Translate this page into:
Atypical presentation of plasma cell vulvitis
*Corresponding author: Joushan Lulu Kuruvadangal, Department of Dermatology, Venereology and Leprosy, Kunhitharuvai Memorial Charitable Trust Medical College, Kozhikode, Kerala, India. joushankh25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kuruvadangal JL, Nair LV, Riyaz NA. Atypical presentation of plasma cell vulvitis. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_74_2024
Abstract
Vulvitis circumscripta plasmacellularis, or plasma cell vulvitis (PCV), was described by Zoon. It typically appears as distinct, glossy, erythematous macules of the vulvar mucosa. We describe an uncommon manifestation of PCV with vegetative growth in a 71-year-old woman.
Keywords
Plasma cell vulvitis
Vegetative growth
Vulvitis circumscripta plasmacellularis
INTRODUCTION
Plasma cell vulvitis (PCV), or Zoon’s vulvitis or vulvitis circumscripta plasmacellularis, is an uncommon idiopathic dermatosis originally described in 1952.[1] It is a spectrum of plasma cell mucositis, which can involve the oral mucosa (buccal mucosa, lips, palate, gingiva, tongue, epiglottis, and larynx) and glans penis.[2] The labia, clitoris, urethral meatus, posterior fourchette, and vaginal canal may have lesions.[1] We present a case of PCV characterized by vegetative growth, which represents an atypical clinical manifestation.
CASE REPORT
A 71-year-old woman presented with itchy vegetative growth over the vulva for six months, which is not associated with bleeding, oozing, or foul-smelling discharge. There was no past history of any medical treatment for the same. She was diagnosed to have hypertension and bronchial asthma. She is on regular medication with amlodipine and inhaler therapy. Her gynecology and obstetrics history were unremarkable, and she attained menopause 25 years ago.
Per speculum examination showed an atrophied cervix and stenosed external opening of uterus. The vulva was replaced by a thick irregular growth with an everted margin nodular surface with a surrounding thick white plaque extending to the left labia majora, vestibule, and labia minora [Figure 1].

- Clinical picture of vegetative growth over vulva.
Direct visual inspection with acetic acid showed acetowhite areas at 6 o’clock, more toward the left side. Lugol’s iodine staining showed a uniform mahogany brown staining of the cervix with unstained areas at the 2’0 clock position, and a biopsy was taken from a lightly stained area [Figure 2]. All baseline investigations were within normal limits, including human immunodeficiency virus (HIV), hepatitis B virus, and hepatitis C virus serology.

- Clinical photograph lesion after applying Lugol’s iodine.
Since the lesion was vegetative, we considered a provisional diagnosis of verrucous carcinoma of the vulva with vaginal nodules and squamous cell carcinoma, and a simple vulvectomy was done by sparing the clitoral body. Three specimens were taken: Cervical tissue, posterior vaginal wall tissue, and a simple vulvectomy specimen. Biopsy of the vulva showed partly ulcerated epidermis, irregular acanthosis with pigment incontinence, and dense lymphoplasmacytic infiltrate along with sheets of plasma cells interspersed by congested blood vessels extending up to mid dermis, periadnexal, and perivascular areas. There were sheets of plasma cells interspersed with congested blood vessels without evidence of dysplasia, suggesting PCV [Figure 3]. A cervical tissue biopsy showed chronic cervicitis [Figure 4]. The follow-up period was uneventful and the patient is asymptomatic till now.
