Translate this page into:
Erythema nodosum: A harbinger of Lipschutz ulceration?
*Corresponding author: Tiya Elizabeth John, Department of Dermatology, Venereology and Leprosy, Dr. Somervell Memorial CSI Medical College, Karakonam, Trivandrum, India. tiyaelizabeth@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Joy A, John TE, Samson JF, Philip M. Erythema nodosum: A harbinger of Lipschutz ulceration? J Skin Sex Transm Dis. 2024;6:192-5. doi: 10.25259/JSSTD_25_2024
Abstract
Diagnosis of genital ulcers can be challenging. There are various differential diagnoses including sexually and non-sexually transmitted infections, autoimmune conditions, drug reactions, and as a manifestation of systemic illness. Lipschutz ulcer is a non-venereal genital ulcer, probably an underdiagnosed condition, characterized by acute painful necrotic vulval ulcerations. We report the case of a 45-year-old female with a recurrent history of erythema nodosum (EN) who presented with vulvar ulcers two weeks after an upper respiratory tract infection. Other possible venereal and non-venereal etiologies were ruled out and lesions healed with no sequelae. Through this case report we attempt to increase awareness regarding this uncommon condition and its possible relation to EN, an entity with the same pathophysiology. The diagnostic workup for genital ulcers is extensive, but when correctly identified, treatment and reassurance provide great comfort to the patient.
Keywords
Lipschutz ulceration
Ulcus vulvae acutum
Erythema nodosum
Non-venereal genital ulcers
INTRODUCTION
The presence of an ulcer in the genitalia prompts us to think of a sexually transmitted infection. Although extremely rare, it is important to have a comprehensive approach and consider nonvenereal etiologies as well. Here, we report a case of “ulcus vulvae acutum” associated with erythema nodosum (EN).
CASE REPORT
A 45-year-old female, with a recurrent history of EN (two episodes in the past eight months), presented with an exquisitely painful vulval ulcer for one week. She gave a history of fever, cough, and sore throat two weeks before the appearance of lesions. She also noticed two tender nodules on the legs two days after the onset of genital ulcer. There was no history of recurrent orogenital ulcers, ocular involvement, or joint pain. The patient and her husband affirmed a monogamous relationship with each other. The last unprotected sexual contact was three months back.
The patient had an antalgic gait; local examination revealed a single tender ulcer of size ~1 × 1 cm on the left labia minora with regular edges, erythematous base, and yellowish necrotic debris [Figure 1]. Upon further examination, patient had two tender violaceous nodules over the right shin and medial aspect of the left leg. General and systemic examinations were non-contributory; there was no inguinal lymphadenopathy.

- A single ulcer of size ~1 × 1 cm on left labia minora with regular edges, erythematous base, and yellowish necrotic debris
Blood parameters and urine investigations were normal. Tzanck smear and Gram’s stain were non-specific. Bacterial culture from the ulcer yielded no growth. Herpes simplex virus 1,2 immunoglobulin (Ig)M and IgG, Human Immunodeficiency Virus, Hepatitis B, Hepatitis C serology, and Venereal Disease Research Laboratory test in dilution were negative. Skin pathergy test was performed and no lesions were induced. Herpes simplex virus 1,2 IgM and IgG were repeated after two weeks which remained negative. Skin punch biopsy of the skin nodule showed septal panniculitis which was consistent with EN [Figure 2]. All possible etiologies for infective genital ulcer and recurrent EN were ruled out [Table 1].
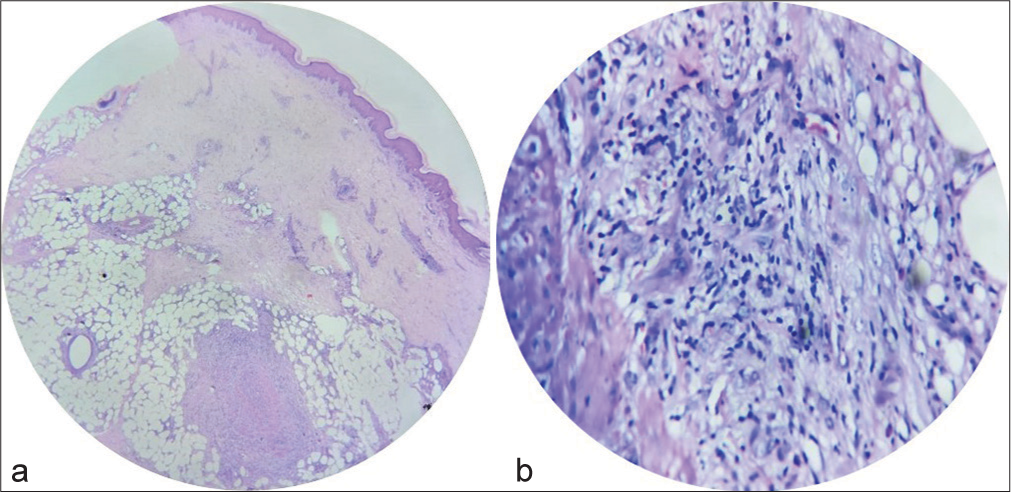
- Punch biopsy from skin nodule (a): Scanner view (Hematoxylin and eosin stain, ×4) showing septal panniculitis; (b): High power view (Hematoxylin and eosin stain, ×40) showing inflammatory infiltrate of neutrophils, epithelioid cells and multinucleate giant cells with septal panniculitis.
