Translate this page into:
Silver in dermatology - From ancient use to modern innovations
*Corresponding author: Aravind Baskar Murthy, Department of Dermatology, Venereology and Leprosy, Sri Ramaswamy Memorial Medical College Hospital and Research Center, Chengalpet, Tamil Nadu, India. aravindbaskarmurthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Murthy A, Palaniappan V, Abirami C, Narasimhan M. Silver in dermatology - From ancient use to modern innovations. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_20_2025
Abstract
Silver, a metal known to mankind since early times, has gained the interest of researchers in recent times, exhibiting a growing trend in the use of silver in modern-day medicine. The biofilm-inhibiting and degrading effects of bioengineered silver nanoparticles have opened opportunities for future research in combating antimicrobial resistance. Silver has demonstrated a beneficial role in burns, wound healing, infections, papulosquamous disorders, and acne vulgaris. Silver has been used in cosmeceuticals, especially in deodorants, lipsticks, foundations, powders, and eyebrow pencils, owing to its antimicrobial and anti-inflammatory properties. The astringent and hemostatic properties of silver have also been utilized in skin care. Chronic exposure to silver causes its deposition in tissue referred to as ‘argyria’ which can be localized or generalized with a bluish-gray appearance due to the Tyndall effect. Allergic contact dermatitis has been reported due to contact with silver sulfadiazine, silver nitrate, and silver fulminate. Further research is needed to explore the promising avenues for silver in healthcare.
Keywords
Antimicrobial
Nanoparticle
Silver
Silver nanoparticles
INTRODUCTION
Silver has a significant role in medicine owing to its antibacterial and antiseptic properties. Although known to mankind since early times, the metal has gained the interest of researchers in recent times with a growing trend in the use of silver in modern-day medicine.[1] The popular forms of silver include silver nitrate, colloidal silver, and silver sulfadiazine (SSD).[1] The use of silver nanoparticles (AgNPs) has been preferred in recent times due to their exceptional antimicrobial activity even at low concentrations. Moreover, the rise of antibacterial resistance has opened the way to explore AgNPs as effective antimicrobial agent.[2]
HISTORY OF SILVER
The earliest use of silver was for safe water storage by the Greeks and Romans, while the first known therapeutic use of silver was in China in 1500 BC. The history of silver in medicine and dermatology is illustrated in Figure 1.[2,3]
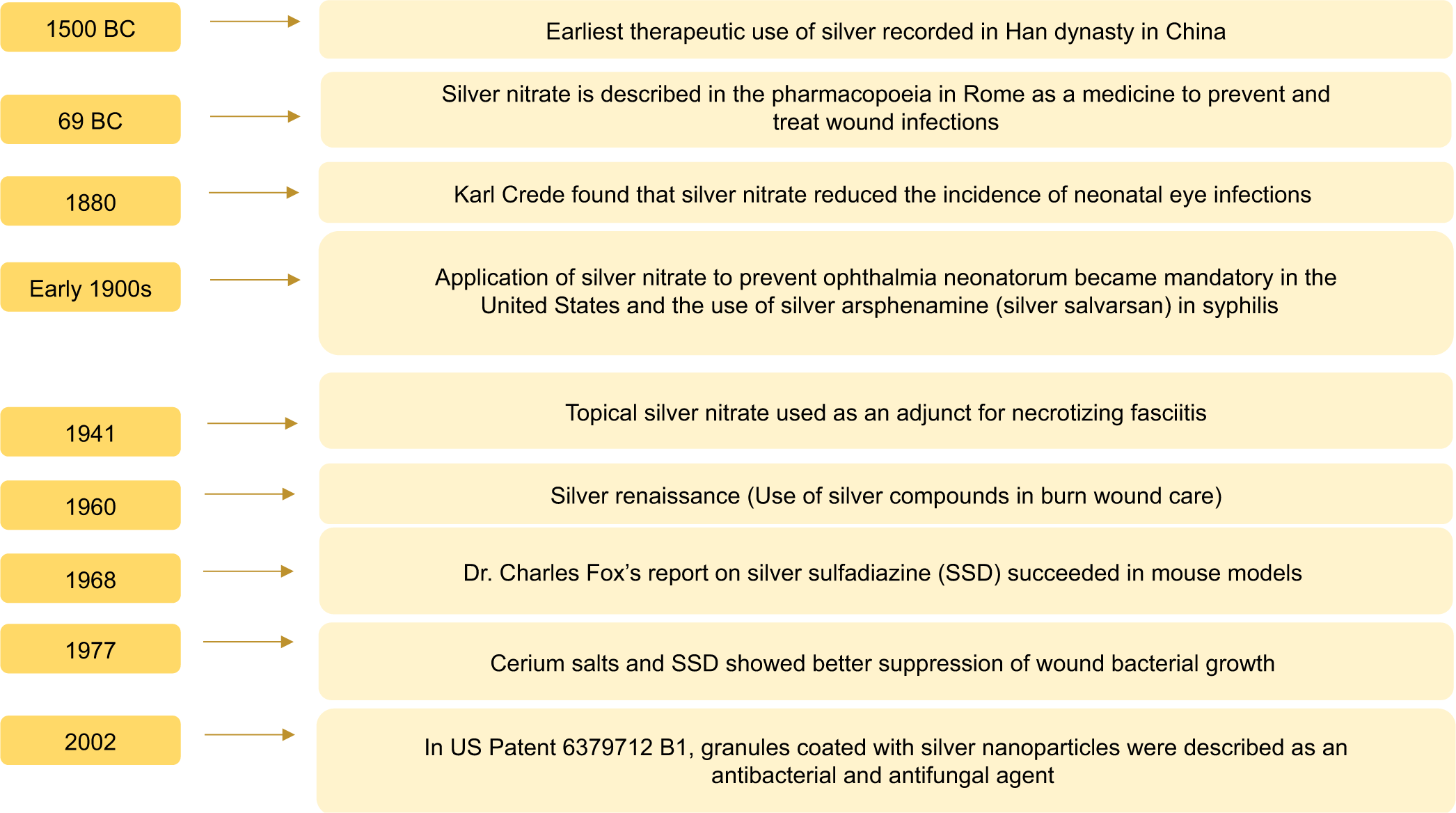
- Timeline of events in the history of silver in dermatology. BC: Before Christ.