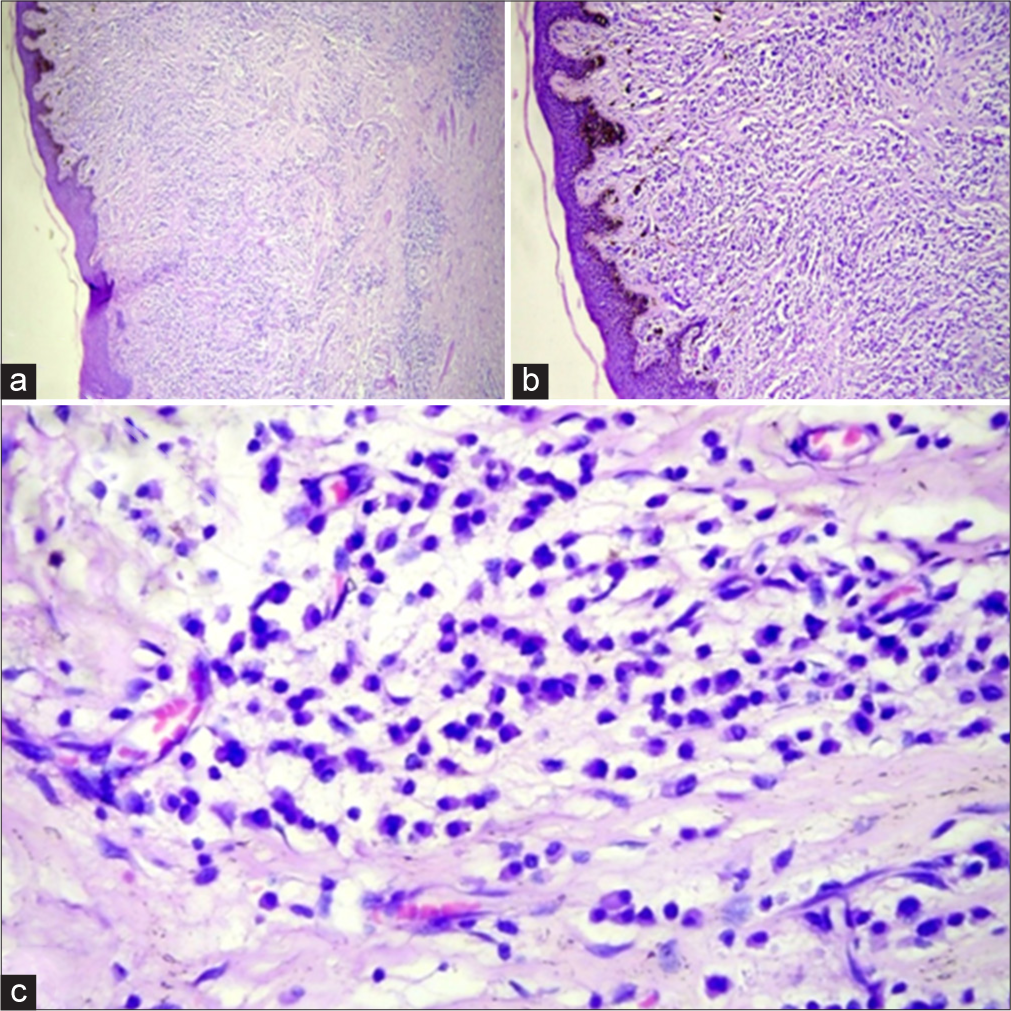
- (a): Histopathology of vulva showing irregular acanthosis and dense infiltrate extending up to mid dermis, periadnexal, and perivascular areas (H&E, 40X); (b): high-power view showing pigment incontinence and dense lymphoplasmacytic infiltrate up to middermis, periadnexal, and perivascular areas (H&E, 40X); (c): sheets of plasma cells with scattered congested blood vessels. No evidence of dysplasia (H&E, 100X). H&E: Hematoxylin and eosin.
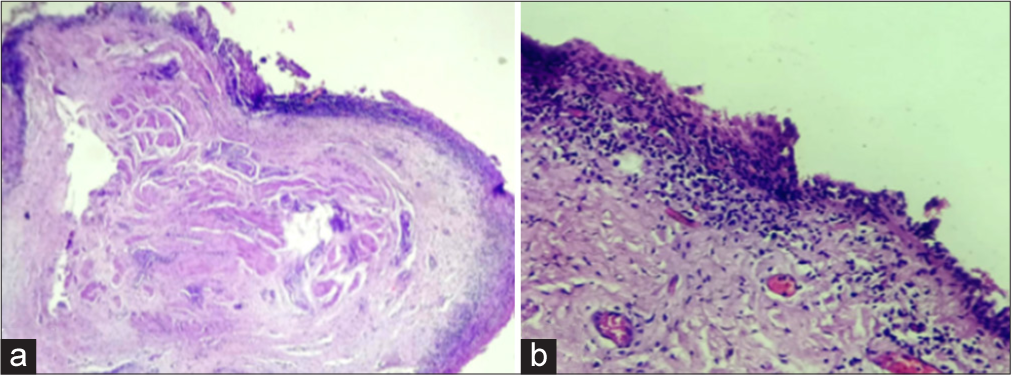
- (a): Histopathological examination of cervical tissue: Transitional zone of cervix with endo and ectocervical epithelium (H&E, 40X); (b): numerous scattered chronic inflammatory cells, lymphocytes, occasional plasma cells, and macrophages. Congested vessels are seen in the adjacent subepithelial tissue suggestive of chronic cervicitis (H&E, 40X). H&E: Hematoxylin and eosin.
