Translate this page into:
Bilateral angiosarcoma: A rare occurrence
*Corresponding author: Divya Thomas, Department of Dermatology, Venereology and Leprosy, Government Medical College, Kottayam, Kerala, India. divyaanuthomas@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thomas D, Zacharia M, Ajithkumar K, Deepa S, Reshma C. Bilateral angiosarcoma: A rare occurrence. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_9_2025
Abstract
Angiosarcoma is a rare and aggressive neoplasm that originates from endothelial cells of lymphatic and blood vessels. It has high rates of metastasis and relapse. It shows a predilection for skin and other superficial soft tissues, with a predilection for the scalp or face. Here, we report an unusual presentation of bilateral and symmetrical angiosarcoma.
Keywords
Angiosarcoma
Cutaneous sarcoma
Idiopathic sarcoma
INTRODUCTION
Cutaneous sarcomas are rare entities accounting for only 5% of malignant skin tumors. Angiosarcomas are exceptionally uncommon as they constitute <1% of all sarcomas. These are malignant vasoformative neoplasms that arise in various tissues such as skin, breast, deep soft tissues, visceral organs, and bone in decreasing order of frequency.[1-3]
We report an extremely rare occurrence of bilateral angiosarcoma on the scalp and face.
CASE REPORT
A 66-year-old female presented with a well-defined unilateral reddish patch on the right side of her face for the past four months. Over the next five months, she developed a similar lesion on the left side also. The patient was initially managed as a case of topical steroid-damaged face given the diffuse telangiectasia and history of topical steroid application. Subsequently, the lesion extended to the scalp and developed ulceration. A plaque also developed subsequently.
On examination, there were two well-defined erythematous macules on both sides of the face. The lesion on the right side of the face extended into the neck and scalp with size 20 × 16 cm, with a plaque of 8 × 7 cm with central ulceration and hemorrhagic crusting superimposed on it. Multiple erythematous papules were present on the surface of the macule, mainly toward the lower part. The macule on the left side of the face had a size of 15 × 12 cm [Figure 1a and b]. Dermoscopy showed reddish areas suggestive of dilated blood vessels [Figure 2].

- (a): Well-defined erythematous macule on right side of the face, extending into neck and scalp with surface showing plaque of 8 × 7 cm with central ulceration and hemorrhagic crusting. Multiple erythematous papules on the surface of macule mainly toward lower part; (b): Left side of the face showing well-defined erythematous macule of 15 × 12 cm size.
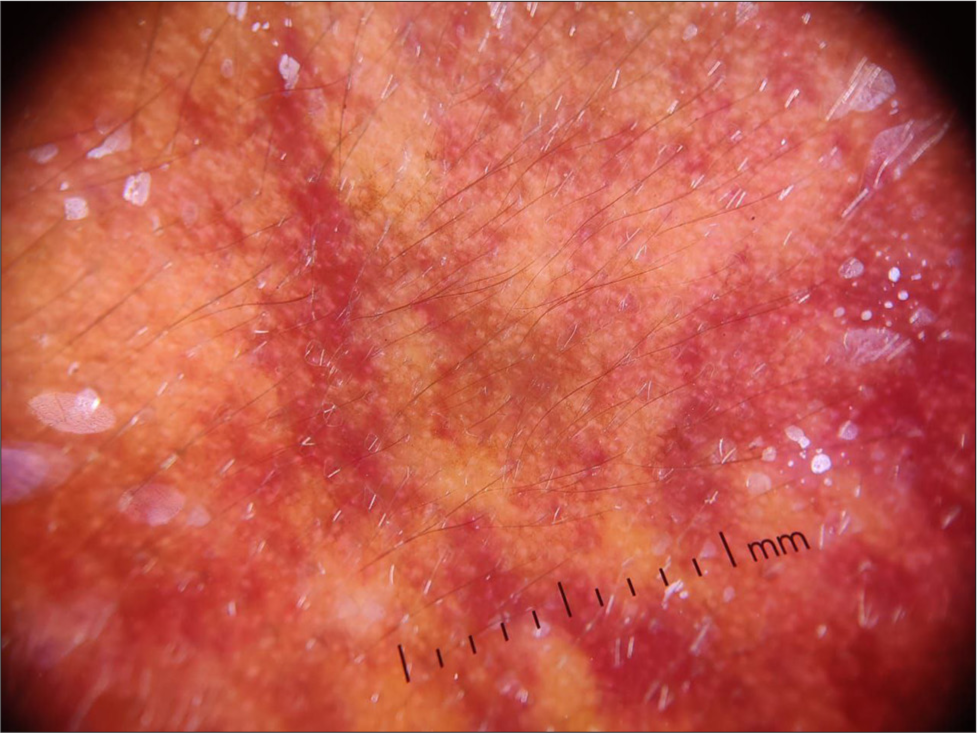
- Dermoscopy showing reddish areas suggestive of dilated blood vessels (DermLite DL4 dermoscope; ×10 magnification).
