Translate this page into:
COVID-19 vaccine-induced pain over port wine stain in a patient with phakomatosis pigmentovascularis Type IIb and Sturge–Weber syndrome – A rare case report
*Corresponding author: K. T. Fathima Hazna, Department of Dermatology, Venereology and Leprosy, Kunhitharuvai Memorial Charitable Trust Medical Kozhikode, Kerala, India. fhazna11@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Hazna KF, Nair LV, Suresh A, Riyaz N. COVID-19 vaccine-induced pain over port wine stain in a patient with phakomatosis pigmentovascularis Type IIb and Sturge–Weber syndrome – A rare case report. J Skin Sex Transm Dis. 2024;6:188-191. doi: 10.25259/JSSTD_14_2024
Abstract
Phakomatosis pigmentovascularis (PPV) is a rare syndrome characterized by simultaneous presence of capillary malformation and pigmentary nevi with or without systemic manifestations. Sturge–Weber syndrome (SWS) comprises meningofacial angiomatosis with cerebral calcification. It occurs sporadically with an incidence of 1 in 50,000. We report a rare association of PPV Type IIb and SWS in a 14-year-old girl who developed severe pain and erythema over the lesions following COVID-19 vaccination.
Keywords
Phakomatosis pigmentovascularis
Sturge–Weber syndrome
Port wine stain
COVID-19 vaccine
INTRODUCTION
We report a case of phakomatosis pigmentovascularis (PPV) Type IIb with port-wine stain and Nevus of Ota associated with Sturge–Weber syndrome (SWS) presenting with an unusual cutaneous reaction following COVID-19 vaccination characterized by severe pain and erythema over the lesions.
CASE REPORT
A 14-year-old girl came to the outpatient department with port wine stain (PWS) over the left side of the face along the distribution of ophthalmic and maxillary branch of the trigeminal nerve. PWS was also present over the upper limbs and trunk in an almost symmetrical pattern with a predominance on the right side. The left half of the soft palate was also involved [Figure 1]. Gray blue patches suggestive of Nevus of Ota were present symmetrically on the frontal and temporal areas of the face, periorbital area, conjunctivae, and posterior part of hard palate since birth [Figure 2]. There was a history of seizures at 10 years of age, she was evaluated and treated with antiepileptics for six months after which the treatment was discontinued but she had no further recurrences. There was gradual loss of vision in the left eye since the age of 5.

- (a): PWS involving the face and oral mucosa; (b): PWS involving the trunk; and (c): PWS involving the upper limbs with hypertrophy of right limb. PWS: Port wine stain.
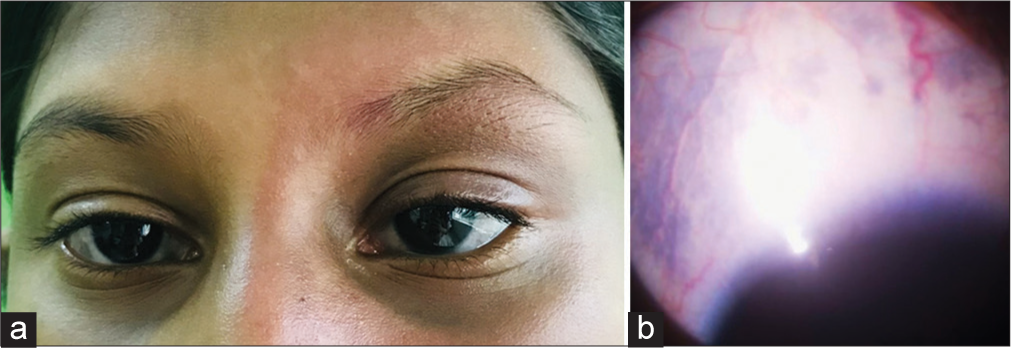
- (a): Nevus of Ota; (b): Scleral melanocytosis.
She noted pain and increased erythema over the PWS following the next day of taking 1st and 2nd doses of COVID vaccination (CORBEVAX). The pain and erythema subsided in a week after the 1st dose but it was persistent after the 2nd dose.
On examination, there was hypertrophy of the right upper limb with a difference of 1.5 cm and 2 cm in the arm and forearm, respectively, compared to the left upper limb. There was severe tenderness and erythema over the areas affected by PWS. However, there was no edema present.
On ophthalmic evaluation, bilateral scleral melanocytosis was noted. Left eye showed buphthalmos, visual acuity of counting finger at 1/2 m, relative afferent pupillary defect, elevated intraocular pressure (24 mmHg), glaucomatous change, and diffuse choroidal hemangioma of the fundus was noted in the left eye. The right eye was normal.