| Blood investigations | Normal |
| Urine routine and microscopy | Normal |
| Gram’s stain | Negative |
| Tzanck smear | Negative |
| Bacterial culture from the ulcer | No growth |
| Herpes Simplex Virus 1,2 IgM and IgG (repeated at 2 weeks) | Negative |
| Human Immunodeficiency Virus, Hepatitis B, Hepatitis C serology | Negative |
| VDRL in dilution | Negative |
| Pathergy test | Negative |
| Antinuclear antibody | Negative |
| Mantoux | Negative |
| Antistreptolysin O titer | Normal |
| Chest Xray | No significant abnormality |
| Skin punch biopsy of erythema nodosum | Septal panniculitis |
VDRL: Venereal disease research laboratory, Ig: Immunoglobulin
Since the patient was extremely symptomatic, she was managed empirically with systemic antibiotics (injection ceftriaxone) and antivirals (tablet acyclovir) along with topical anesthetics and systemic analgesics while awaiting reports of the investigations. Considering herpes genitalis to be one of the most common causes of painful genital ulcers in a sexually active woman, she was started on antivirals. Systemic antibiotics were started as the ulcer had yellowish necrotic debris on the floor. Despite the above treatment patient showed no improvement. Two more smaller ulcers developed four days later.
Based on history, clinical presentation, exclusion of venereal and non-venereal etiologies, and non-responsiveness to usual treatment modalities, a diagnosis of Lipschutz ulcera was considered. The ulcers resolved completely after three weeks [Figure 3]. One month after healing of the Lipschutz ulcer, she had another episode of EN. All the relevant investigations were again carried out to find a cause for the recurrent EN, but none yielded any evidence of a specific cause. Our patient is being followed up for the past six months.
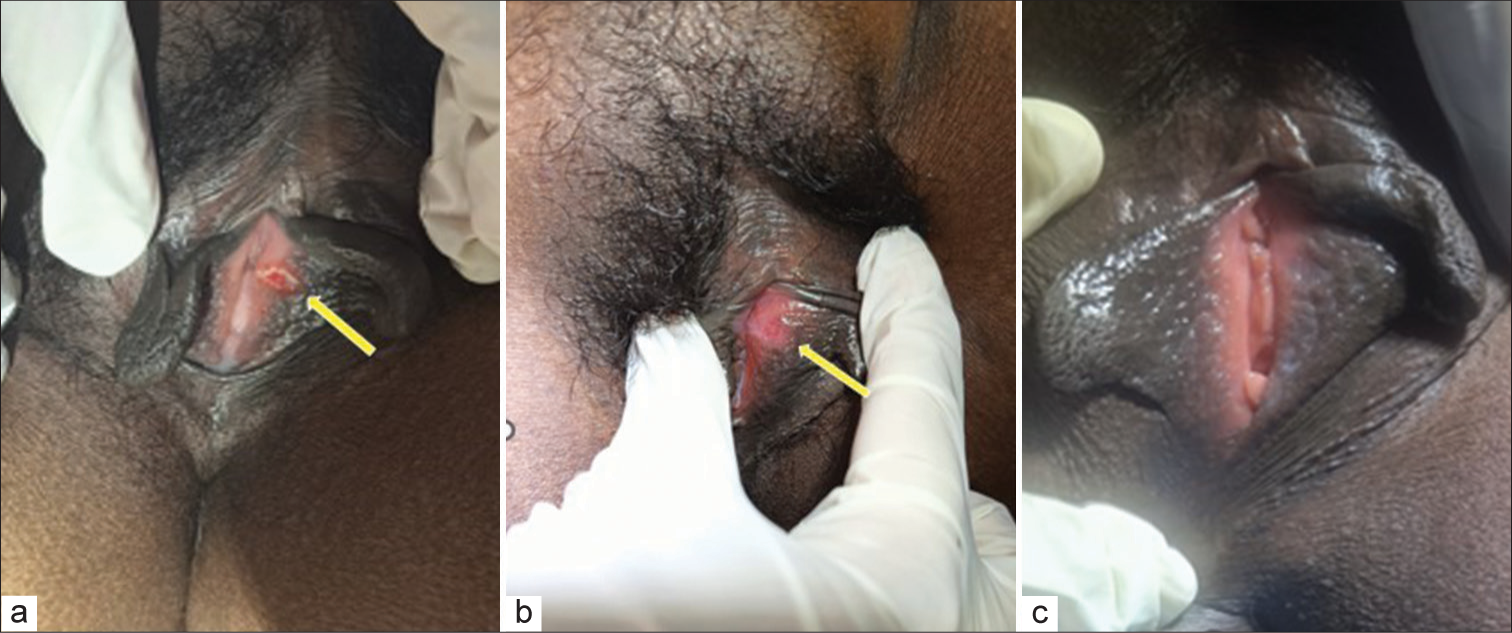
- The ulcer (yellow arrow) at (a): Presentation; (b): After 2 weeks; (c): After 3 weeks.
