Translate this page into:
Brodalumab: Looking beyond psoriasis
*Corresponding author: Aditya Kumar Bubna, Department of Dermatology, Katihar Medical College, Katihar, Bihar, India. zimbabwa21@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bubna AK, Viplav V. Brodalumab: Looking beyond psoriasis. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_14_2025
Abstract
Brodalumab is a fully human monoclonal antibody that selectively targets interleukin-17 receptor A (IL-17RA), blocking the activity of pro-inflammatory IL-17 cytokines. Apart from psoriasis, brodalumab exhibits potential in managing hidradenitis suppurativa, pyoderma gangrenosum, and pityriasis rubra pilaris, with rapid and sustained lesional improvement. Besides, it has shown to have an acceptable safety profile. Although, not currently used in the treatment of bullous pemphigoid, lichen planus, and atopic dermatitis, brodalumab may elucidate efficacy for the same. The unique mechanism of brodalumab in blocking multiple IL-17 cytokines may contribute to its efficacy in patients who have failed other biologic therapies. Adverse effects observed with brodalumab are mild, although rarely serious alterations have been reported. While further research is needed in some areas, brodalumab represents an important therapeutic option for IL-17-mediated inflammatory skin disorders.
Keywords
Brodalumab
Hidradenitis suppurativa
Pityriasis rubra pilaris
Pyoderma gangrenosum
INTRODUCTION
Brodalumab is a fully human monoclonal antibody that targets the interleukin-17 receptor A (IL-17RA), effectively blocking the activity of multiple pro-inflammatory IL-17 cytokines.[1] Although currently approved by the United States Food and Drug Administration (US-FDA) for the management of plaque psoriasis, its utility in other dermatoses has also been demonstrated. This comprehensive review aims to outline the non-psoriatic utility of brodalumab in dermatology.
PHARMACOKINETICS
After subcutaneous (SC) injection, brodalumab is absorbed, with a bioavailability of approximately 55%. It undergoes slow absorption, reaching peak serum concentrations by 3 days. Brodalumab exhibits non-linear pharmacokinetics, with a t1/2 of 10.9 days. Clearance of brodalumab involves degradation into small peptides and amino acids through catabolic pathways, similar to endogenous IgG; and hepatic impairment is not expected to influence its elimination.[2]
METHODS
PubMed, Medline, and Embase databases were searched from the period January 1, 2015, to May 20, 2024. Search terms included; “Brodalumab” AND “pityriasis rubra pilaris” AND “hidradenitis suppurativa” AND “pyoderma gangrenosum” AND “lichen planus” AND “atopic dermatitis” AND “bullous pemphigoid” NOT “psoriasis.” All original studies including case reports, case series, and clinical trials were included if they were full-text, involved a dermatologic disorder treated with brodalumab and published in English. Articles were excluded if they were conference abstracts, non-clinical reports, or in vitro studies. Schematic representation of the search strategy is outlined in Figure 1.
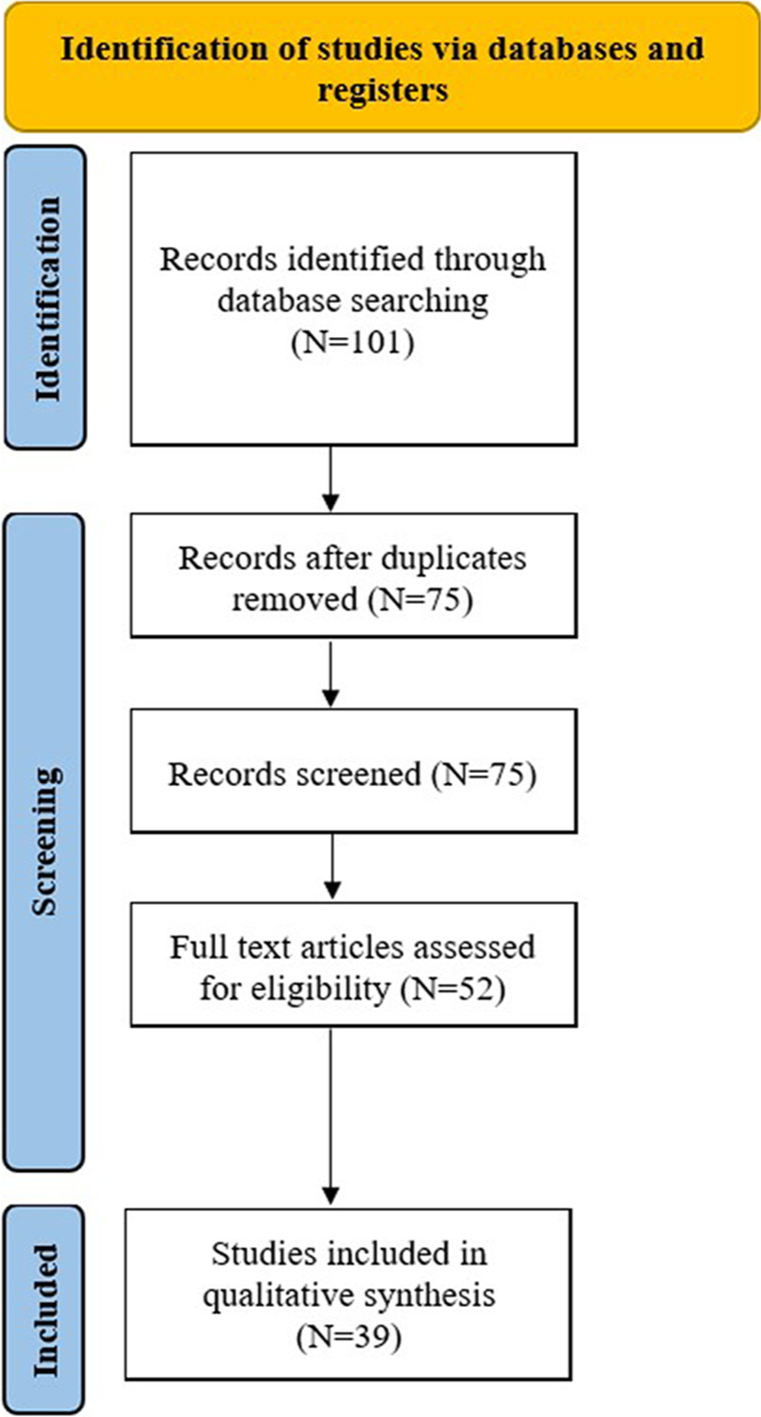
- Schematic representation of the search strategy.
RESULTS
Clinical uses
Hidradenitis suppurativa (HS)
