Translate this page into:
Abrikossoff tumor of the vulva
*Corresponding author: Pradeep S. Nair, Department of Dermatology and Venereology, Government Medical College, Thiruvananthapuram, Kerala, India. dvmchtvm@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Nair PS, Sudhesan A. Abrikossoff tumor of the vulva. J Skin Sex Transm Dis. 2024;6:221-2. doi: 10.25259/JSSTD_50_2023.
A 36-year-old female patient presented with no history of pre or extramarital sexual contact and gave the history of a single, asymptomatic, and raised lesion over labia minora of 4 years duration. On examination, a single, well defined, non-tender, non-bleeding, oval, reddish brown, and indurated plaque of size 2 × 1 cm with a smooth surface was present at the junction of the upper one-third and lower two-third of left labia minora [Figure 1]. There was no vaginal discharge or inguinal lymphadenopathy. Viral markers for human immunodeficiency virus, hepatitis B, C, and investigations for other sexually transmitted infections were negative.

- Well-defined oval indurated smooth surfaced plaque on left labia minora.
An excision biopsy and histopathological examination demonstrated a tumor composed of sheets of large polyhedral cells with eosinophilic granular cytoplasm and small round central basophilic nuclei with distinct cell borders, diagnostic of Abrikossoff tumor [Figure 2]. Abrikossoff tumor (granular cell tumor) is a rare benign peripheral nerve sheath tumor of Schwann cell origin, the usual sites being the tongue, head, neck, and breast, the vulva being a very rare site. The tumors are S-100 positive and periodic acid-schiff positive, staining the cytoplasmic granules, while diastase resistant. Rarely malignant transformation (2%) may occur. Excision margin is the treatment of choice as this tumor can infiltrate deep and recurrences are possible in 2–8%. In our patient, excision was done with a 1 cm margin of normal skin. Recurrent tumors may be treated with radiation and chemotherapy–pazopanib a selective tyrosine kinase inhibitor that blocks tumor growth and inhibits angiogenesis.
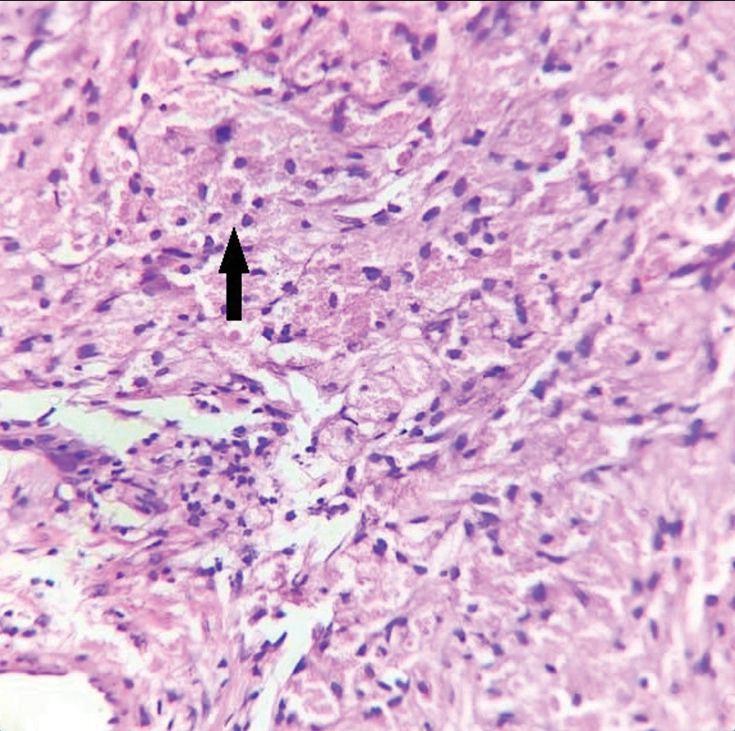
- Sheets of well-defined polyhedral cells with granular eosinophilic cytoplasm and central basophilic nuclei (arrow) in the dermis, Hematoxylin & eosin, ×400.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Pradeep S Nair is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.