DISCUSSION
Lipschutz ulcers are acute onset multiple painful ulcers with erythematous border and necrotic center, common in adolescent females, though it is reported in different age groups.[1,2]
Probable etiology is hypersensitivity to viral or bacterial infection, leading to deposition of immune complexes in dermal vessels, which activates the complement system, resulting in microthrombi formation leading to deep, necrotizing, painful ulcers.[3] Organisms implicated include Epstein–Barr virus, cytomegalovirus, group A Streptococcus, toxoplasmosis, influenza A virus, and Mycoplasma pneumonia.[4] In most cases, the association with infection could not be confirmed. Ulcers resolve spontaneously in two to six weeks. Recurrence is uncommon.[5]
Lipschutz ulcer is a diagnosis of exclusion. Histologic examination is not of diagnostic value as it is non-specific.[3] Based on the literature, major and minor criteria are devised for the diagnosis. Both major and at least two minor criteria are required for diagnosis.[6,7] Our patient fulfilled two major and three minor criteria.
Major criteria
Acute onset of one or more painful ulcers in the vulvar region
Exclusion of infectious and other non-infectious causes.
Minor criteria
Localization of ulcer at vestibule or labia minora
No sexual intercourse ever or within the past 3 months
Flu-like symptoms
Systemic infection within two to four weeks before the onset of vulvar ulcer.
Management includes symptomatic treatment with topical anesthetics and oral analgesics.
Topical and systemic corticosteroids further aid in ulcer healing.[8]
EN is the prototypic septal panniculitis[9] seen in women during the second and fourth decade. It is characterized by tender, erythematous nodules, and plaques, over the extensor aspect of lower extremities with bruise-like changes on regression. It subsides in three to six weeks without scarring. It is a hypersensitivity to antigenic stimuli leading to immune complex formation and deposition in septal venules of subcutaneous fat.[8] Multiple treatments suggested include compression bandage and limb elevation, potassium iodide, non-steroidal anti-inflammatory drugs, and corticosteroids.[9] Few cases suggesting the existence of skin nodules similar to EN and Lipschutz ulcers are reported.[10]
CONCLUSION
After a thorough literature review, we could see that a reactive dermatosis following an upper respiratory tract infection, though not so uncommon, the occurrence of two reactive dermatoses of which one is extremely rare (Lipschutz ulcer) is unreported. The presence of two immune complex-mediated diseases in the same person within a short span, with neither having an identifiable cause and both resolving without specific treatment justifies our doubt that EN and Lipschutz ulcerations are related entities warranting follow-up.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Joan Felicita Samson is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Lipschütz ulcers: Should we rethink this? An analysis of 33 cases. Eur J Obstet Gynecol Reprod Biol. 2016;198:149-52.
- [CrossRef] [PubMed] [Google Scholar]
- Reactive nonsexually related acute genital ulcers. J Gen Fam Med. 2017;19:30-1.
- [CrossRef] [PubMed] [Google Scholar]
- Lipschütz ulcer: An unusual diagnosis that should not be neglected. Rev Bras Ginecol Obstet. 2021;43:414-6.
- [CrossRef] [PubMed] [Google Scholar]
- Lipschütz ulcers: Classic presentation of an uncommon condition. Available from: https://www.cureus.com/articles/148325-lipschtz-ulcers-classic-presentation-ofan-uncommon-condition [Last accessed on 2024 Apr 08]
- [Google Scholar]
- Erythema nodosum: A practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-78.
- [CrossRef] [PubMed] [Google Scholar]
- Non-sexually related acute genital ulcers in 13 pubertal girls: A clinical and microbiological study. Arch Dermatol. 2009;145:38-45.
- [CrossRef] [PubMed] [Google Scholar]