HS is a chronic autoinflammatory follicular disorder, classically involving those body parts rich in apocrine glands, and clinically manifesting as nodules, abscesses, and draining sinuses. Apart from significant physical disability, HS profoundly impacts the emotional aspect of life.[3]
Recently, the IL-17 pathway has been identified as a major player in HS pathogenesis.[4] In HS, IL-17 is expressed, not only in lesional and perilesional tissue but also in unaffected skin; expounding the occurrence of subclinical inflammatory processes, even before the development of active disease.[5] Moreover, elevated levels of IL-17 induce proteins such as IL37/cathelicidin, S100A7, S100A8, and S100A9 that promote cytokine/chemokine expression and keratinocyte proliferation, thereby perpetuating a progressive feed forward loop, eventuating in potential tissue damage.[6,7] IL-17 further acts on nod-like receptor protein-3 inflammasome and stimulates production of transforming growth factor-beta (TGFβ), IL-1β, IL-6 and transforming growth factor-alpha (TNFα) from macrophages, crucial for T helper 17 (Th17) differentiation, and proliferation.[8]
TGF-β facilitates RAR-related orphan receptor gamma-γt (a transcription factor), necessary for generation of Th17 cells;[9] IL-1β and IL-6 individually downregulate Foxp3(another transcription factor), consequently reducing levels of regulatory T cells;[10] and TNFα rapidly induces expression of IL-1β, IL-6, IL-8, IL-2, and adhesion molecules in monocytes/macrophages, promoting a tenacious progressive pathogenic cycle for HS.[11]
Even so, in HS patients, elevated levels of IL-17 A/C/F transcripts and CD4+ IL-17 T cells have been identified in lesional tissue, with increased IL-17A serum levels of these patients.[12] IL-17A and IL-17F work synergistically in promoting inflammation in HS. They act on IL-17C and promote production of other inflammatory cytokines, including IL-17A and IL-17F, and establish a well-coordinated continuous and self-perpetuating inflammatory cascade.[13] Brodalumab, by its unique mechanism of blocking IL-17RA, antagonizes IL-17A, IL-17C, and IL-17F, thereby inhibiting all 3 cytokines and breaking the inflammatory feedback loop which eventuates in amelioration of inflammation, manifesting clinically as resolution of lesions. Besides, it proves superior to ixekizumab and secukinumab in being able to suppress other cytokines, not targeted by them.[12,14]
Table 1 outlines existing literature utilizing brodalumab for treating HS.[14-20] Based on these publications, conflicting results have been observed with brodalumab for HS.[14-20] Although effective in both Hurley stage II and III HS, there have been reports documenting both primary and secondary therapeutic failure with brodalumab.[19] Besides, as brodalumab is a newer biologic drug for HS, its utility is limited to case reports/series. Moreover, brodalumab has never been used as a first-line drug for HS, with its application employed mainly as a second-, third-, or fourth-line therapy. Robust clinical trials, therefore, become essential in clearly determining the exact timing of brodalumab use, including the dose, as well as the duration of brodalumab treatment for HS. Further, addition of antibiotics along with brodalumab while simultaneously managing severe forms of HS is another avenue to embark on.
