Translate this page into:
A rare case report of Maffucci syndrome in a 16-year-old girl
*Corresponding author: Shivani Ranjan, Department of Dermatology, Government Medical College, Jammu, Jammu and Kashmir, India. drshivaniranjan@rocketmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhary R, Ranjan S. A rare case report of Maffucci syndrome in a 16-year-old girl. J Skin Sex Transm Dis. 2024;6:196-9. doi: 10.25259/JSSTD_12_2024
Abstract
Maffucci syndrome is an extremely rare, sporadic disorder that primarily affects bone and skin. It is characterized by multiple enchondromas, especially in the bones of hands and feet, with cutaneous hemangiomas. Treatment consists of orthopedic and surgical intervention to minimize deformities and for cosmetic purposes. Careful surveillance for both skeletal and non-skeletal malignancies is needed. We report here a case of Maffucci syndrome in a 16-year-old girl.
Keywords
Maffucci
Syndrome
Hemangioma
Enchondroma
INTRODUCTION
First described by Angelo Maffucci in 1881, Maffucci syndrome is a rare disorder with the involvement of bone and skin. Fewer than 200 cases reported till date.[1] It presents with multiple enchondromas and vascular tumors. This syndrome occurs sporadically without any familial, sexual or racial predilection. 25% of cases manifest at 4-5 years of age, 45% before 6 years of age, and 78% of cases develop before puberty.[2] The risk of malignant transformation is higher in chondromatous lesions as compared to hemangiomas.[3]
CASE REPORT
A 16-year-old female born out of non-consanguineous marriage presented to the outpatient department with multiple bony swellings over the right hand for seven years and multiple asymptomatic soft swellings on her right hand and left foot for seven years and pain in her right hand for seven to eight months. These swellings were initially small and gradually increased in size and number. There were no similar complaints in the family. On examination, multiple hard, non-tender bony swellings were present over the 3rd, 4th, and 5th digits of the right hand [Figure 1], and multiple firm, mildly tender, slightly compressible nodules with a bluish hue were present over the ulnar border of the right hand and medial border of the left foot [Figure 2a and b]. Nodules were variable in size and shape. Lesions over the hand had a smooth surface, while lesions over the foot were hyperpigmented and rough. No limb length discrepancy was observed. There was no mucosal or nail involvement. Systemic examination showed no abnormality. Routine investigations such as complete blood count, liver function test, kidney function tests, urine routine, and stool for occult blood were normal. X-ray chest and ultrasound abdomen and pelvis were normal. X-ray of the right hand revealed multiple well-defined expansile lytic lesions involving metaphysis of the 4th metacarpal, 3rd and 4th proximal phalanges, and epiphysis of the 5th metacarpal and proximal phalanx. The lesions show a type 1a margin with a narrow zone of transition. Internal linear and round radiopaque foci are seen, consistent with the chondroid internal matrix. Features were suggestive of multiple enchondromas [Figure 3]. No fractures were noted. Histopathological examination of firm nodules present over the right hand revealed dilated vascular spaces in the dermis lined by a single layer of endothelium containing red blood cells. Dermoscopic findings of hemangioma over the left foot are shown in Figure 4. Based on clinical, histopathological, and dermoscopic examination, a diagnosis of Maffucci syndrome was made. The patient was explained about the prognosis and course of the disease, and was kept under regular follow-up for early detection of malignant transformation.

- Enchondromas present over the 3rd, 4th, 5th digits of the right hand.
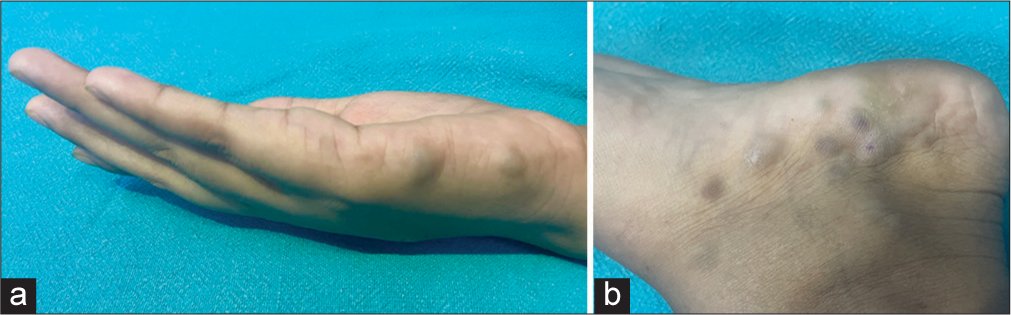
- (a): Hemangiomas present over the ulnar border of the right hand; (b): Hemangiomas present over the medial border of the left foot.