Histopathological examination from both lesions showed an ill-defined neoplasm composed of anastomosing vascular channels infiltrating through dermal collagen. Neoplastic cells showed pleomorphic nuclei with a hobnailing pattern and an increase in mitosis [Figure 3a and b]. Immunohistochemistry was positive for CD31 and CD34 and negative for human herpesvirus 8 [Figure 4a and b].
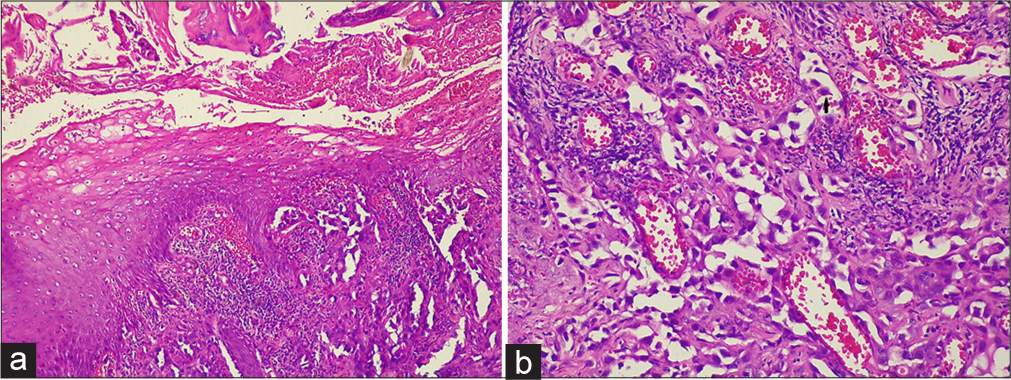
- (a): Ill-defined neoplasm of anastomosing vascular channels infiltrating through dermal collagen (H&E, x10); (b): Hobnail appearance (H&E, x40). H&E: Hematoxylin and eosin.
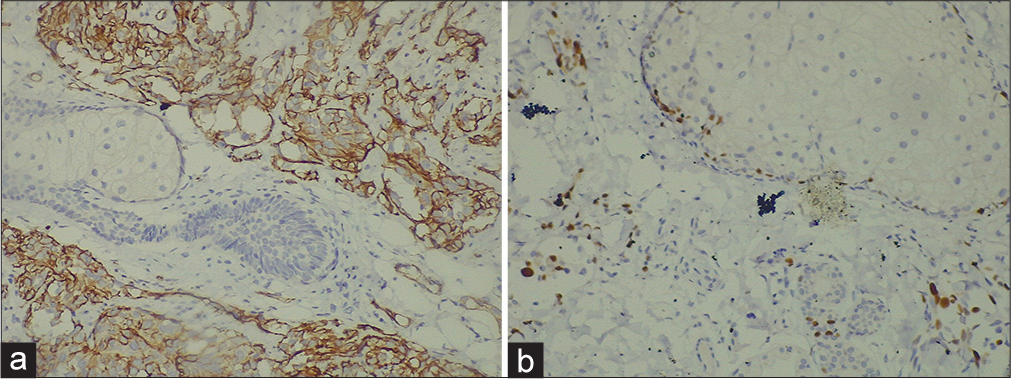
- (a): Immunohistochemistry (IHC) positive for CD31 (40×); (b): IHC positive for CD34 (40×).