| S. No. | Authors/Year | Type of study | Patient details | Prior failed treatment | Brodalumab dosing | Outcomes following brodalumab treatment |
|---|---|---|---|---|---|---|
| 1. | Frew et al., [14]/2020 |
Open-label cohort study. |
n=10 (5 males, 5 females). Age range: 21–55 years. 8 patients: Hurley stage 2 disease. 2 patients: Hurley stage 3 disease. |
• Oral antibiotics (n=10). • Adalimumab (n=7). • Infliximab (n=4). • Secukinumab (n=2). • Ixekizumab (n=2). • Wide surgical excision (n=6). |
Label dosing. |
• At week 12, all patients achieved the HiSCR that was maintained at week 29. • At week 12, 80% of patients achieved the IHS4 which was maintained at week 24. • No serious adverse events were encountered. |
| 2. | Yoshida et al.,[15]/2021 |
Case report. | • 47-year-old smoker male (30 cigarettes/day) with HS (Hurley stage 3), with an extensive subcutaneous abscess spreading towards the fascia and muscle layers with coexisting plaque psoriasis and no previous history of biologic use. |
• Antibiotics (for 15 years). • Stab incision drainage. |
Label dosing. |
• At 1-year, satisfactory improvement of both psoriasis and HS were observed. • There was no need for optional treatment with systemic antibiotics or local incision and drainage. • The modified Sartorius score reduced from 102 (baseline) to 30 (8months). • PASI reduced from 10.8 (baseline) to 0 (8 months). • No adverse events were documented after 1.5 years of treatment. |
| 3. | Tampouratzi et al.,[16]/2019 | Case report. | A 42-year-old man with co-existing plaque psoriasis, psoriatic arthropathy and HS (Hurley stage 2). |
• Methotrexate (for 3 years). • Cyclosporine (for 2 years). • Ustekinumab (duration not specified). • Golimumab (for 3 years). • Secukinumab (duration not specified). • Adalimumab (duration not specified). |
Label dosing. |
• IHS4 score reduced from 10 (baseline) to 3 (week 16). • DLQI improved from 25 (baseline) to 1 (week 12). • Both psoriasis and PsA demonstrated significant improvement at week 8 with PASI reducing from 18.5 (baseline) to 1.5 and body surface area (BSA) plummeting from 45% (baseline) to 8%. • No adverse events were encountered. |
| 4. | Arenbergerova et al.,[17]/2020. | Case report. | 45-year-old smoker male with HS (Hurley stage 3). |
• Adalimumab (secondary failure). • Following adalimumab therapy (160 mg at day 1, 80 mg at day 15, and from day 29, 40 mg weekly), good clinical responses were initially seen, with achievement of HiSCR score at week 12. • However, after week 36, disease began worsening, with elevation of pain and discharge of blood-stained pus. |
Label dosing. |
• IHS4 reduced from 62 (baseline) to 18 (week 12). • DLQI reduced from 17 (baseline) to 5 (week 12). • Pain VAS score decreased from 8.7 (baseline) to 3.5 (12 weeks). • Patient tolerated brodalumab treatment well even after 9 months of therapy. |
| 5. | Vagnozzi et al.,[18]/2023. |
Case report. | 50-year-old smoker male with HS (Hurley Stage 3) and plaque psoriasis for 20 years. |
• Adalimumab (for 3 years). • Infliximab (for 5 years). • Etanercept (for 12 months). |
Label dosing. |
• Patient achieved HiSCR at week 12. • At week 24 IHS4 reduced from 56 (baseline) to 20, at week 48 it reduced to 15 and at week 136 it showed a value of 5. • DLQI reduced from 28 (baseline) to 8 (week 48), and 4 (week 136). • No adverse events were encountered even after 34 months of treatment. |
| 6. | Kearney et al.,[19]/2023. |
Case series of 8 patients. |
• 6 females, 2 males. • Age range: 27–79 years. • Smokers: 2. • Hurley stage 2: 3 patients. • Hurley stage 3: 5 patients. |
• Adalimumab (8). • Infliximab (5). • Ustekinumab (2). • Guselkumab (1). • Anakinra (1). |
Label dosing. |
• 1 patient experienced primary failure after 16 weeks of treatment. • 3 patients experienced secondary failure. • 4 patients demonstrated treatment efficacy with the mean DLQI reducing from 20.6 (baseline) to 16.8 (16 weeks). • These 4 patients remained on brodalumab treatment with a mean treatment duration of 11.3 months. • Besides all patients needed concurrent antibiotics due to flares. |
| 7. | Frew et al.,[20]/2021. |
Open label cohort study. | Seven of the 10 patients included in the National clinical trial (NCT) 0396026 participated in this trial. No additional demographic data of the enrolled patients are available. | - | Weekly administration after the induction phase. |