USES OF SILVER IN DERMATOLOGY
Silver as an antimicrobial agent
The antimicrobial action of silver is directly proportional to the rate and the amount of silver being released, with the nature of the silver antimicrobial used being a pertinent factor in determining its efficacy.[4] The antimicrobial actions of silver are illustrated in Figure 2. A recent study has found synergistic activity of metal-metalloid-based antimicrobials (silver nitrate and potassium tellurite) with the advantage of combined bacteriostatic, bactericidal, and anti-biofilm activity.[5]
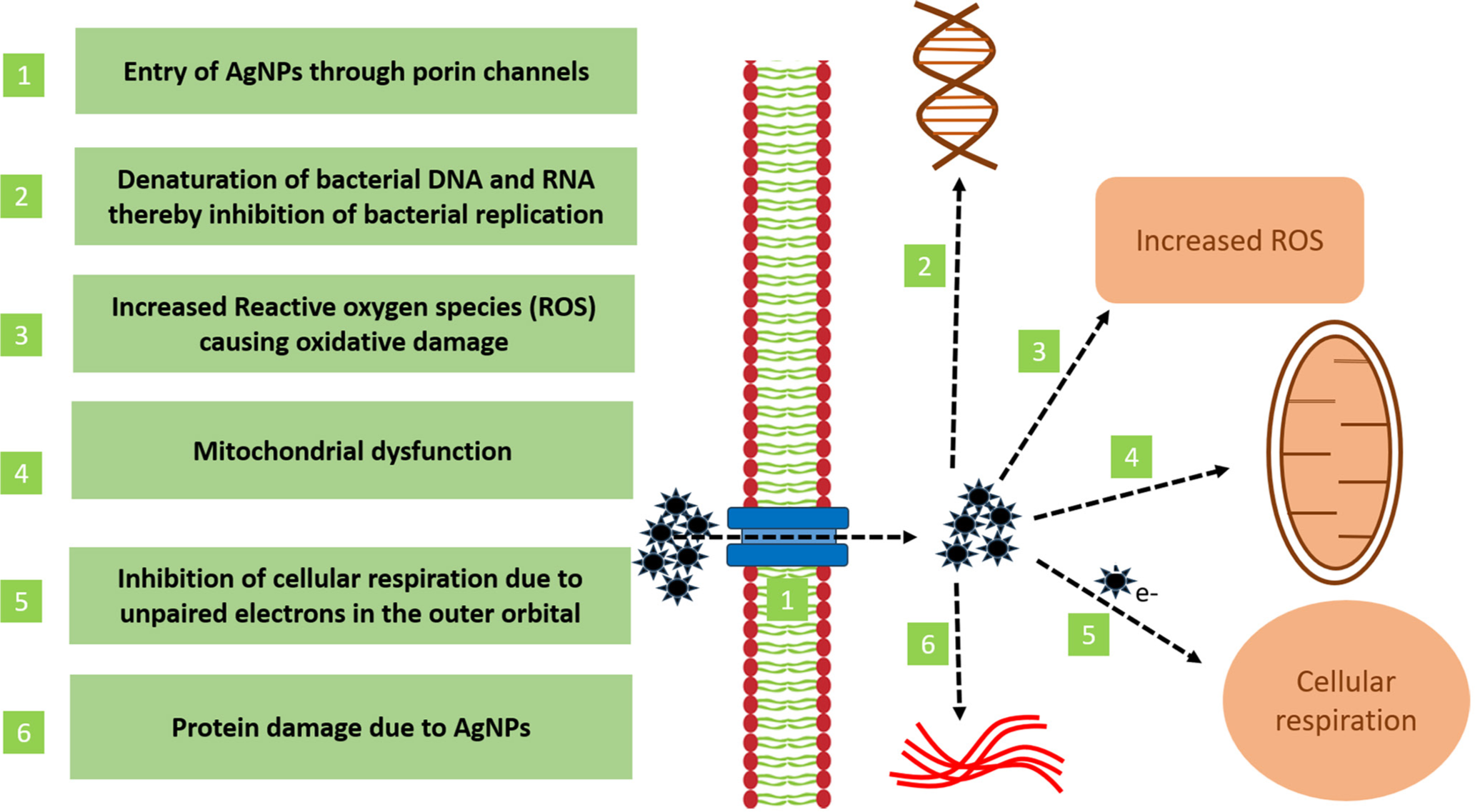
- Antimicrobial actions of silver. AgNPs: Silver nanoparticles, DNA: Deoxyribonucleic acid, RNA: Ribonucleic acid.
Evolution of AgNPs and its antimicrobial role
With the development of nanotechnology, metals are modulated to their nano size, altering their inherent physical, chemical, and optical properties. AgNPs are nanomaterials with sizes ranging from 1 to 100 nm in all dimensions, with a higher area-to-volume ratio than silver.[6] AgNPs have gained popularity, given the existing and emerging antibiotic resistance to various antibiotics.[6] According to the United States Centers for Disease Control, biofilms, 10-1000 times more resistant to antimicrobials than planktonic bacteria, are responsible for 80% of human bacterial infections.[7] AgNPs are synthesized by physical, chemical, and biological methods. The AgNPs bioengineered by microfabrication (Saccharomyces cerevisiae-derived AgNPs) and photofabrication (Pimpinella anisum-derived AgNPs) have shown significant antibacterial activity.[7,8] These bioengineered AgNPs have demonstrated antibiofilm activity against Escherichia coli, Staphylococcus aureus, Salmonella enterica, and Staphylococcus epidermis.[7] The characteristic features of nanoparticles, such as their size, shape, surface charge, and surface chemistry, affect their biological and pharmacological properties.[9] AgNPs have also documented efficacy against vancomycin-resistant bacteria and offer a broad spectrum of antibiotic coverage.[10]
Role of silver in specific infectious diseases
Uses of silver nitrate in viral infections
Silver nitrate is an effective caustic agent used to achieve hemostasis. Silver nitrate acts by causing coagulation of proteins, leading to tissue necrosis and eschar formation, eventually leading to thrombus formation and hemostasis.[11]The caustic property of silver nitrate has been used for various applications in dermatology, such as in warts and molluscum contagiosum.[11]
Warts
The self-limiting superficial penetration potential of silver nitrate makes it ideal for the treatment of warts, especially in patients with an increased risk of reduced tissue healing capacity. Silver nitrate (10%) is effective in the treatment of verruca vulgaris, causing 63.33% complete regression of lesions without significant side effects.[12] Verruca vulgaris treated with silver nitrate pencils has shown 43% complete resolution and 26% partial resolution.[13] The silver duct tape occlusion method has also been found to be effective in the management of plantar warts by creating a macerating and keratolytic environment, leading to stimulation of the immune response.[14] Silver nitrate application causes localized tissue irritation and immune reactions by the host against the virus, causing both biochemical and physical destruction.[15] Silver nitrate application to the periungual region causes gray-black staining and rarely gangrenous necrosis.[16]