DISCUSSION
Zoon’s vulvitis is a relatively rare, benign disease of the vulvar mucosa that commonly affects women aged 26-70.[3] Although the exact etiology is unknown, many factors have been postulated, including autoimmune, infections, hormonal, and irritant factors such as poor hygiene, sweating, and persistent friction. The characteristic clinical findings are bright red to cayenne-pepper or orange-hued, well-demarcated macules or patches involving the vulvar vestibule, periurethral area, and labia minora.[2,4] The condition may be asymptomatic or with symptoms of burning, dyspareunia, pruritus, and pain.[4,5] Erosive or granulomatous lesions are rarely observed. The lesions can be found in the small and large labia, clitoris, urethral meatus, posterior fourchette, and vagina. Our patient had intense pruritus and vegetative growth. Ulcerovegetative growth was reported in an HIV patient.[1] Our patient had an irregular nodular growth with satellite nodules in the vagina that replaced the vulva and extended into the vestibule and labia minora, and her HIV serology was non-reactive. Solt et al. described a case of ulcerative PCV in which the ulcer was excised locally, and there was no recurrence after 2 years of follow-up.[6]
Histology shows plasma cell-dominated infiltrates in the upper dermis, extending into the mid-reticular dermis. In addition, “lozenge-shaped” keratinocytes, mast cells, lymphocytes, and sometimes eosinophils and neutrophils may be observed.[4] Our patient had mainly dense infiltration of plasma cells only.
Several therapeutic approaches have been tried, including excision, platelet-rich plasma, carbon dioxide laser, and topical medications such as steroids, tacrolimus, and imiquimod. Systemic treatments such as steroids, etretinate, estrogens, and interferons are also used.[2] In our patient, the lesion was excised to exclude malignancy.
PCV remains a rare and underreported cause of vulval dermatoses, presenting significant challenges in both diagnosis and treatment. Further studies are necessary to establish uniform treatment guidelines, especially for cases with unusual manifestations and those that are recalcitrant to monotherapy.[7]
CONCLUSION
Our patient had a rare clinical manifestation of PCV with vegetative growth, which replaced the vulva. To the best of our knowledge, a vegetative lesion was described in HIV patients, but our patient’s HIV serology test was negative. Hence, PCV should be considered a differential diagnosis of any vegetative lesions of the vulva.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Zoon vulvitis as a differential diagnosis in an HIV-infected patient: A short report. J Int Assoc Provid AIDS Care. 2013;12:159-61.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell vulvitis: A systematic review. Int J Womens Dermatol. 2021;7(5 Part B):756-62.
- [CrossRef] [PubMed] [Google Scholar]
- Vulvitis plasmacellularis: Two new cases. Sex Transm Infect. 1995;71:311-3.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell vulvitis. Indian J Sex Transm Dis AIDS. 2015;36:185-7.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell vulvitis: A vulvar itching dilemma. Indian J Dermatol Venereol Leprol. 2012;78:230.
- [CrossRef] [Google Scholar]
- Ulcerative vulvitis circumscripta plasmacellularis. Isr Med Assoc J IMAJ. 2004;6:117-8.
- [Google Scholar]
- Plasma cell vulvitis: A case report. Case Rep Womens Health. 2024;42:e00601.
- [CrossRef] [PubMed] [Google Scholar]






