Translate this page into:
A rare case report of penile schwannoma
*Corresponding author: Rehab Ahmed Alhejairi, Department of Dermatology, Dermatology Hospital of Southern Medical University, Guangzhou, China. rehab_hujairi@hotmail.com
Wujian Ke, Department of Dermatology, Dermatology Hospital of Southern Medical University, Guangzhou, China. kewujianstauch@163.com
-
Received: ,
Accepted: ,
How to cite this article: Alhejairi RA, Ke W, Alnour R, Chen Z, Li X, Chen Y. A rare case report of penile schwannoma. J Skin Sex Transm Dis. 2024;6:163-6. doi: 10.25259/JSSTD_29_2024
Abstract
Penile neoplasms are rare, and diagnosis of these are challenging. There have been only 27 cases of penile schwannomas (PSs) documented in English medical literature. We report a case of PS. A 36-year-old male patient presented with a penile tumor that had grown steadily over the past year without causing the patient any pain or affecting his sexual aptitude and performance. The dermatological examination and ultrasonographic evaluation yielded inconclusive results. The diagnosis of PS was confirmed through histopathological and immunohistochemical investigation.
Keywords
Schwannoma
Penile
Case report
Benign neoplasm
Tumor
INTRODUCTION
Schwannomas are benign neoplasms that arise within the sheath surrounding nerves, which can manifest either sporadically or in patients with neurofibromatosis. While the penis is richly innervated, schwannomas that affect the penis are extremely rare. A total of 27 cases of penile schwannomas (PSs) have been documented in the past. Tumors frequently arise due to the loss of function of the gene that encodes neurofibromatosis type 2, which is responsible for producing the Merlin protein. The disorder can manifest as either benign or malignant, although the majority of instances are benign.[1]
Schwannomas can manifest in several anatomical locations and are predominantly seen in the cranial and peripheral regions. The overall prevalence of all schwannomas was 1 in 50,000 individuals, while the prevalence of intracranial schwannomas was 1 in 80,000 individuals, and the prevalence of peripheral schwannomas was documented at 0.6/100,000 individuals.[2]
PS does not have distinct clinical characteristics. The bulk of the tumor appears either as single or multiple isolated, gradually expanding, and well-defined lesions. PS is often non-tender, firm, and fixed. A histological investigation, particularly immunohistochemistry analysis to detect positive S-100 is essential to make a diagnosis of PS. The preferred course of action for PS is surgical excision, and the probability of recurrence following the procedure is minimal. We report a case of PS.[3]
CASE REPORT
A 36-year-old male presented with an isolated subcutaneous tumor near the coronal sulcus of penis for a duration of one year. The lesion started as a rice-sized asymptomatic subcutaneous tumor on the patient’s penis, which required no treatment at the time. Within a year, the tumor’s size gradually increased; however, it did not affect the quality of his life. Laboratory and radiological workup, including complete blood picture, liver and renal functions, chest radiograph, and abdominal B-ultrasound, did not indicate any abnormalities. However, the ultrasound showed a circumscribed hypoechoic area. A dermatological examination of the lesion revealed a 1 × 1.5 cm mobile nontender tumor near the coronal sulcus of the penis [Figure 1]. The tumor is round, with a firm texture, smooth surface, and borders. It arose from the skin. There was no inguinal lymph node enlargement and penile erection is not causing any pain or curvature.

- A 1 × 1.5 cm tumor occurs near the corona of the penis.