Pox virus infections (Molluscum contagiosum [MC] and Monkeypox infections)
MC lesions responded well to 40% silver nitrate application, with 70% of lesions resolving in one application with a maximum of three applications needed for 97.7% resolution. Following application, the lesions become brown-black immediately, surrounded by an erythematous halo. Applying lignocaine jelly before the procedure prevents the erythematous flare, pruritus, and burning sensation.[17] A black crust forms before the MC lesion drops between days 10 and 14.[18] Silver nitrate paste has been tried successfully with 70% efficacy for MC to avoid unnecessary irritation caused by dripping of solution formulation onto the normal skin.[17]
In a study by Rogers et al., polysaccharide-coated AgNPs of size 10 nm and silver nitrate decreased monkeypox virus plaque formation by 60-79% and 29-40%, respectively.[19]
Herpes simplex virus (HSV) infection
A study by Pan et al., showed that AgNPs inhibited HSV-1 by reducing plaque formation, viral progeny production, and genomic load. AgNPs also interfere with HSV-1 messenger RNA expression and protein synthesis, alter the shape of viral particles, affect the virus’s entry, release, and cell-to-cell spread, and enhance the efficacy of acyclovir.[20] AgNPs in a concentration of 100 μg/mL have also been shown to inhibit HSV-2 replication in vitro completely.[21]
Human immunodeficiency virus (HIV)
AgNPs have demonstrated anti-HIV-1 activity by preventing CD4-dependent virion binding and fusion with a half-maximal inhibitory concentration between 0.44 and 0.91 mg/mL.[22] Silver ions, by themselves, exert lower efficiency in inhibiting HIV-1 infection in vitro than AgNPs. This is evident from a study that showed that the therapeutic index of silver salts such as silver nitrate and SSD in HIV-1 inhibition was 12 times lower than AgNPs.[22] It is also observed that the mutations in antiretroviral HIV strains conferring resistance were not found to affect the efficacy of AgNPs.[22] However, the efficacy of AgNPs in HIV needs further confirmation with human studies since the majority of data are based on in vitro studies.[22]
Silver and antifungal effect
AgNPs produced by the bioreduction of aqueous Ag+ ions by the leaf extract of Solanum trilobatum plant leaf have been found to have a higher inhibitory effect on Pityrosporum ovale. This effect has been proposed to enhance the efficacy of anti-dandruff shampoos. S. trilobatum-based AgNPs have also shown antifungal activity against Candida albicans and Candida parapsilosis.[23] Silver-zinc zeolite nanoparticles coated soft denture liners are beneficial in the prevention of oral candidiasis.[24] AgNPs have demonstrated anti-fungal activity against Microsporum canis, Trichophyton mentagrophytes, and Microsporum gypseum by creating pores in cell walls and plasma membranes and also against invasive mycosis like mucormycosis.[25,26] Recently, antifungal creams such as luliconazole and ketoconazole have been combined with AgNPs to combat superficial mycoses.[27,28] The various mechanisms by which AgNPs exhibit their antifungal effect are illustrated in Figure 3.[29]
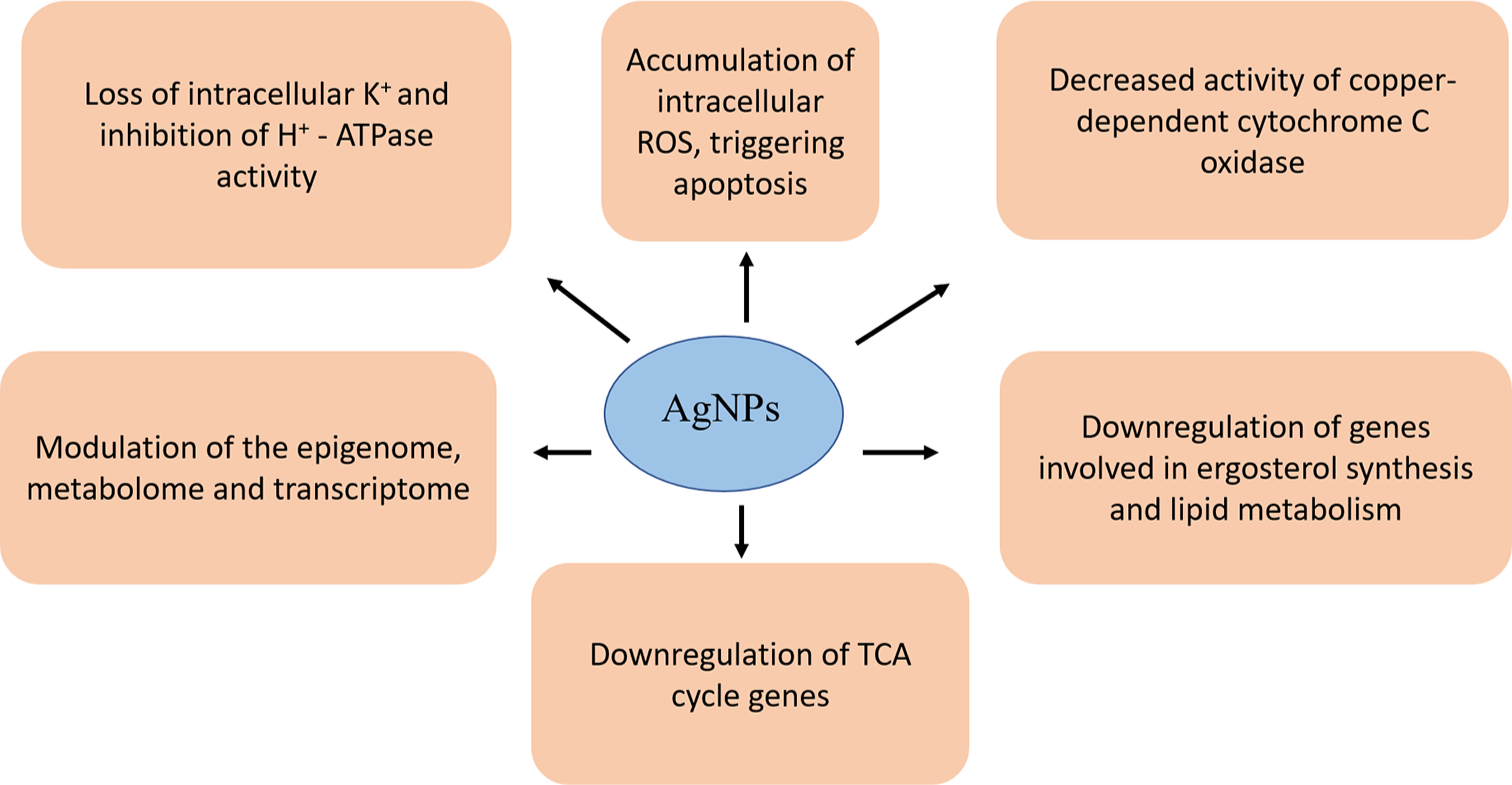
- Mechanism of antifungal action of silver nanoparticles. AgNPs: Silver nanoparticles, ROS: Reactive oxygen species, ATPase: Adenosine triphosphatase, K+: Potassium ion, H+: Hydrogen ion, C oxidase: Cytochrome C oxidase, TCA: Tricarboxylic acid.