DISCUSSION
Cutaneous angiosarcoma has three clinical variants as follows:
Primary cutaneous or idiopathic
Associated with chronic lymphedema (Stewart–Treves syndrome)
Radiation-induced
The most common form is idiopathic, which usually affects the scalp and face of the elderly, as in our case. Typical lesions are infiltrative and multifocal and can ulcerate and bleed. Men with Fitzpatrick skin type 1-3 are more commonly affected.[1,2] Stewart–Treves syndrome occurs predominantly in the upper limb of women, usually in 5-15 years following radical mastectomy with axillary lymphadenectomy. Immunosuppression and promotion of vascular oncogenesis are thought to be brought on by the buildup of serum proteins in lymphedema.[4,5] Post-radiation angiosarcoma is more common in women who underwent radiotherapy for treatment of carcinoma breast.[6]
Histopathological features range from irregular and anastomosed vascular channels in the most differentiated areas to solid sheets of epithelioid or spindle cells with a high degree of atypia, numerous mitoses, necrosis, and hemorrhage in less differentiated areas. Nuclear protrusion into the lumen and the pattern of dissecting proliferation between collagen bundles, as observed in our case, is characteristic.[2,7]
Typically, endothelial markers such as CD34 and vascular endothelial growth factor are expressed in angiosarcoma. CD31, von Willebrand factor, and Ulex europaeus I lectin, being more sensitive, are helpful in cases where there is minimal differentiation. In addition, lymphatic vessel markers such as Podoplanin are also expressed.[3,4,7]
Prognostic factors include age, extent of disease, primary site, tumor size, and histological grade.[1,3]
In a study of 434 cases of cutaneous angiosarcoma during 35 years (1973–2007), 62% of cases were seen in the head-and-neck region, whereas 24% arose on the trunk. Patients younger than 50 years had a 10-year relative survival rate of 71.7%, whereas 50 years or older had 36.8%. Angiosarcoma of the scalp and neck had a 10-year survival rate of 13.8%.[1]
Angiosarcomas in the head and neck have a worse prognosis due to the difficulty of excision with free margins.[1] Relapse and early metastasis are high in angiosarcoma. Patients with localized disease who undergo aggressive early surgery have a better chance of survival. Radiotherapy and chemotherapy are adjuncts to surgical treatment or palliative options for metastatic disease.[2-4] Our patient was referred to oncology for staging and treatment. However, she was lost to follow-up as she resorted to alternative medicine.
CONCLUSION
Angiosarcoma per se is a rare disease. The cases that have been reported to date have a unilateral distribution. Hence, our case is unique being bilateral in presentation.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr Ajithkumar K is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cutaneous angiosarcoma. Analysis of 434 cases from the surveillance, epidemiology, and end results program, 1973-2007. Ann Diagn Pathol. 2011;15:93-7.
- [CrossRef] [PubMed] [Google Scholar]
- Angiosarcoma: State of the art and perspectives. Crit Rev Oncol Hematol. 2011;80:257-63.
- [CrossRef] [PubMed] [Google Scholar]
- Stewart-Treves syndrome: Pathogenesis and management. J Am Acad Dermatol. 2012;67:1342-8.
- [CrossRef] [PubMed] [Google Scholar]
- Stewart-Treves syndrome of the lower extremity. J Clin Oncol. 2010;28:e351-2.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma as a delayed complication of radiation therapy for carcinoma of the breast. J Am Acad Dermatol. 2003;49:532-8.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant vascular tumors--an update. Mod Pathol. 2014;27:S30-8.
- [CrossRef] [PubMed] [Google Scholar]