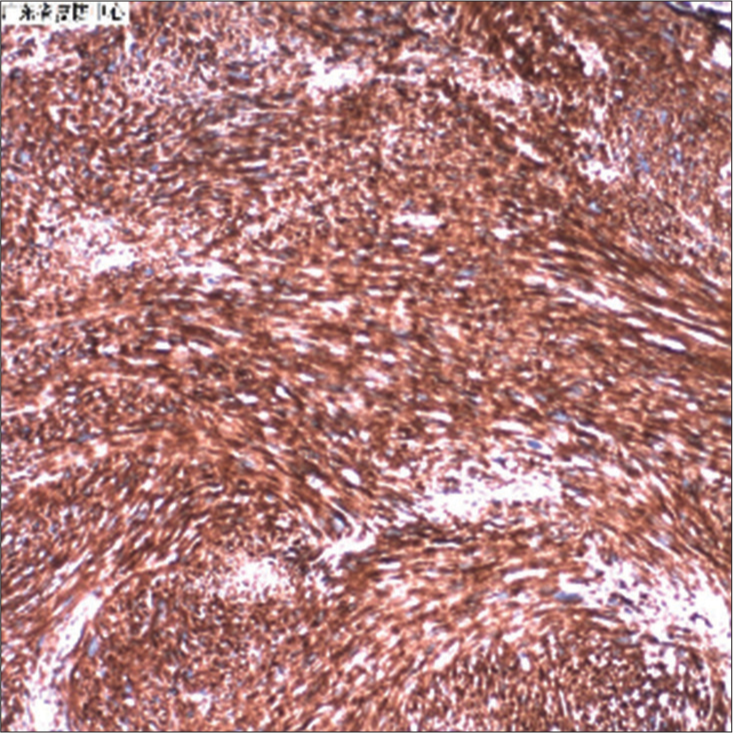
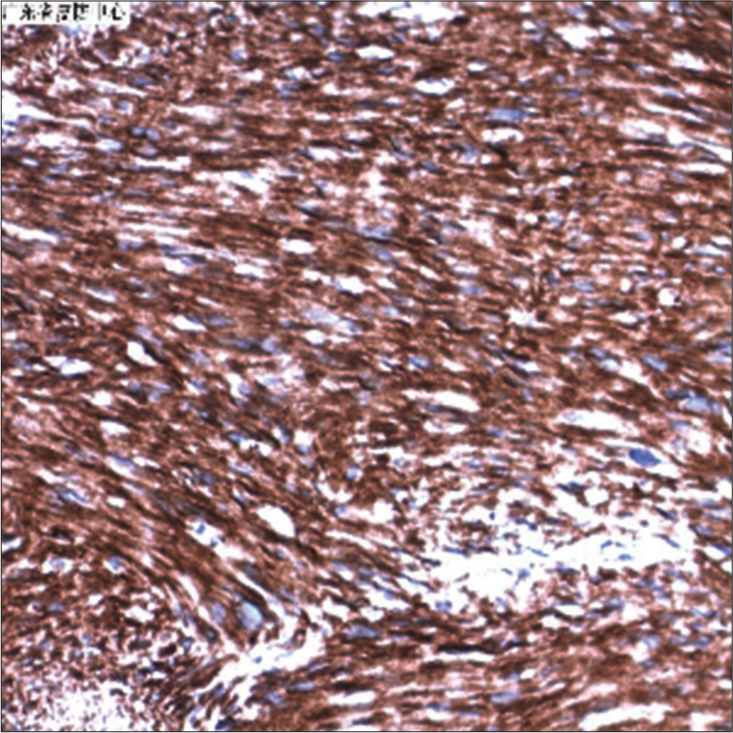
In addition, histopathological examination using hematoxylin and eosin staining revealed an intradermal circular tumor with a clear boundary composed of spindle cells. The section showed alternating Antoni A and Antoni B areas. Cells were braided and arranged as cytoplasmic staining shows red, mild nuclear atypia, and some nuclear staining hyperchromatic with mild hypertrophy [Figures 2 and 3]. Immunohistochemical analysis revealed diffuse, strong positivity for S-100 protein. In addition, S-100 immunoperoxidase was positive for almost all spindle-shaped cells, with strong positivity for vimentin [Figures 4-7].