Silver in parasitic infections
AgNP impairs the glycoprotein present on the surface of the parasite and can inhibit the proliferation of promastigotes, as demonstrated by Allahverdiyev et al., in Leishmania tropica. It was further studied that in the presence of increased ultraviolet light, AgNP further hampers amastigote endurance in the host cell.[30] Inhibitory action against Leishmania amazonensis has also been studied.[31]
Antimicrobial resistance to silver
Rampant use of silver-containing compounds has led to documented resistance of Ag to a few bacteria and fungi, especially in burn wards.[32] Significant mechanisms of resistance documented are due to the plasmid sil operon, copper-silver efflux systems, silver cation efflux proteins, and biofilm formation. The biofilm formation has been attributed to Bap1 and RbmA, and the binding of Ag+ ions with the negatively charged extracellular polymeric substances. Cross-resistance in bacteria (Serratia marcescens, Proteus mirabilis, Pseudomonas aeruginosa, Enterococcus durans, and Enterococcus gallinarum) has been noted between silver and other heavy metals such as mercury, arsenic, copper, tellurite, and zinc.[33]
Silver in burns and wound healing
Silver compounds have been exploited for their noteworthy role in the management of burns. The gold standard silver agent in the management of burns is SSD.[34] Silver nitrate (0.5%) is considered the standard and popular silver salt solution for burn wound therapy. On the contrary, the reduction of nitrate to nitrite can lead to oxidative cell damage, impairing re-epithelialization.[34]
The benefits of silver in wound healing can be attributed to various reasons, such as broad-spectrum antimicrobial activity, reduction in the activity of matrix metalloproteinase, combating biofilm formation, and its anti-inflammatory properties.[35,36] An ideal silver dressing maintains a sustained, therapeutic silver ion concentration (>30 ppm) while not causing local or systemic toxicity (≤60 ppm). The role of silver in wound healing is illustrated in Figure 4.
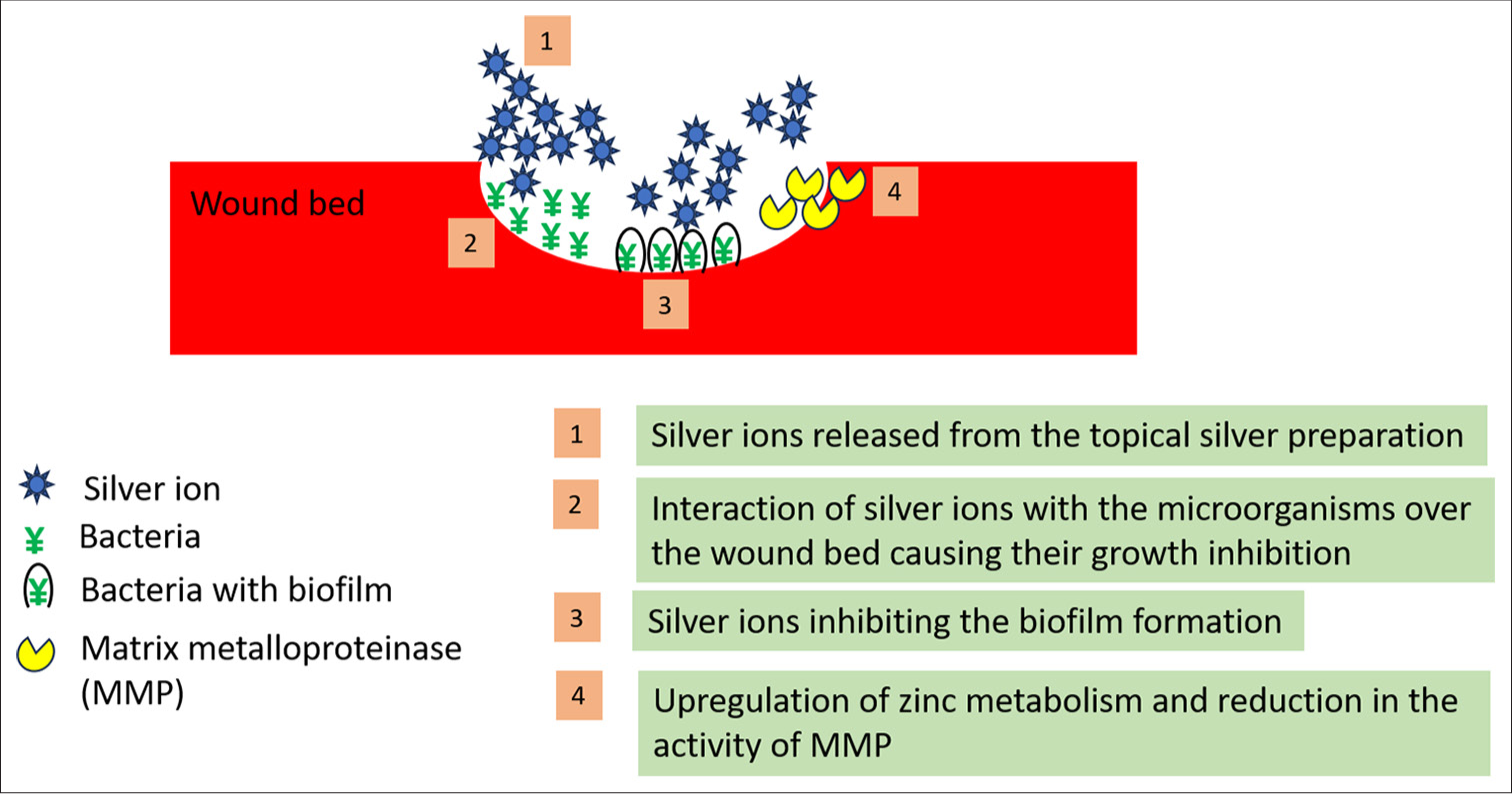
- Role of silver in wound healing.