• At week 12 all patients achieved HiSCR, with 50% achieving HiSCR-100. • 80% of participants achieved an IHS4 category change at week 12 and 24 with 50% participants having a 2-category change in IHS4 at week 12 and 24. |
DLQI: Dermatology life quality index, HS: Hidradenitis suppurativa, PASI: Psoriasis area and severity index, HiSCR: Hidradenitis Suppurativa Clinical Response, VAS: Visual Analog Scale, IHS4: International Hidradenitis Suppurativa Severity Score 4
Pyoderma gangrenosum (PG)
PG is a burdensome, painful neutrophilic dermatosis characterized by rapidly evolving painful, irregular ulcers with a violaceous and erythematous edge.[21] It can present in isolation or in association with other immunological conditions like inflammatory bowel disease.[21]
At present, the efficacy of brodalumab has been outlined in two publications [Table 2].[22,23] Diseased skin in PG is characterized by an increased expression of multiple IL-17 isoforms (IL-17A, IL-17C, and IL-17F), that facilitate neutrophilic migration, trigger secretion of IL-6, IL-8, and GM-CSF, and plummet levels of regulatory T cells. In addition, these isoforms upregulate CXCL1, and CXCL8 (IL-8) that again mediate neutrophil chemotaxis and potentially perpetuate the inflammatory cascade.[24,25]
| S. No. | Authors/Year | Type of study | Patient details | Failed prior treatments | Brodalumab dosing | Remarks |
|---|---|---|---|---|---|---|
| 1. | Huang and Tsai[22]/2021 | Case report. |
• 57-year-old lady with recurrent PG, first over the left buttock and then the right. • She was also having Sjogren’s syndrome, dermatomyositis and hyperthyroidism. |
• Prednisolone (10–20 mg/every other day). • Cyclosporine (upto 250 mg/day). • Colchicine (0.25 mg/day). • Methotrexate (10 mg/week). • Hydroxychloroquine (100 mg/day). • Intralesional triamcinolone. • Topical tacrolimus. • Secukinumab (duration not specified). • Duration of non-biological treatment was~6 years. |
Label dosing. | Complete healing of PG on both buttocks was witnessed at week 11 following brodalumab initiation. However, owing to development of putaminal haemorrhage, brodalumab therapy was terminated, although there was no confirmed evidence for this association. |
| 2. | Tee et al.,[23]/ 2020 |
Case series of 2 patients. | Patient 1: 23-year-old man with PASH syndrome. Painful superficial PG was present on the anterior and posterior surfaces of both lower limbs. Patient 2: 52-year-old woman with a 10-year history recurrent PG of the left anterolateral lower limb. |
• Patient 1: • Systemic steroids (up to 1mg/kg/day), • Adalimumab (40 mg/week) and • Methotrexate (7.5 mg/week). • Patient 2: • Intermittent oral and intralesional steroids. • Adalimumab. • Exact duration of treatment not specified. |
Label dosing. | Patient 1: • Within 4 weeks, rapid reduction in swelling, pain and re-epithelization in PG was seen. • Follow up 6 months after starting brodalumab indicated no lesional recurrence. Patient 2: • Within 12-weeks of brodalumab administration PG had re-epithelized with minimal residual pain and edema. • Follow up at 4 months indicated no recurrence of PG. |
PG: Pyoderma gangrenosum, PASH: Pyoderma gangrenosum, Acne Conglobata and Suppurative Hidradenitis
Brodalumab, by blocking multiple IL-17 isoforms, contributes in rapid resolution of PG. Besides, the high recapture rate of brodalumab allows it to be effective even following temporary suspension.[23,26] However, the development of PG in patients receiving brodalumab for psoriasis has been reported following biologic switching from adalimumab, secukinumab, and ustekinumab.[27-29] This occurs secondary to compensatory upregulation of IL-23 following IL-17RA inhibition that disrupts the IL-23/IL-17 axis.[28,29] In addition, there is also disruption in the TNFα-dependent apoptotic pathway, furthering cytokine disequilibrium, eventually precipitating PG.[27] Interestingly, patients with heterozygous polymorphisms within the promoter region of IL-6 genes have been associated with an increased susceptibility for the development of PG. This occurs due to exaggerated IL-6 production in these patients that skew the patients’ immune responses toward a Th17 phenotype and this genetically determined milieu, when coupled with brodalumab-mediated inhibition of IL-17-associated physiological regulatory functions, results in exaggeration of the preexisting Th17 response, that possibly precipitates PG.[28] The clinician should therefore be aware of this therapeutic paradox before prescribing brodalumab for PG.