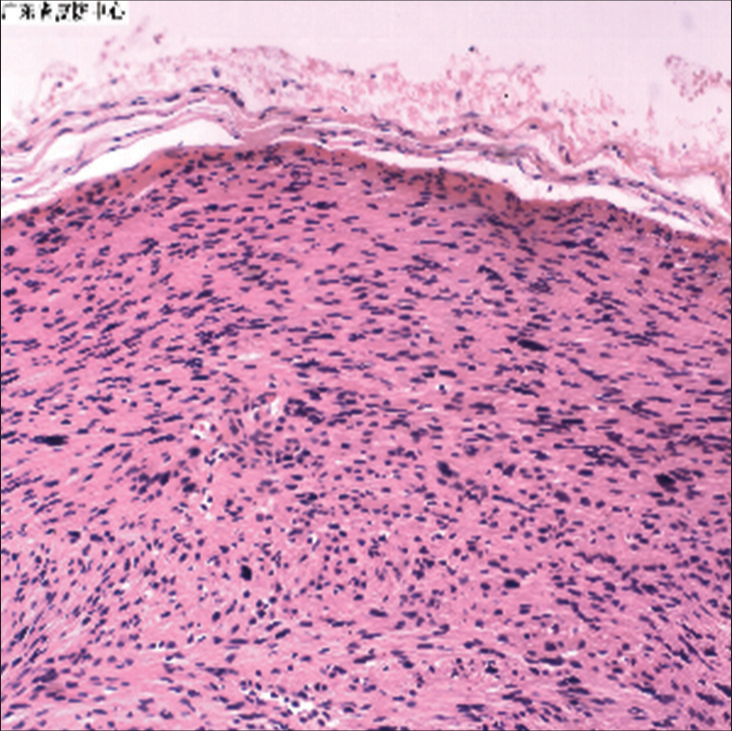
- The boundary of the tumor is clear, and the spindle cells are braided arranged (hematoxylin & eosin, ×100). Microscopic section shows that the nodules were well delineated and consisted of interlacing bundles of spindle-shaped cells.
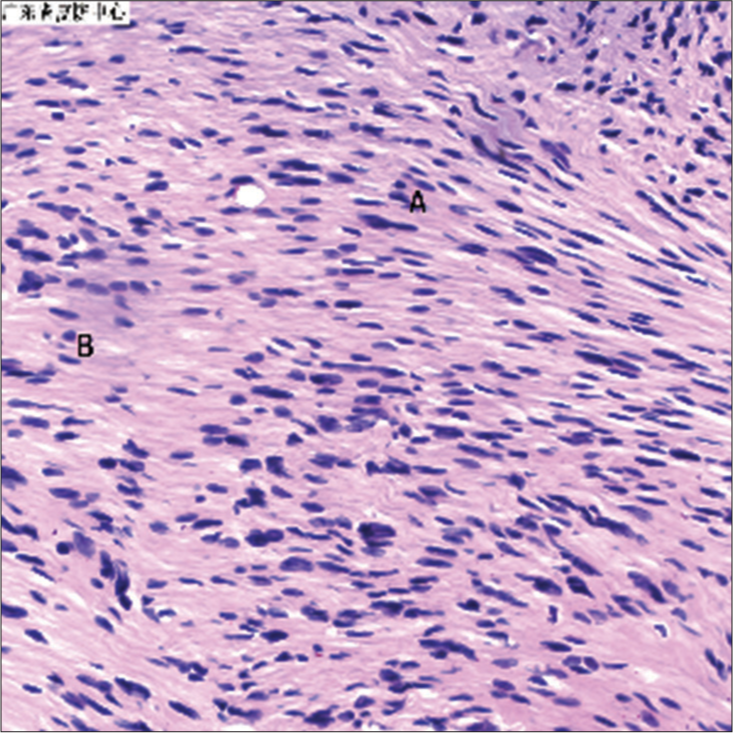
- Antoni A tissue consists of high cellularity area. Foci of palisaded nuclei (Verocay bodies) are seen. Antoni B tissue shows low cellularity of spindle cells on myxoid stroma. Hematoxylin and eosin, ×400.