The various forms of silver dressings used in wound care include SSD, silver-coated nylon, silver-coated polyethylene, silver-coated foam, silver-coated silicone, silver-coated cellulose hydrofiber, and silver-coated polyurethane (PU) sponge.[35] Silver-coated PU negative pressure wound therapy (NPWT) combines the benefit of NPWT and delivers an optimal concentration of silver that is below the toxic threshold to fibroblasts and keratinocytes.[35] The advantages of silver-containing dressings include less frequent change of dressing, reduced pain levels, and accelerated wound healing in contaminated wounds. Silver has no beneficial role in non-infected clean wounds as it can delay epithelialization.[35]
Dynamic reversible hydrogels have demonstrated a significant application in wound dressing. The use of SSD as a catalyst for the construction of hyaluronic acid-based hydrogels has enabled hydrogels to possess concurrent dynamics, stability, and antimicrobial properties.[37] Silver in dressings can be either in ionic form or metallic form (extremely small crystals or nanocrystals). The metallic silver needs to react with substances in the wound bed to form soluble salts such as silver nitrate, silver chloride, or silver oxide, releasing free silver ions.[36]
AgNP-loaded collagen chitosan dressing exerted significant biological effects on wound healing by regulation of growth and inflammatory factors (vascular endothelial growth factor [VEGF], basic fibroblast growth factor, transforming growth factor-beta 1, interleukin [IL]-1 beta, and epidermal growth factor-like domain 7).[38]
Silver in graft procedures
NPWT combined with AgNP sheets has shown better results in patients undergoing graft procedures in terms of better graft integration and decreased levels of systemic inflammatory markers.[39]
Silver as an astringent
Silver nitrate is used as an astringent in concentrations of 0.1-0.5% by drawing water out of the cells, causing dryness of exudative lesions. Hence, it is used in the management of leg ulcers and burns. Higher concentrations of silver nitrate are found to induce pain.[40]
Silver in hyperhidrosis and bromhidrosis
PU sheets, modified using hydrophilic polymers and coated with SSD, are used as cushion insoles in patients with plantar hyperhidrosis. Perspiration leads to the swelling of hydrophilic polymers on the PU surface, causing SSD release, which has bactericidal properties. Hence, silver prevents bad odor in bromhidrosis and bacterial infections in plantar hyperhidrosis.[41] In a randomized controlled trial by Celleno et al., an antiperspirant product based on silver citrate, aluminum hydrochloride, and agaricine showed beneficial antiperspirant and anti-bacterial activity with the added advantage of not staining the clothes.[42]
Silver as a hemostatic agent
Silver nitrate is an inexpensive, readily available topical hemostatic agent effective in concentrations of 10% applied with light pressure over the bleeding site after application.[43] Interaction of silver ions with proteins causes denaturation and precipitation of proteins and obstruction of small vessels. Silver nitrate application causes the formation of a thin eschar which prevents the formation of deep tissue necrosis.[44] Side effects of topical silver nitrate application include a burning sensation and temporary black discoloration.[44] However, application over large areas can cause permanent black discoloration due to silver particle impregnation. Inadvertent application of silver nitrate in large amounts can be neutralized by saline application.[43]
Silver in papulosquamous disorders
Silver in psoriasis
AgNPs complexed with Cornus mas modulate inflammation in psoriasis both at the molecular and cellular levels.[45] They have been found to reduce CD-68 positive macrophages, tumor necrosis factor (TNF), and IL-12 production in the psoriatic plaques, representing a novel “green” technology in modern psoriasis therapy. AgNPs resulted in reduced erythema, scaling, and plaque thickness with good long-term tolerability, devoid of treatment-related side effects.[45]
Bioengineered AgNPs coated textiles in atopic dermatitis
A combination of micro silver and nano lipid carriers (sNLC and NLC) has been used in the management of atopic dermatitis. The positive silver ions adsorb onto the negatively charged NLC to form sNLC, which adheres to the skin and bacterial surfaces, causing effective killing of the bacteria.[46] Bioengineered silver-based nanomaterial coatings have been used in cotton textiles, causing effective reduction of S. aureus colonization in patients with atopic dermatitis. The effect of AgNPs coated silver textiles starts 2 days after application and lasts for 1 week after removal of clothing.[47]
Silver in autoimmune bullous disorders
Topical nano colloidal silver is effective in the management of hard-to-heal ulcers of pemphigus vulgaris with a significant positive effect on the ulcer area and exudate.[48] Physiotulle silver dressings containing silver used in erosions of pemphigus vulgaris resulted in a significant reduction of pain score, reduced length of hospital stay, and reduced frequency of change of dressings.[49]
Silver in onychocryptosis
High-strength silver nitrate is beneficial in the management of hypergranulation tissue, complicating ingrown toenails in concentrations of 40%, 75%, and 90% through applicator sticks.[50]
Silver in umbilical granuloma
Umbilical granuloma, which presents with a pinkish to skin-colored granulomatous tissue, is the most documented umbilical abnormality in neonates. Careful application of silver nitrate 20% has been used once weekly over the lesion till resolution while protecting the surrounding area with petroleum jelly. Considering high rates of caustic burns and post-inflammatory pigmentation, other treatment modalities, such as the usage of common salt, electrocautery, cryotherapy, and topical steroids, are preferred.[51]
Silver in acne vulgaris
Acne vulgaris, due to its chronic and relapsing nature, demands long-term antibiotic use, resulting in antibiotic resistance demanding the use of alternative treatment options. With the use of AgNP gel on the rising trend, the combination of AgNP gel and 2.5% benzoyl peroxide is effective in both moderate inflammatory and non-inflammatory acne lesions.[52] A combination of AgNPs and extracts of Azadirachta indica (neem) leaves and Curcuma caesia rhizome has demonstrated good antibacterial activity against Propionibacterium acnes with a sustained drug release.[53,54]
Silver socks in epidermolysis bullosa
Silver-fibered cotton socks and silver vinyl insole material can be used for foot care in epidermolysis bullosa which has the advantages of reducing friction and heat, conducting heat away from the skin, and additional antibacterial action.[55]
Silver in cosmeceuticals
With the growing trend in the use of skincare and cosmetic products, consumers prefer safer products with long-term efficacy. This has led to the use of the term “cosmeceutical,” implying the overlap of cosmetics and pharmaceuticals. The cosmeceutical industry has integrated nanotechnology in the form of AgNPs in various products such as moisturizers, sunscreens, lipsticks, face cleansers, whitening creams, deodorants, toothpaste, and anti-aging products.[56] The combination of silver and gold nanoparticles to produce yellow-red pigment has been utilized in the production of various cosmetic products such as lipsticks, foundations, powders, and eyebrow pencils.[54]
Preference for silver as a nanoparticle in cosmeceuticals is attributed to its antimicrobial and anti-inflammatory properties.[56] The anti-inflammatory effects are due to disruption of the VEGF pathway, decrease in TNF-alpha and IL-6, inhibitory effect on nuclear factor-kB signaling, and inhibition of prostaglandin and cyclooxygenase synthesis.[56] Silver zeolite has been used as a deodorant in the axilla due to its strong and long-lasting bactericidal ability.[57] The uses of silver in dermatology, venereology, and leprosy have been summarized in Table 1.