Except for raised erythrocyte sedimentation rate blood and urine routine were normal. Other baseline investigations were normal. Computed tomography (CT) and magnetic resonance imaging (MRI) of the brain showed left cerebral hemisphere volume loss with gliosis and dense parenchymal gyriform calcifications [Figure 3]. Electroencephalogram showed diffuse slowing from the left hemisphere. Doppler study of both upper limbs was normal.
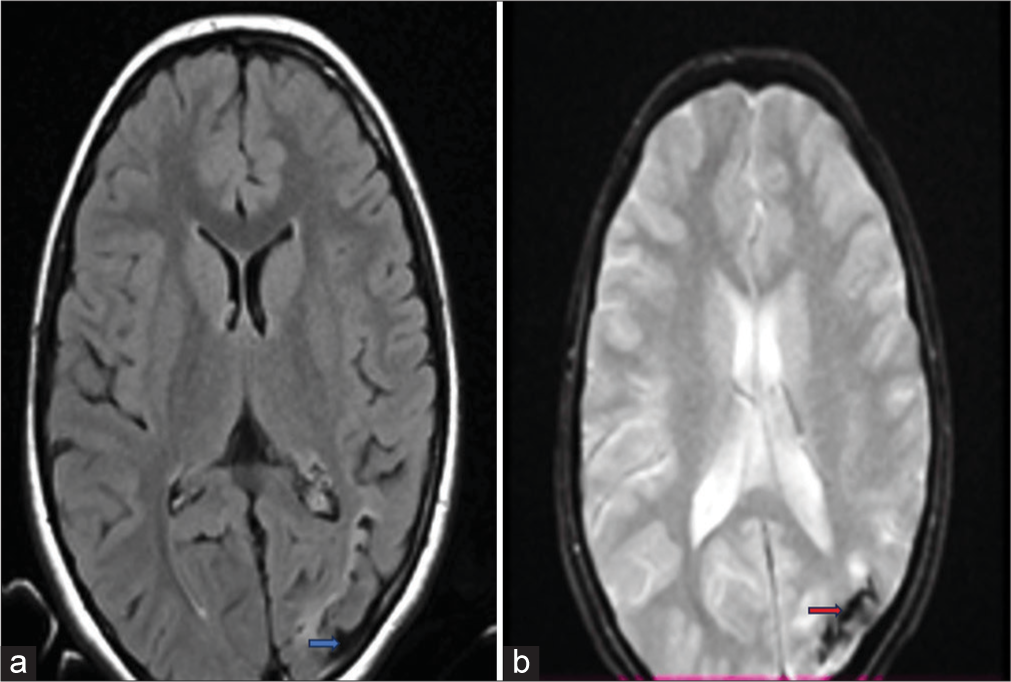
- (a): MRI SWI image showing volume loss (Blue arrow); (b): MRI FLAIR image showing calcifications (Red arrow). MRI: Magnetic resonance imaging, SWI: Susceptibility-weighted imaging, and FLAIR: Fluid-attenuated inversion recovery.
A diagnosis of SWS was made in the presence of extensive PWS, seizures, leptomeningeal involvement, brain calcifications, and glaucomatous changes. A diagnosis of PPV Type IIb was made in view of the presence of PWS with Nevus of Ota with systemic involvement.
As the pain was intense and not relieved with symptomatic measures, she was admitted and treated with a short course of oral prednisolone with a starting dose of 20 mg daily with gradual improvement of her symptoms. The steroid was tapered and stopped over three weeks. She was discharged with topical steroid and was under our follow-up for one month on outpatient basis with no recurrence.
DISCUSSION
PWS in SWS is usually unilateral, but may rarely be bilateral or more extensive involving the trunk, limbs, nasal, and buccal mucosae. The incidence of bilateral facial nevi or capillary hemangiomas on the limbs or trunk is about 40% in all cases.[1] Ocular and leptomeningeal hemangiomas are the other two signs seen in SWS.[2,3] Patients with cortical vein dysplasia will gradually develop dystrophic calcification in the brain secondary to tissue ischemia manifesting as early onset seizures with eventual neurological deterioration and neurodevelopmental delay.[2-4] Our patient developed seizures at 10 years of age and in spite of discontinuation of treatment after six months, which developed no further recurrences which are rather unusual.
Glaucoma the most common ocular complication in SWS is seen in 30–70% of affected individuals and in about 50% of patients presenting with choroidal hemangioma.[5] Our patient developed a decrease in visual acuity from the age of 5 years with loss of vision in the left eye.