- X-ray of the right hand AP and lateral shows multiple well-defined expansile lytic lesions involving metaphysis of 4th metacarpal, 3rd and 4th proximal phalanges, epiphysis of 5th metacarpal and proximal phalanx. The lesions show type 1a margin with narrow zone of transition. Internal linear and round radiopaque foci are seen, consistent with chondroid internal matrix.
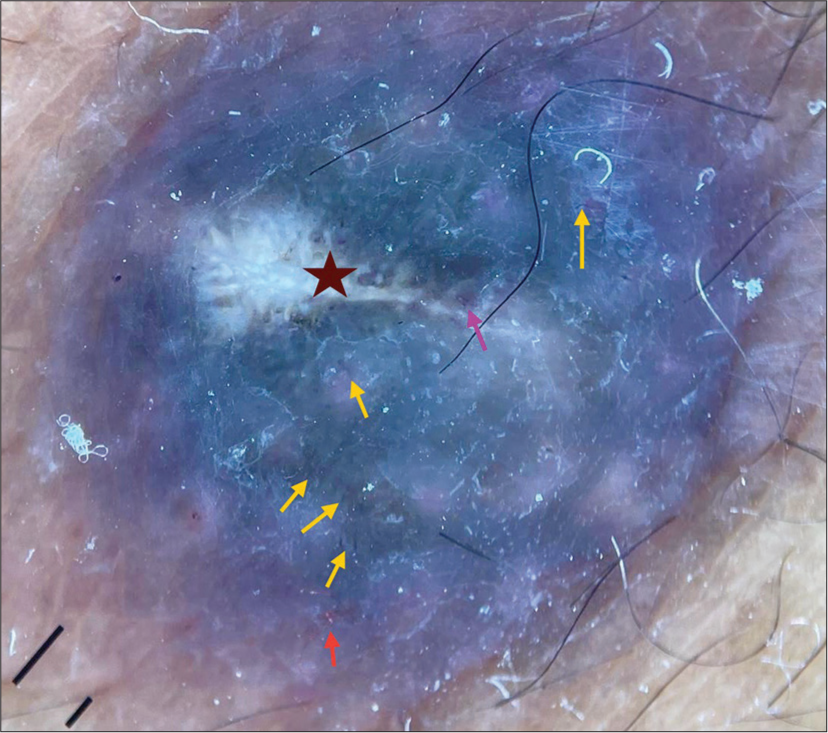
- Dermoscopic findings of hemangioma over left foot: Bluish-pink background, white scales, whitish lacunae (maroon star), dotted vessels (red arrow), hairpin vessel (pink arrow), linear vessels (yellow arrows). (Dermlite DL4 10× magnification polarised mode with pigment boost).
DISCUSSION
Maffucci syndrome was first defined by Carleton et al. (1942), who named it after the Italian pathologist who described the first affected individual in 1881.[4] IDH1 is a known pathogenic gene in enchondromatosis, and ERC2 is a novel gene identified in Maffucci’s syndrome. The somatic L309I mutation of ERC2 contributes to the pathogenesis of hypervascularization to facilitate the development of hemangiomas in Maffucci’s syndrome.[5] Clinically, it presents with asymmetrically distributed enchondromas and vascular tumors, usually over the extremities.