| S. No. | Uses | Form of silver | |
|---|---|---|---|
| 1. | Antibacterial activity | ||
| Broad spectrum covering Staphylococcus aureus, Escherichia coli, Bacillus subtilis, Pseudomonas aeruginosa, and Salmonella Typhi | Silver nitrate, SSD, silver zeolite, silver-zinc zeolite nanoparticles, silver-tellurite, AgNPs | ||
| Leprosy | Gold-silver nanoparticle combination | ||
| Syphilis | Silver arsphenamine | ||
| Antiviral activity | |||
| Warts | Silver nitrate | ||
| Molluscum contagiosum | Silver nitrate | ||
| HSV infection | AgNPs | ||
| HIV infection | AgNPs | ||
| Antifungal activity | |||
| Candidiasis (Candida albicans, Candida parasilosis) | AgNPs | ||
| Pityrosporum folliculitis (Pityrosporum ovale) | |||
| Dermatophytosis (Trichophyton mentagrophytes, Microsporum gypseum) | |||
| Mucormycosis | |||
| Parasitic infections | |||
| Leishmaniasis | AgNPs | ||
| 2. | Wound healing including graft procedures | SSD, silver-coated nylon, silver-coated polyethylene, silver-coated foam, silver-coated silicone, silver-coated cellulose hydrofiber, and silver-coated polyurethane sponge | |
| 3. | As an astringent | Silver nitrate | |
| 4. | As a hemostatic agent | Silver nitrate | |
| 5. | Papulosquamous disorders | ||
| Psoriasis | AgNPs | ||
| Atopic dermatitis | Microsilver and nanolipid carrier Silver-coated cotton textiles |
||
| 6. | Acne vulgaris | AgNPs | |
| 7. | Autoimmune bullous disorders | Nano colloidal silver | |
| 8. | Miscellaneous | ||
| Umbilical granuloma | Silver nitrate | ||
| Epidermolysis bullosa | Silver-fibred cotton socks | ||
| Onychocryptosis | Silver nitrate | ||
| Use in cosmeceuticals | AgNPs and silver zeolite | ||
AgNPs: Silver nanoparticles, SSD: Silver sulfadiazine, HSV: Herpes simplex virus, HIV: Human immunodeficiency virus
Use of silver-coated instruments in dermatology
The antimicrobial properties of silver have been highly valued in varied medical applications through the silver coating of instruments. Ready-to-use medical instruments with instant antimicrobial effects have been devised, which activate bioactive silver coating upon package opening.[1] Invasive surgical tools, including medical needles, are coated with AgNPs with a particle diameter of 0.1-300 nm and silver concentration of 0.01-20% to prevent infection and provide pain relief. It was found that a silver concentration of <0.01% shows negligible antimicrobial effect, and more than 20% reduces the needle strength.[1]
Silver stains
Silver staining involves utilizing silver to selectively modify the appearance of a specific target in the microscopy of histological sections. The uses of silver stains in dermatology are mentioned in Table 2.[58-60]
| Category | Stain (s) | Structures demonstrated |
|---|---|---|
| Argentaffin-silver reduction | Fontana-Masson | Argentaffin tumors, melanomas, and some carcinoid tumors |
| Argyrophil-absorption | ||
| Acidic | Warthin-Starry, Dieterle, Steiner and Steiner | Spirochetes and other bacteria |
| Acid melanin stain | Melanomas | |
| Basic | Grimelius | Neuroendocrine secretory granules |
| Neutral | AgNOR stain | Nucleolar organizer region |
| Argyrophil-impregnation | ||
| Type I | Bodian, Bielschowsky | Neurites |
| Type II | Golgi | Neurites |
| Argyrophil-oxidation-reduction | Grocott’s Modified Gomori Methenamine silver stain | Fungi |
| Jones stain | Basement membranes | |
| Reticulum stain | Reticular fibers | |
Silver in Raman spectroscopy
Raman spectroscopy has been used recently to diagnose skin diseases, especially skin tumors such as basal cell carcinoma and melanoma, based on autofluorescence. AgNPs with unique optical properties of strong absorption and scattering of light have made them useful in surface-enhanced Raman spectroscopy.[8]
SIDE EFFECTS OF SILVER
Argyria
The term “argyria” derived from the Greek word argyros, meaning silver, was coined by Fuchs in 1840. It is an uncommon benign condition characterized by chronic exposure and the deposition of silver in the tissue.[61,62] Argyria can be localized or generalized based on the mode and quantity of silver absorbed.[62] The commonly characterized forms of localized argyrias are (i) cutaneous, (ii) oral cavity, and (iii) ocular. A few unusual localized argyrias are penis, vagina, urinary tract, nasal mucosa, and trachea.[61,62]
Generalized argyrias occur due to systemic absorption of silver that gets widely deposited in the skin, nails, eyes, and mucous membranes.[61] As alternative medicine gains popularity, the availability of silver-containing solutions increases, consequently raising the incidence of argyria. This trend is particularly noticeable in Asia, where there is a growing number of case reports documenting instances of argyria.[63] Exceeding the daily oral exposure of 5 μg/kg/day of silver exposes the patients to risks of skin discoloration.[64]
Apart from cutaneous deposition of silver, systemic side effects such as renal toxicity, leukopenia, and cytotoxicity have also been reported, especially through SSD dressings in burns involving >40% of body surface area.[34]
Localized argyrias occur due to the impregnation of silver confined to the site of direct contact, especially in professions such as silversmithing and industries involving photography, soldering, batteries, and mirrors. Dental procedures, including those involving amalgam tattooing, as well as the use of silver jewelry such as earrings and nasal piercings, have also been linked to localized argyria.[65] The presence of the Tyndall effect causes the brown colloidal silver particles located in the dermis to give off a bluish-gray appearance when observed through the skin.[66] The differential diagnoses of argyria are mentioned in Table 3.
| S. No. | Differential diagnosis | S. No. | Differential diagnosis |
|---|---|---|---|
| 1. | Metals deposition
|
4. | Nutritional deficiencies
|
| 2. | Drug deposition
|
5. | Endocrine disorders
|
| 3. | Metabolic conditions
|
6. | Dermatological conditions
|
Histologically, yellow-brown colored collagen bundles resembling pseudo-ochronosis have been described occasionally.[61] Management options include sunscreens, 1064 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser, 755 nm alexandrite laser, and low-fluence Q-switched Nd:YAG laser and avoidance of offending silver-containing agents.[63,67]
Silver as an allergen
Most of the cases of allergic contact dermatitis (ACD) to silver seem to be related to occupation, such as jewelers, photographers, and silver miners.[68] ACD has been reported to be silver sulfadiazine, silver nitrate, or silver fulminate.[69] The side effects of topical silver preparations include stinging, pain, redness, chemical burns, and post-inflammatory pigmentation.[70] The widespread erythema with irritant contact dermatitis is seen especially in atopic individuals and in clustered lesions over the intertriginous areas.[17]
CONCLUSION
Silver is a historic metal with diverse applications in dermatology and various fields of medicine. Silver has demonstrated its efficacy and versatility, from infection control and wound healing to its advancing role in skincare. The antibacterial and biofilm inhibitory effects of silver and AgNPs have a greater role to play in the future, especially in this era of growing antimicrobial resistance. Further research is needed to explore the possible promising avenues for silver in healthcare.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Antimicrobial silver in medicinal and consumer applications: A patent review of the past decade (2007-2017) Antibiotics (Basel). 2018;7:93.
