the diagnosis of visceral leishmaniasis in Ethiopia: A systematic review and meta-analysis. BMC Infect Dis. 2021;21:1166.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and epidemiological study of cutaneous leishmaniasis in two tertiary care hospitals of Jammu and Kashmir: An emerging disease in North India. Int J Infect Dis. 2021;103:138-45.
- [CrossRef] [PubMed] [Google Scholar]
- Typical and atypical cutaneous leishmaniasis in Himachal Pradesh (India) Heliyon. 2021;7:e07282.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and epidemiological characteristics of cutaneous leishmaniasis in Sri Lanka. BMC Infect Dis. 2018;18:108.
- [CrossRef] [PubMed] [Google Scholar]
- Parasites - leishmaniasis- resources for health professionals. Available from: https://www.cdc.gov/parasites/leishmaniasis/health_professionals/index.html#tx [Last accessed on 2024 Oct 16]
- [Google Scholar]
- Diagnosis and treatment of leishmaniasis: Clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH) Am J Trop Med Hyg. 2017;96:24-45.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing the efficacy of fluconazole and cryotherapy versus cryotherapy alone on treating cutaneous leishmaniasis: A triple-blind randomized clinical trial. BMC Infect Dis. 2024;24:332.
- [CrossRef] [PubMed] [Google Scholar]