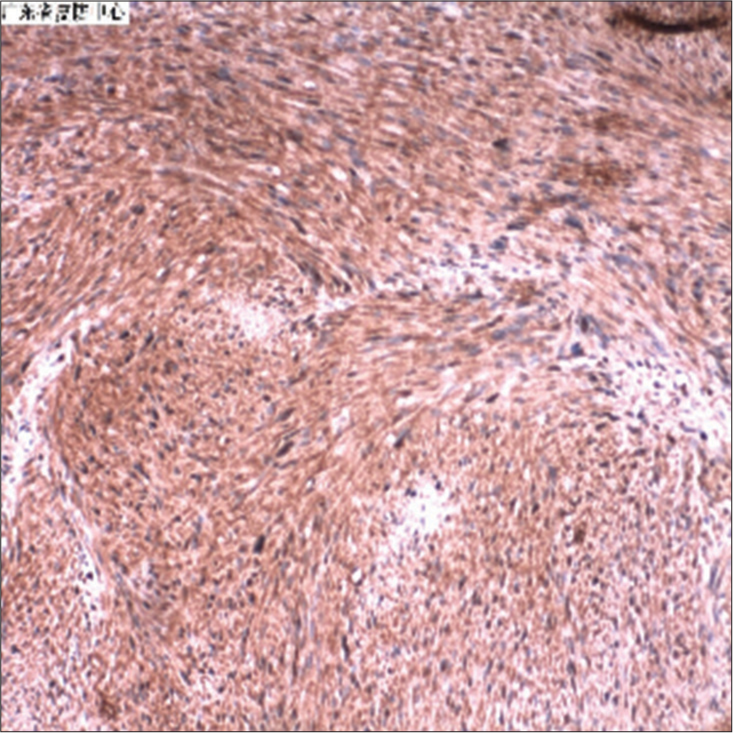
- S100 (+ +) stain using S-100 immunoperoxidase shows intensely positive reaction. Reduced from ×100.
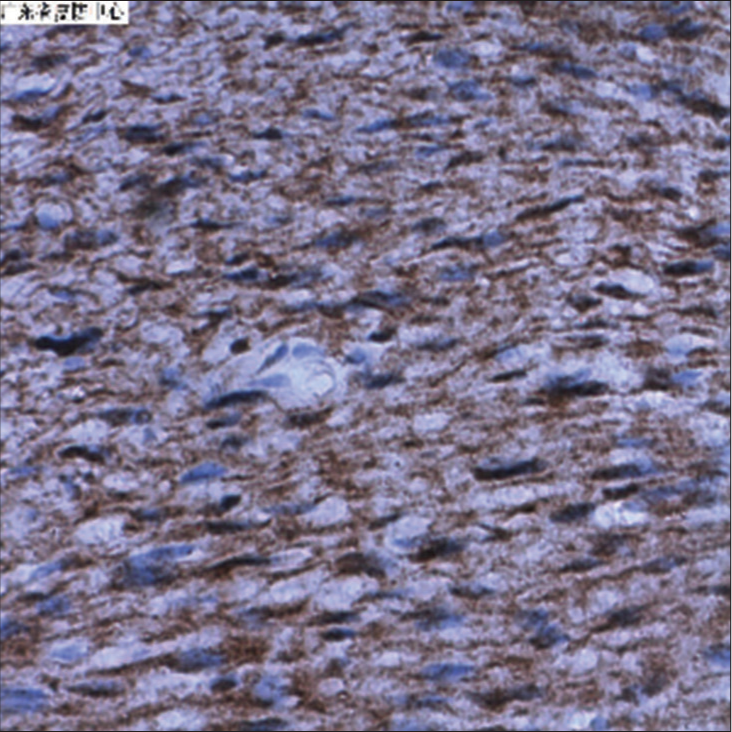
- S100 (+ +), Intracellular expression of tumor. S-100 immuno-peroxidase was positive for almost all spindle-shaped cells. Reduced from ×400.
- Immunohistochemical staining of tumor with vimentin showing intracellular expression of vimentin (×100).
- Immunohistochemical staining of tumor with vimentin showing intracellular expression of vimentin (×100).
Finally, the patient’s lesion was confirmed as PS, and the lesion underwent surgical resection under local anesthesia.