- [CrossRef] [PubMed] [Google Scholar]
- Antibacterial activity of silver and its application in dentistry, cardiology and dermatology. Microorganisms. 2020;8:1400.
- [CrossRef] [PubMed] [Google Scholar]
- Silver in medicine: A brief history BC 335 to present. Burns. 2014;40(Suppl 1):S3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Silver in health care: Antimicrobial effects and safety in use. Curr Probl Dermatol. 2006;33:17-34.
- [CrossRef] [PubMed] [Google Scholar]
- Insights into the synergistic antibacterial activity of silver nitrate with potassium tellurite against Pseudomonas aeruginosa. Microbiol Spectr. 2023;11:e0062823.
- [CrossRef] [PubMed] [Google Scholar]
- Silver nanoparticles and their antibacterial applications. Int J Mol Sci. 2021;22:7202.
- [CrossRef] [PubMed] [Google Scholar]
- Bioinspired green-synthesized silver nanoparticles: In vitro physicochemical, antibacterial, biofilm inhibitory, genotoxicity, antidiabetic, antioxidant, and anticoagulant performance. Mater Adv. 2023;4:3037-54.
- [CrossRef] [Google Scholar]
- Exploring the biological properties of Saccharomyces cerevisiaederived silver nanoparticles: In vitro structural characteristics, antibacterial, biofilm inhibition and biofilm degradation, antioxidant, anticoagulant, thrombolytic, and antidiabetic performance. Inorg Chem Commun. 2024;162:112291.
- [CrossRef] [Google Scholar]
- Chapter 5 - Green nanotechnology: Isolation of bioactive molecules and modified approach of biosynthesis In: Patra C, Ahmad I, Ayaz M, Khalil AT, Mukherjee S, Ovais M, eds. Biogenic nanoparticles for cancer theranostics. Netherlands: Elsevier; 2021. p. :101-22. Available from: https://www.sciencedirect.com/science/article/pii/B9780128214671000057 [Last accessed on 2024 Oct 27].
- [CrossRef] [Google Scholar]
- Applications of gold and silver nanoparticles in theranostics. Appl Biochem Biotechnol. 2022;194:4187-219.
- [CrossRef] [PubMed] [Google Scholar]
- Achieving hemostasis in dermatology-Part II: Topical hemostatic agents. Indian Dermatol Online J. 2013;4:172-6.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of 10% silver nitrate solution in the treatment of common warts: A placebo-controlled, randomized, clinical trial. Int J Dermatol. 2007;46:215-7.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of silver nitrate pencils in the treatment of common warts. J Dermatol. 1994;21:329-33.
- [CrossRef] [PubMed] [Google Scholar]
- Silver duct tape occlusion in treatment of plantar warts in adults: Is it effective? Dermatol Ther. 2020;33:e13342.
- [CrossRef] [Google Scholar]
- A randomized comparative evaluation of clinical and home application to investigate the effectiveness of silver nitrate (AgNO(3)) (95%) for the treatment of verruca pedis. Int J Pharm Pract. 2017;25:421-8.
- [CrossRef] [PubMed] [Google Scholar]
- Silver nitrate staining of the fingernails. J Cutan Med Surg. 2017;21:443-4.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of molluscum contagiosum with silver nitrate paste. Pediatr Dermatol. 1999;16:395-7.
- [CrossRef] [PubMed] [Google Scholar]
- Molluscum contagiosum: Review and update on management. Pediatr Dermatol. 2017;34:504-15.
- [CrossRef] [PubMed] [Google Scholar]
- A Preliminary assessment of silver nanoparticle inhibition of monkeypox virus plaque formation. Nanoscale Res Lett. 2008;3:129.
- [CrossRef] [Google Scholar]
- Inhibitory activity and mechanism of silver nanoparticles against herpes simplex virus type 1. Arch Virol. 2022;167:1619-36.
- [CrossRef] [Google Scholar]
- Inhibition effect of silver nanoparticles on herpes simplex virus 2. Genet Mol Res. 2014;13:7022-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mode of antiviral action of silver nanoparticles against HIV-1. J Nanobiotechnology. 2010;8:1.
- [CrossRef] [PubMed] [Google Scholar]
- Enhancement of antidandruff activity of shampoo by biosynthesized silver nanoparticles from Solanum trilobatum plant leaf. Appl Nanosci. 2012;3:431-9.
- [CrossRef] [Google Scholar]
- Long term antifungal efficacy of silver-zinc zeolite nanoparticles incorporated in two soft denture liners-An in vitro assessment. Dent Res J (Isfahan). 2022;19:12.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of antifungal effect of silver nanoparticles against Microsporum canis, Trichophyton mentagrophytes and Microsporum gypseum. Iran J Biotechnol. 2015;13:38-42.
- [CrossRef] [PubMed] [Google Scholar]
- Antifungal activity of silver nanoparticles on fungal isolates from patients of suspected mucormycosis. Int Microbiol. 2023;26:143-7.
- [CrossRef] [PubMed] [Google Scholar]
- Preparation of luliconazole loaded silver nanoparticles topical gel. J Drug Deliv Ther. 2022;12:31-5.
- [CrossRef] [Google Scholar]
- Antifungal activity of silver nanoparticles in combination with ketoconazole against Malassezia furfur. AMB Express. 2019;9:131.
- [CrossRef] [PubMed] [Google Scholar]
- Biogenic silver nanoparticles as antifungal agents. Front Chem. 2022;10:1023542.
- [CrossRef] [PubMed] [Google Scholar]
- Antileishmanial effect of silver nanoparticles and their enhanced antiparasitic activity under ultraviolet light. Int J Nanomedicine. 2011;6:2705-14.
- [CrossRef] [PubMed] [Google Scholar]
- Green synthesis of antileishmanial and antifungal silver nanoparticles using corn cob Xylan as a reducing and stabilizing agent. Biomolecules. 2020;10:1235.
- [CrossRef] [PubMed] [Google Scholar]
- The increasing threat of silver-resistance in clinical isolates from wounds and burns. Infect Drug Resist. 2019;12:1985-2001.
- [CrossRef] [PubMed] [Google Scholar]
- Microbial silver resistance mechanisms: Recent developments. World J Microbiol Biotechnol. 2022;38:158.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of silver on burn wound infection control and healing: review of the literature. Burns. 2007;33:139-48.