PPV is subclassified into four types, with PWS (nevus flammeus) in common. In addition, Type I has epidermal nevus; Type II: Blue spots/melanocytic nevi; Type III: Nevus spilus; and Type IV: Blue spots and nevus spilus.[6] Till date only around 250 cases have been reported. Most patients (75%) represent phakomatosis cesioflammea (Type IIa and IIb).[6] Our patient had PWS with nevus of Ota and systemic manifestations of SWS as reported in PPV Type IIb.
CORBEVAX vaccine is a protein subunit vaccine containing receptor binding domain of SARS-CoV-2 spike protein adsorbed to the adjuvant Alhydrogel (Alum).[7] There are various types of vaccines available against SARS-CoV-2 and post-marketing surveillance of these vaccines has reported various cutaneous adverse reactions.
The spike protein stimulates host immune system to produce antibody against coronavirus resulting in a systemic inflammatory response. It is noticed that the vascular malformations which were earlier silent become symptomatic in the setting of a trauma, infection, or systemic inflammation. The systemic inflammation following vaccination may lead to recruitment of macrophages expressing vascular endothelial growth factor A (VEGFA) and monocytes to site of venous malformations where VEGFA receptors are expressed on endothelial cells. This may contribute to increased erythema and pain over the skin lesion exacerbating vascular malformations.[8] Thrombotic events following vaccination due to antibody production against platelet factor 4 stimulating the coagulation system or autoimmune-related vasculitis may be other mechanisms.[9,10] However, there were no features of thrombosis evident in imaging studies of limbs, brain, and on fundus examination in our patient. The diagnosis of cerebral vasculitis is difficult due to non-specific symptoms and absence of any specific biomarker. The most common feature radiographic feature of vasculitis in MRI brain is ischemia, which will be absent in 10% cases. Other diagnostic methods include central nervous system biopsy, which was not done in this patient.[11]
CONCLUSION
This child had a rare combination of congenital neurocutaneous disorders with a systemic inflammatory response to CORBEVAX vaccine. To the best of our knowledge, there have been no reports of similar adverse effects following COVID vaccination.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Laxmi V. Nair and Dr. Najeeba Riyaz are on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Neuroradiologic findings in a young patient with characteristics of Sturge-Weber syndrome and Klippel-Trenaunay syndrome. J Child Neurol. 2005;20:911-3.
- [CrossRef] [PubMed] [Google Scholar]
- Disorders affecting cutaneous vasculature In: Griffiths C, ed. Rook's textbook of dermatology (9th ed). UK: Wiley Blackwell; 2016. p. :73.1-21.
- [CrossRef] [Google Scholar]
- Combination of the syndrome of Sturge-Weber and the syndrome of Klippel-Trenaunay. Klin Padiatr. 1976;188:464-71.
- [Google Scholar]
- An infantile case of Sturge-Weber syndrome in association with Klippel-Trenaunay-Weber syndrome and phakomatosis pigmentovascularis. J Korean Med Sci. 2005;20:1082-4.
- [CrossRef] [PubMed] [Google Scholar]
- Visual outcome in Sturge-Weber syndrome: A systematic review and Dutch multicentre cohort. Acta Ophthalmol. 2016;94:638-45.
- [CrossRef] [PubMed] [Google Scholar]
- Phakomatosis pigmentovascularis Type IIb, Sturge-Weber syndrome and cone shaped tongue: An unusual association. Indian J Dermatol Venereol Leprol. 2015;81:614-6.
- [CrossRef] [PubMed] [Google Scholar]
- Immunogenicity and safety of biological E's CORBEVAX vaccine compared to COVISHIELD (ChAdOx1 nCoV-19) vaccine studied in a phase-3, single blind, multicentre, randomized clinical trial. Hum Vaccin Immunother. 2023;19:2203632.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical emergence of low-flow vascular malformations after vaccination against SARS-CoV-2: A case series. J Vasc Anom. 2022;3:e049.
- [CrossRef] [Google Scholar]
- COVID-19 Vaccine-related thrombosis: A systematic review and exploratory analysis. Front Immunol. 2021;12:729251.
- [CrossRef] [PubMed] [Google Scholar]
- SARS-CoV-2 vaccination-induced cutaneous vasculitis: Report of two new cases and literature review. Dermatol Ther. 2022;35:e15458.
- [CrossRef] [Google Scholar]
- Primary central nervous system vasculitis In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024.
- [Google Scholar]