DISCUSSION
Schwannomas can develop in many anatomical areas, and they typically appear in the limbs and skull. They are mostly observed in the seminal vesicles, testicles, bladder, prostate, and spermatic cord. In the case presented, the tumor manifested in the penis, and this type of penile tumor is considered a rare occurrence, and the majority of them are benign. The first recorded documentation of PSs dates back to 1968.[4]
PSs have been linked to penile curvature, erectile dysfunction, and unpleasant sexual intercourse,[5] while schwannoma, in this case, presents as a single, painless, slow-growing tumor that does not cause any symptoms.
Schwannomas can be classified into three main forms: Melanocytic, plexiform, and cellular schwannomas. Cellular schwannomas, which were detected in this case, commonly have elevated cell density and mitotic activity. In addition, they have a higher occurrence of local recurrence in comparison to ordinary schwannomas. Plexiform schwannomas commonly occur in superficial areas and are composed of a substantial amount of Antoni A-type tissues. Melanotic schwannomas are uncommon and have a low probability of being malignant. It is crucial to differentiate between melanoma and neoplasms that produce melanin.[6]
We decided to excise the tumor surgically, as surgical removal is the preferred initial treatment for benign schwannomas. During the surgical treatment, the tumor was easily removed. We advise doing a wide excision of the affected area, ensuring that there are no cancerous cells left behind.[7]
The histopathologic examination revealed predominantly spindle-shaped cells that frequently arranged themselves in palisades, exhibiting a mixture of Antoni A and Antoni B patterns. The immunohistochemistry results of S100 showed nearly full positive staining,[8] suggesting the presence of a benign tumor. Conversely, smooth muscle actin and desmin yielded a negative outcome. It also showed vimentin -positive staining.[9]
During the surgical removal, we were unable to detect any blood vessels supplying blood to the tumor. Typically, a clearly identifiable hypoechoic mass with enhanced sound transmission posteriorly is observable in ultrasonography; however, ultrasonography was not very effective in diagnosing this case of schwannomas.[10]
CONCLUSION
Penile schwannomas are extremely uncommon tumors with a favorable prognosis. Due to its great vascularity, it may be misdiagnosed as hemangioma in ultrasonography. Schwannomas differ in vascularity and could develop in the areas of the body where nerves are supplied and are crossed. In the case presented in this report, the schwannoma had poor and nearly invisible blood supply, and it is only revealed through histopathology. Therefore, even in rare instances, physicians must conduct further investigations to rule out schwannoma when presented with an unknown tumor.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Clinical features and treatment of penile schwannoma: A systematic review. Clin Genitourin Cancer. 2016;14:198-202.
- [CrossRef] [PubMed] [Google Scholar]
- Penile schwannoma mistaken for hemangioma: A rare case report and literature review. Transl Androl Urol. 2021;10:2512-20.
- [CrossRef] [PubMed] [Google Scholar]
- Plexiform schwannoma of the penis: A rare subtype of genital Schwannoma. Case Rep Urol. 2019;2019:1752314.
- [CrossRef] [PubMed] [Google Scholar]
- Case report and literature review: Plexiform schwannoma in the penile and inguinal region in a child. Front Oncol. 2024;14:1356000.
- [CrossRef] [PubMed] [Google Scholar]
- A clinicopathological study of peripheral schwannomas. Med Pharm Rep. 2021;94:191-6.
- [CrossRef] [PubMed] [Google Scholar]
- Complete resection of penile schwannoma without sexual dysfunction. Turk J Urol. 2010;36:207-10.
- [CrossRef] [Google Scholar]
- Clinicopathological presentation and management of penile schwannoma. Sex Med Rev. 2020;8:615-21.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple penile and pelvic schwannomas in an adult male: A case report. J Clin Diagn Res. 2023;17:TD03-5.
- [CrossRef] [Google Scholar]
- Neoplasms of the penis and scrotum In: Genitourinary radiology: Male genital tract: adrenal and retroperitoneum: The pathologic basis. London: Springer London; 2013. p. :199-210.
- [CrossRef] [Google Scholar]