Further, as brodalumab is contraindicated in patients with Crohn’s disease, it needs to be avoided in those patients of PG associated with the above condition.
Pityriasis rubra pilaris (PRP)
PRP is a rare inflammatory dermatosis characterized by keratotic follicular papules coalescing into scaly orangered plaques. Although easy to diagnose, treatment is often challenging, as a result of which newer agents to treat PRP are being constantly explored. Of late, upregulated expression of Th17 cytokines (IL-17A, IL-17F, and IL-22) as well as TNF, IL-6, IL-12, IL-23, and IL-1β have been demonstrated in PRP.[30] Based on these findings, the utility of brodalumab in PRP has been propounded. Currently, though, the efficacy of brodalumab in PRP is confined to case reports [Table 3],[31-34] with the need for RCTs to strengthen this observation. One major advantage of brodalumab in PRP is its rapidity of action in both lesional clearance and alleviation of pruritus.
| Serial No. | Authors/Year | Type of study | Patient details | Prior failed treatment | Brodalumab dosing | Remarks |
|---|---|---|---|---|---|---|
| 1 | Amat-Samaranch et al.,[31]/2021 | Case report. | A 36-year-old man with severe refractory type 1 PRP. | • Narrow band UVB. • Cyclosporine (4 mg/kg/day, duration not specified). • Ustekinumab (45 mg, at the dose licensed for psoriasis, for 5 months). • Acitretin (25 mg/day, for 5 months). |
Label dosing. | • Within 4 weeks partial response in lesional resolution and complete relief of itch was noted. • After 10 weeks of treatment there was complete response with residual post-inflammatory hypopigmentation. |
| 2 | De Felice et al.,[32]/2020 |
Case report. | • 52-year-old female with familial (type V) PRP who had a waxing and waning course. • Her father and paternal grandfather were also suffering from this disease. |
• Topical corticosteroids. • Acitretin (duration not specified). • Methotrexate (duration not specified). • Cyclosporine. • Several cycles of phototherapy. • Etanercept (50 mg twice weekly for 3 months). • Ustekinumab (45mg, at the dose licensed for psoriasis for 15 months); there was an initial improvement with subsequent relapse. |
Label dosing. | • Skin disease significantly improved following 1 month of brodalumab therapy and had completely cleared at month 2. • Besides palmoplantar keratoderma also completely resolved. • At 5 months of follow up patient remained in remission. • No side effects were encountered. |
| 3 | Khan et al.,[33]/2020 |
Case report. | 62-year-old man with classic adult onset PRP. | • Cyclosporine (for 3 months). • Ustekinumab (for 3 months). • Ixekizumab (for 3 months). • Guselkumab (for 9 weeks). |
Label dosing. | • By week 12 of initiating brodalumab, patient displayed significant clinical improvement. • Long-term remission continued through 6 months of combination therapy of brodalumab and methotrexate with no adverse effects. |
| 4 | De Rosa et al.,[34]/2020. |
Case report. | A 60-year-old man with type 1 PRP. Other comorbidities included type 2 DM, and liver steatosis with elevated hepatic transaminases (because of which methotrexate and acitretin were not given to this patient). | • Cyclosporine (4 mg/kg/day, for 3 months). • Topical corticosteroids. |
Label dosing. | • A complete clinical response was obtained after 2 months with body surface area involvement reducing to 0% from 38% (baseline). • Remission was maintained at 6 months of follow up. |
PRP: Pityriasis Rubra Pilaris, DM: Diabetes mellitus, UVB: Ultraviolet B
The level of evidence for the use of brodalumab in the abovementioned dermatoses is outlined in Figure 2.

- Level of evidence for off-label indications of brodalumab in dermatology.