Enchondromas are benign cartilage-forming tumors in the medullary cavity of bone which can involve any bone but most commonly occur in small bones of hands (88%), followed by long tubular bones tibia/fibula (56%), feet (51%), femur (47%), humerus (39%), radius/ulna (37%), ribs (30%) and flat bones such as pelvis (23%).[3] Vascular lesions can be of three types: (a) cavernous hemangiomas, (b) phlebectasias, and (c) lymphangiectasias-lymphangiomas.[6] Hemangiomas in Maffucci syndrome are mostly located in subcutaneous tissue and appear as bluish nodules. The most common sites are hands and feet. Other sites include arms, legs, or trunk.[7]
Complications because of bony involvement include irregular enlargement of enchondromas, which can prevent skeletal growth, causing deformities of the hand and feet, upper limb/lower limb, short stature, limb discrepancies, and pathological fractures.[2] Though it is a benign condition, and there is an increased risk of both skeletal and non-skeletal malignant lesions. The most common tumor chondrosarcoma, occurs in >30% of patients. The age for development of chondrosarcoma can range between 13 and 69 years (average age of 40 years).[7] Non-skeletal malignancies include gliomas, ovarian tumors, cholangiocarcinomas, and other sarcomas.[8]
The condition has to be differentiated from Ollier disease, in which venous malformations are absent, and Gorham’s disease, in which only hemangiomas are observed.[7] Glomuvenous malformations in which lesions would be non-compressible and painful and blue rubber bleb nevus syndrome in which unilateral involvement would be unusual.[9]
Diagnosis can be confirmed with the help of radiological and histopathological examination. The radiography of enchondromas shows radiolucent well-demarcated lesions. Histopathological examination shows dilated vessels and vascular spaces in the mid to lower dermis and subcutaneous tissue. Thrombi often form within vessels and develop into phleboliths. Under microscopic examination, these phleboliths appear as calcified vessels which can be identified by radiography.[7]
Management of this condition depends on the severity of the disease. In asymptomatic patients, treatment is not indicated and only regular follow-up is advised for early detection of complications, particularly malignant transformation. For symptomatic bony lesions, like in pathological fractures, growth defects, or malignant transformation, surgery in the form of corrective osteotomy and lengthening of arm and leg can be done.[7] Curettage and packing with bone grafts are other options for bony lesions, and for symptomatic vascular lesions, sclerotherapy, irradiation, and laser therapy are done.[7] Recently, the role of mammalian target of rapamycin (mTOR) inhibitors has been reported. Rapamycin, an mTOR inhibitor, given 4 mg/day (2.5 mg/m 2/day) to a 20-year-old male with Maffucci syndrome resulted in softening of nodules, decreased pain, and less purplish lesions as early as two weeks into treatment.[10]
CONCLUSION
Maffucci syndrome is a very rare disease characterized by multiple enchondromas with vascular lesions. There is a risk for both sarcomatous transformation of the enchondromas as well as systemic malignancies. There is a need for both treatment of the immediate orthopedic complications of the disease and a systematic approach to ongoing annual surveillance using advanced imaging and routine physical examination for timely diagnosing associated malignancies.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Unilateral mosaic cutaneous vascular lesions, enchondroma, multiple soft tissue chondromas and congenital fibrosarcoma-A variant of Maffucci syndrome? Pediatr Dermatol. 2008;25:205-92.
- [CrossRef] [PubMed] [Google Scholar]
- Best cases from the AFIP. Maffucci syndrome: Radiologic and pathologic findings. Armed forces institutes of pathology. Radiographics. 2001;21:1311-6.
- [CrossRef] [PubMed] [Google Scholar]
- The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987;69:269-74.
- [CrossRef] [PubMed] [Google Scholar]
- IDH1 R132C and ERC2 L309I mutations contribute to the development of Maffucci's Syndrome. Front Endocrinol (Lausanne). 2021;12:763349.
- [CrossRef] [PubMed] [Google Scholar]
- Maffucci's syndrome: A rare case report with unusual location. Med J DY Patil Vidyapeeth. 2019;12:65-8.
- [CrossRef] [Google Scholar]
- Long term oncologic surveillance in Maffucci syndrome: A case report. J Oncol Sci. 2017;3:140-4.
- [CrossRef] [Google Scholar]
- Maffucci syndrome in an eight-year-old girl. Indian J Dermatol Venereol Leprol. 2015;81:412-4.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of rapamycin for refractory hemangioendotheliomas for Maffucci's syndrome. J Clin Oncol. 2012;30:e213-5.
- [CrossRef] [PubMed] [Google Scholar]