- [CrossRef] [PubMed] [Google Scholar]
- Silver in wound care-friend or foe?: A comprehensive review. Plast Reconstr Surg Glob Open. 2019;7:e2390.
- [CrossRef] [PubMed] [Google Scholar]
- The role of silver in wound healing. Br J Nurs. 2005;14:S22-S24. S26 passim
- [CrossRef] [PubMed] [Google Scholar]
- One stone three birds: Silver sulfadiazine modulates the stability and dynamics of hydrogels for infected wound healing. Adv Healthc Mater. 2024;13:e2400242.
- [CrossRef] [PubMed] [Google Scholar]
- Characterization and biological evaluation of a novel silver nanoparticle-loaded collagen-chitosan dressing. Regen Biomater. 2020;7:371-80.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring an innovative approach: Integrating negative-pressure wound therapy with silver nanoparticle dressings in skin graft procedures. J Pers Med. 2024;14:206.
- [CrossRef] [PubMed] [Google Scholar]
- Principles of topical therapy In: Griffiths CE, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook's textbook of dermatology (9th ed). United Kingdom: Wiley Blackwell; 2016. p. :361-99.
- [Google Scholar]
- Surface modified and medicated polyurethane materials capable of controlling microorganisms causing foot skin infection in athletes. Colloids Surf B Biointerfaces. 2013;102:139-45.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical evaluation of an antiperspirant for hyperhidrosis. G Ital Dermatol Venereol. 2019;154:338-41.
- [CrossRef] [PubMed] [Google Scholar]
- Topical hemostatic agents: A review. Dermatol Surg. 2008;34:431-45.
- [CrossRef] [PubMed] [Google Scholar]
- Topical hemostatic agents In: Consultative hemostasis and thrombosis. Netherlands: Elsevier; 2013. p. :538-45. Available from: https://linkinghub.elsevier.com/retrieve/pii/B9781455722969000294 [Last accessed on 2022 Sep 13].
- [CrossRef] [Google Scholar]
- Topical silver and gold nanoparticles complexed with Cornus mas suppress inflammation in human psoriasis plaques by inhibiting NF-kB activity. Exp Dermatol. 2018;27:1166-9.
- [CrossRef] [PubMed] [Google Scholar]
- A new concept for the treatment of atopic dermatitis: Silver-nanolipid complex (sNLC) Int J Pharm. 2014;462:44-51.
- [CrossRef] [PubMed] [Google Scholar]
- Silver-coated textiles in the therapy of atopic eczema. Curr Probl Dermatol. 2006;33:152-64.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of topical nanocolloidal silver formulation use with eosin 2% solution in management of hard-to-heal ulcers in patients with pemphigus vulgaris. J Wound Care. 2020;29:664-8.
- [CrossRef] [PubMed] [Google Scholar]
- A preliminary clinical trial comparing wet silver dressings versus wet-to-dry povidone-iodine dressings for wound healing in pemphigus vulgaris patients. Dermatol Ther. 2021;34:e14906.
- [CrossRef] [Google Scholar]
- The use of silver nitrate (AgNO3) as a caustic agent for the treatment of hypergranulation tissue affecting ingrown toenails: A scoping review. J Int Foot Ankle Found. 2023;2:1-8.
- [Google Scholar]
- Treatment with silver nitrate versus topical steroid treatment for umbilical granuloma: A non-inferiority randomized control trial. PLoS One. 2018;13:e0192688.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative trial of silver nanoparticle gel and 1% clindamycin gel when use in combination with 2.5% benzoyl peroxide in patients with moderate acne vulgaris. J Med Assoc Thai. 2017;100:78-85.
- [Google Scholar]
- Nano-therapeutics to treat acne vulgaris. Indian J Microbiol. 2022;62:167-74.
- [CrossRef] [PubMed] [Google Scholar]
- Safety of the application of nanosilver and nanogold in topical cosmetic preparations. Colloids Surf B Biointerfaces. 2019;183:110416.
- [CrossRef] [PubMed] [Google Scholar]
- Foot care in epidermolysis bullosa: Evidence-based guideline. Br J Dermatol. 2020;182:593-604.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of silver nanoparticles in cosmeceutical and potential biosafety complications. Saudi J Biol Sci. 2022;29:2085-94.
- [CrossRef] [PubMed] [Google Scholar]
- New antiaxillary odour deodorant made with antimicrobial Ag-zeolite (silver-exchanged zeolite) Int J Cosmet Sci. 2006;28:299-309.
- [CrossRef] [PubMed] [Google Scholar]
- Histologic stains in dermatopathology. J Am Acad Dermatol. 1990;22:820-30.
- [CrossRef] [PubMed] [Google Scholar]
- Histological stains in the past, present, and future. Cureus. 2021;13:e18486.
- [CrossRef] [PubMed] [Google Scholar]
- PAS and GMS utility in dermatopathology: Review of the current medical literature. J Cutan Pathol. 2020;47:1096-102.
- [CrossRef] [PubMed] [Google Scholar]
- Argyria an unrecognized cause of cutaneous pigmentation in Indian patients: A case series and review of the literature. Indian J Dermatol Venereol Leprol. 2013;79:805-11.
- [CrossRef] [PubMed] [Google Scholar]
- Localized cutaneous argyria: Review of a rare clinical mimicker of melanocytic lesions. Ann Diagn Pathol. 2021;54:151776.
- [CrossRef] [PubMed] [Google Scholar]
- "Silver man" argyria of the skin after ingestion of a colloidal silver solution. J Dtsch Dermatol Ges. 2015;13:1030-2.
- [CrossRef] [Google Scholar]
- Argyria, an unexpected case of skin discoloration from colloidal silver salt ingestion. J Emerg Med. 2020;59:e39-41.
- [CrossRef] [PubMed] [Google Scholar]
- Localized cutaneous argyria: Two case reports and clinicopathologic review. Am J Dermatopathol. 2013;35:e115-8.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative near infrared spectroscopic analysis of Q-Switched Nd:YAG treatment of generalized argyria. Lasers Surg Med. 2013;45:15-21.
- [CrossRef] [PubMed] [Google Scholar]
- Effective laser treatment options for argyria: Review of literatures. J Cosmet Dermatol. 2020;19:1877-82.
- [CrossRef] [PubMed] [Google Scholar]
- Silver-resistance, allergy, and blue skin: Truth or urban legend? Burns. 2014;40(Suppl 1):S19-23.
- [CrossRef] [PubMed] [Google Scholar]
- Silver: An underdiagnosed allergen? Contact Dermatitis. 2021;84:464-6.
- [CrossRef] [PubMed] [Google Scholar]
- Update on the treatment of molluscum contagiosum in children. Actas Dermosifiliogr (Engl Ed). 2018;109:408-15.
- [CrossRef] [PubMed] [Google Scholar]