Special considerations
Although presently not reported, brodalumab may prove to be effective in treating the following dermatoses, as per the rationale stated in Table 4.[35-39]
| S. No. | Dermatological disorder | Suggested rationale for use |
|---|---|---|
| 1. | Bullous pemphigoid | • IL-17 along with IL-23 upregulates expression of proteases and facilitates cleavage of the extracellular domain of BP180, eventuating in blister formation.[35] • IL-17 upregulates cytokine and related genes in the skin of BP patients and activates neutrophils to release neutrophil elastase, thereby facilitating degradation of the basement membrane.[36] • By inhibiting IL-17RA, brodalumab can ameliorate the above responses. |
| 2. | Lichen planus | • In LP, Th17/Tc17 and T-cell derived IL-17A help in inducing and perpetuating an inflammatory response. This is further bolstered by the presence of CD4+/IL-17+and CD8+/IL-17+cells lined along the dermal-epidermal junction, in close proximity to apoptotic epidermal keratinocytes.[37] • By antagonizing IL-17RA, brodalumab can help in thwarting the generation and progression of this inflammatory cascade, thereby helping in alleviating disease pathology. |
| 3. | Atopic dermatitis | • Increased Th17 skewing in pediatric and Asian patients with atopic dermatitis has been observed, and Th1-related markers show an obvious corelation with disease severity.[38,39] • By its IL-17 antagonistic effects, brodalumab may prove to be of value in this subset of patients. |
IL-17: Interleukin-17, IL-17RA: Interleukin-17 receptor A, BP: Blood pressure, Th-17: T helper 17
Safety
Brodalumab is a relatively safe drug, adverse events reported are represented in Figure 3.[40-45] Besides, from phase I, II, and III studies, no case of tuberculosis reactivation following brodalumab therapy was reported, and malignancy rates from long-term clinical trials and 1-, 2-, and 3-year US pharmacovigilance studies in patients receiving brodalumab were 0.9, 1.0, 0.8, and 1.1 events per 100 patient-years, respectively.[45,46]

- Adverse effects reported with brodalumab.
A rare but worrisome adverse effect associated with brodalumab in psoriasis patients is the occurrence of suicidal ideation and behavior. The US FDA has therefore issued a black box warning regarding the association of brodalumab with suicidality. This causation though has been disputed in literature, with the suggestion that untreated or insufficiently treated disease could majorly contribute for the same.[47,48]
Besides, a paradoxical eruption of palmoplantar pustulosis and PG in patients with psoriasis receiving brodalumab has been reported following switching from adalimumab, secukinumab, and ustekinumab, as well as spontaneously, being related to cytokine imbalance and genetic polymorphisms, respectively.[44]
Use in special populations
Pregnancy/lactation
Although no contraindication exists for the usage of brodalumab in pregnancy/lactation, monoclonal antibodies are known to actively be transported through the placenta, especially in the third trimester, and get excreted in modest amounts in breast milk. Risks and benefits to the mother require assessment before initiation or discontinuation of brodalumab.[49]
Crohn’s disease (CD)
In patients with CD, brodalumab is contraindicated. If a patient develops CD while taking brodalumab, it needs to be discontinued; otherwise, CD can progress disproportionately with ongoing brodalumab therapy.[50]
Infections
In patients having a non-resolving infection, brodalumab needs to be discontinued.[51]
Pediatric
Efficacy and safety data of brodalumab in the pediatric population with moderate-to-severe psoriasis are not yet characterized. However, based on adult population data regarding brodalumab, it can become an excellent therapeutic option for treating IL-17-mediated dermatoses in the pediatric population, given the rapid therapeutic onset and high skin clearance rates associated with it.[52]
Geriatric
Brodalumab is seen to be an effective and safe therapeutic option for treating psoriasis in patients ≥65 years and, therefore, can also be used in treating other IL-17-mediated dermatoses. Besides, adverse events do not seem to differ from those reported in younger patients despite the greater frequency of comorbidities in the elderly population.[53]
Monitoring guidelines
Monitoring guidelines of brodalumab are elaborated in Figure 4.

- Monitoring guidelines for brodalumab.
Availability and administration
Brodalumab is a clear to slightly opalescent, colorless to slightly yellow solution. It is administered as a SC injection. It is available as Siliq (in the United States and Canada), Lumicef (in Japan), and Kyntheum (in the European Union). It is available as a single-use prefilled syringe as 210 mg/1.5 mL (140 mg/mL) solution in a packaging of 2 or 3 (monthly dose). Label dosing of brodalumab is 210 mg at weeks 0, 1, and 2, and then every 2 weekly.[2]
Future direction
In off-label dermatological disorders, the appropriate dose and scheduling of brodalumab remain avenues open for further exploration. Besides, combination with non-biological drugs, as well as dual biological therapy for unresponsive cases are other areas that need close scrutiny.
CONCLUSION
Brodalumab serves as a valuable therapeutic option for some inflammatory disorders apart from psoriasis, making it a drug for multiple indications. While common adverse effects are generally mild, the occurrence of rare serious adverse events necessitates ongoing monitoring and research. Overall, brodalumab represents a significant advancement in the management of IL-17-mediated inflammatory dermatoses, offering hope to patients who have not responded to other biologic therapies. Further studies are warranted to fully understand its long-term safety and efficacy across diverse patient populations.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this review.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Mechanism of action of brodalumab may correlate with efficacy in patients with inflammatory skin diseases. J Drugs Dermatol. 2023;22:994-1000.
- [CrossRef] [PubMed] [Google Scholar]
- SILIQ (brodalumab) injection for subcutaneous use: Prescribing Information. 2017. Bridgewater (NJ): Valeant Pharmaceuticals North America LLC; Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761032lbl.pdf [Last accessed on 2025 Jan 10]
- [Google Scholar]
- Hidradenitis suppurativa: An update on epidemiology, phenotypes, diagnosis, pathogenesis, comorbidities and quality of life. J Eur Acad Dermatol Venereol. 2021;35:50-61.
- [CrossRef] [PubMed] [Google Scholar]
- Biologic therapies for the treatment of hidradenitis suppurativa. Expert Opin Biol Ther. 2020;20:621-33.
- [CrossRef] [PubMed] [Google Scholar]
- Cytokine pathways and investigational target therapies in hidradenitis suppurativa. Int J Mol Sci. 2020;21:8436.
- [CrossRef] [PubMed] [Google Scholar]
- IL-17 in inflammatory skin diseases psoriasis and hidradenitis suppurativa. Clin Exp Immunol. 2020;201:121-34.
- [CrossRef] [PubMed] [Google Scholar]
- Keratinocytes and neutrophils are important sources of proinflammatory molecules in hidradenitis suppurativa. Br J Dermatol. 2016;174:514-21.
- [CrossRef] [PubMed] [Google Scholar]
- Central role of Th17 Cells in adaptive immune responses In: IL-17, IL-22 and their producing cells: Role in inflammation and autoimmunity (2nd ed). Heidelberg, New York, Dordrecht, London: Springer; 2013. p. :71-89.
- [CrossRef] [Google Scholar]
- Excess IL-1 signaling enhances the development of Th17 cells by downregulating TGF-β-induced Foxp3 expression. J Immunol. 2014;192:1449-58.
- [CrossRef] [PubMed] [Google Scholar]
- Hidradenitis suppurativa is characterized by dysregulation of the Th17:Treg cell axis, which is corrected by anti-TNF therapy. J Invest Dermatol. 2017;137:2389-95.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment outcomes of IL-17 inhibitors in hidradenitis suppurativa: A systematic review. J Cutan Med Surg. 2022;26:79-86.
- [CrossRef] [PubMed] [Google Scholar]
- IL-17C regulates the innate immune function of epithelial cells in an autocrine manner. Nat Immunol. 2011;12:1159-66.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of subcutaneous brodalumab on clinical disease activity in hidradenitis suppurativa: An open-label cohort study. J Am Acad Dermatol. 2020;83:1341-8.
- [CrossRef] [PubMed] [Google Scholar]
- Longstanding refractory hidradenitis suppurativa responded to a brodalumab monotherapy in a patient with psoriasis: A possible involvement of Th17 across the spectrum of both diseases. J Dermatol. 2021;48:916-20.
- [CrossRef] [PubMed] [Google Scholar]
- Case report: Treating a co-existence of hidradenitis suppurativa and psoriasis with different therapeutic approaches. F1000Res. 2019;8:2002.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of recalcitrant gluteal hidradenitis suppurativa with brodalumab after anti-TNF failure. Int J Dermatol. 2020;59:733-5.
- [CrossRef] [PubMed] [Google Scholar]
- Brodalumab for severe hidradenitis suppurativa: A case of clinicoradiologic improvement and literature review. J Dermatolog Treat. 2023;34:2270091.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of hidradenitis suppurativa with brodalumab in biologic treatment failures: Experiences from a specialty clinic. Clin Exp Dermatol. 2023;48:790-2.
- [CrossRef] [PubMed] [Google Scholar]
- Weekly administration of brodalumab in hidradenitis suppurativa: An open-label cohort study. Br J Dermatol. 2021;184:350-2.
- [CrossRef] [PubMed] [Google Scholar]
- Pyoderma gangrenosum: An updated literature review on established and emerging pharmacological treatments. Am J Clin Dermatol. 2022;23:615-34.
- [CrossRef] [PubMed] [Google Scholar]
- Use of brodalumab for the treatment of pyoderma gangrenosum: A case report. Dermatol Sin. 2021;39:57-8.
- [CrossRef] [Google Scholar]
- Rapid resolution of pyoderma gangrenosum with brodalumab therapy. JAAD Case Rep. 2020;6:1167-9.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular and cellular characterization of pyoderma gangrenosum: Implications for the use of gene expression. J Invest Dermatol. 2022;142:1217-20.e14.
- [CrossRef] [PubMed] [Google Scholar]
- Pyoderma gangrenosum: A review of pathogenesis and treatment. Expert Rev Clin Immunol. 2018;14:225-33.
- [CrossRef] [PubMed] [Google Scholar]
- Recapture rate of brodalumab in patients with a lapse in treatment. J Drugs Dermatol. 2020;19:384-7.
- [CrossRef] [PubMed] [Google Scholar]
- Switch from adalimumab to brodalumab as a possible trigger factor for the onset of pyoderma gangrenosum. Australas J Dermatol. 2024;65:e111-3.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic findings in a patient with paradoxical pyoderma gangrenosum induced by brodalumab. Clin Exp Dermatol. 2023;48:293-5.
- [CrossRef] [PubMed] [Google Scholar]
- First emergence of pyoderma gangraenosum, palmoplantar pustulosis and sacroiliitis in a psoriasis patient associated with switching from secukinumab to brodalumab. J Eur Acad Dermatol Venereol. 2019;33:e406-7.
- [CrossRef] [PubMed] [Google Scholar]
- Interleukin 23-Helper T cell 17 axis as a treatment target for pityriasis rubra pilaris. JAMA Dermatol. 2017;153:304-8.
- [CrossRef] [PubMed] [Google Scholar]
- Response of pityriasis rubra pilaris to brodalumab after primary failure to ustekinumab. Int J Dermatol. 2021;60:e112-4.
- [CrossRef] [PubMed] [Google Scholar]
- Familial pityriasis rubra pilaris successfully treated with brodalumab. Int J Dermatol. 2020;59:885-7.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of pityriasis rubra pilaris with brodalumab. Skin J Cut Med. 2020;4:139-42.
- [CrossRef] [Google Scholar]
- Successful treatment of Pityriasis rubra pilaris with brodalumab. Australas J Dermatol. 2020;61:e249-51.
- [CrossRef] [PubMed] [Google Scholar]
- Integrating longitudinal serum IL-17 and IL-23 follow-up, along with autoantibodies variation, contributes to predict bullous pemphigoid outcome. Sci Rep. 2015;5:18001.
- [CrossRef] [PubMed] [Google Scholar]
- IL-17A is functionally relevant and a potential therapeutic target in bullous pemphigoid. J Autoimmun. 2019;96:104-12.
- [CrossRef] [PubMed] [Google Scholar]
- TH1/TH17 cell recognition of desmoglein 3 and bullous pemphigoid antigen 180 in patients with lichen planus. J Allergy Clin Immunol. 2018;142:669-72.e7.
- [CrossRef] [PubMed] [Google Scholar]
- The Asian atopic dermatitis phenotype combines features of atopic dermatitis and psoriasis with increased TH17 polarization. J Allergy Clin Immunol. 2015;136:1254-64.
- [CrossRef] [PubMed] [Google Scholar]
- Atopic dermatitis endotypes and implications for targeted therapeutics. J Allergy Clin Immunol. 2019;143:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- Brodalumab: 4-year US pharmacovigilance report. J Drugs Dermatol. 2023;22:419-22.
- [CrossRef] [PubMed] [Google Scholar]
- Injection site reactions with the use of biological agents. Dermatol Ther. 2019;32:e12817.
- [CrossRef] [PubMed] [Google Scholar]
- Brodalumab-induced subacute cutaneous lupus erythematosus. Clin Exp Dermatol. 2021;46:926-7.
- [CrossRef] [PubMed] [Google Scholar]
- A possible case of brodalumab-induced ichthyosis. J Dtsch Dermatol Ges. 2023;21:288-90.
- [CrossRef] [Google Scholar]
- Paradoxical eruptions to targeted therapies in dermatology: A systematic review and analysis. J Am Acad Dermatol. 2022;86:1080-91.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term safety of brodalumab in Japanese patients with plaque psoriasis: An open-label extension study. J Dermatol. 2020;47:569-77.
- [CrossRef] [PubMed] [Google Scholar]
- Three-year U.S. pharmacovigilance report of brodalumab In: Dermatol Ther. Vol 34. 2021. p. :e15105. Erratum in: Dermatol Ther, 2022;35:e15664
- [CrossRef] [PubMed] [Google Scholar]
- Psychiatric adverse events during treatment with brodalumab: Analysis of psoriasis clinical trials. J Am Acad Dermatol. 2018;78:81-9.e5.
- [CrossRef] [PubMed] [Google Scholar]
- Depression and anxiety in adults with hidradenitis suppurativa: A systematic review and meta-analysis. JAMA Dermatol. 2019;155:939-45.
- [CrossRef] [PubMed] [Google Scholar]
- Brodalumab In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470324 [Last accessed on 2025 Jan 10]
- [Google Scholar]
- Efficacy and safety of interleukin-17 inhibitors in the treatment of chronic rheumatic diseases: A combined and updated meta-analysis. J Clin Pharm Ther. 2021;46:895-906.
- [CrossRef] [PubMed] [Google Scholar]
- Management strategies for pediatric moderate-to-severe plaque psoriasis: Spotlight on biologics. Pediatric Health Med Ther. 2023;14:435-51.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness and safety of anti-interleukin-17 therapies in elderly patients with psoriasis. Acta Derm Venereol. 2020;100:adv00316.
- [CrossRef] [PubMed] [Google Scholar]






