Translate this page into:
Multifocal infantile hemangiomas in a 4-month-old female infant
*Corresponding author: Linza P. Zachariah, Department of Dermatology, Government Medical College, Thrissur, Kerala, India. linzajojy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Zachariah LP, Prathap P, Asokan N, Zacharia T. Multifocal infantile hemangiomas in a 4-month-old female infant. J Skin Sex Transm Dis 2024;6:93-5. doi: 10.25259/JSSTD_62_2023
Dear Editor,
Infantile hemangioma (IH) is the most frequent benign tumor of infancy (with a 3–10% prevalence among newborns) and is more common among girls.[1] Multifocal IH constitutes about 3.6% of all IH.[1]
A 4-month-old female infant presented with asymptomatic discrete reddish raised lesions on the face, trunk, and extremities, noticed one month after birth. Initially, the skin lesions were flat and became raised gradually over three months, along with the appearance of new lesions. There was no history of bleeding or oozing from the lesions.
The baby was born by lower segment cesarean section at 32 weeks of gestation due to fetal distress. Her mother had systemic lupus erythematosus, class 3 lupus nephritis, and expired immediately after delivery due to left ventricular failure. There was no history suggestive of TORCH infections for the mother during pregnancy.
The birth weight of the baby was 1.52 kg. She was admitted to the newborn intensive care unit for prematurity and small for gestational age. She was given formula feeds and gradually gained normal weight. Neck fixation was attained normally at 3rd month. There was no history of seizures.
On examination, the baby was active and playful. There were 12 discrete, partially blanching, reddish, non-tender papules of size varying from 1 mm to 4 mm on the face, trunk, and limbs [Figure 1]. Dermoscopy showed reddish lacunae and cerebriform appearance on a pinkish background [Figure 2]. There were no mucosal lesions. The ophthalmological examination was normal. Systemic examination was normal. There was no hepatosplenomegaly, no tenderness or swellings on the bones, and the joints were normal.

- Reddish, non-tender, partially blanching papules.
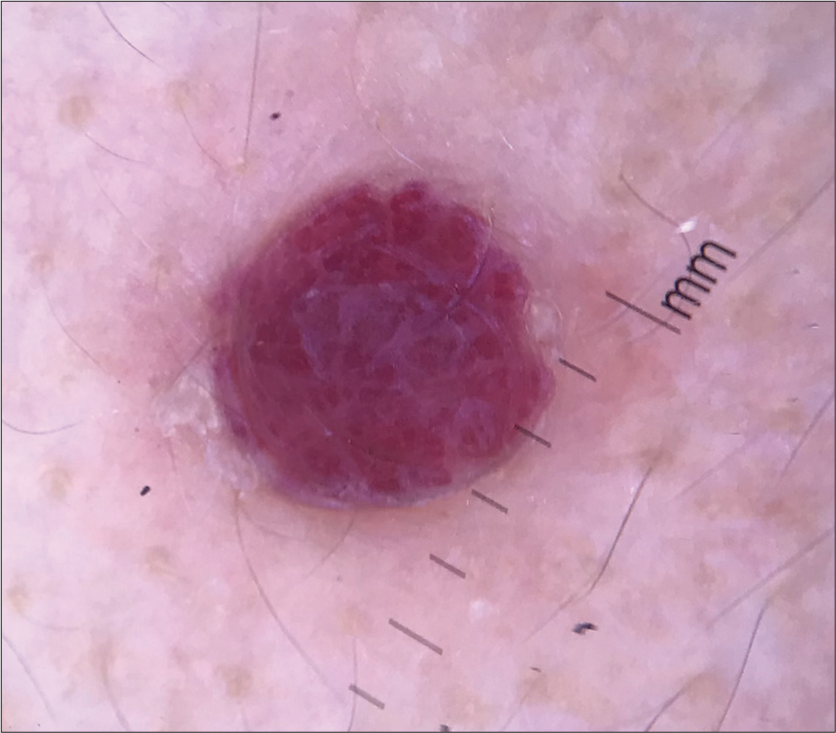
- Reddish lacunae and cerebriform appearance on a pinkish background on dermoscopy.
Clinical possibilities of multifocal IHs, blueberry muffin lesions, juvenile xanthogranulomas, and Langerhans cell histiocytosis were considered [Table 1]. Complete blood count, platelet count, bleeding time, clotting time, peripheral smear, liver and renal function tests were within normal limits. TSH was elevated (10 mIU/L). Free T3 and T4 were normal. Subclinical hypothyroidism was considered. Anti–Ro antibody was positive in the ANA profile. There was no evidence of heart block in the electrocardiogram. Echocardiography was normal. Immunoglobulin G and immunoglobulin M antibodies against TORCH infections were negative. Ultrasound of the abdomen was normal; there were no hemangiomas in the liver and no hepatosplenomegaly. Histopathological examination revealed multiple lobules composed of plump endothelial cells lining vascular spaces with inconspicuous lumens and endothelial cell proliferation in the dermis, suggestive of IH [Figures 3a and b]. We could not do GLUT-1, which is the specific marker of IH, due to financial constraints. Vascular markers, CD 31 and CD 34 were positive [Figures 4a and b].
| Differential diagnosis | Clinical features | Histopathology | Dermoscopy |
|---|---|---|---|
| Blueberry muffin lesions | Erythematous or purple macules, papules, and nodules in the skin | Foci of dermal erythropoiesis | Fine telangiectatic arborizing vessels distributed within a pink background |
| Multifocal infantile hemangioma | Multiple, discrete, partially blanching reddish papules | Lobules with plump endothelial cells and endothelial cell proliferation | Reddish lacunae and cerebriform appearance |
| Juvenile xanthogranuloma | Reddish yellow single to multiple papules | Histiocytes in the dermis and Touton giant cells | Setting sun: central yellowish area surrounded by a reddish periphery |
| Langerhans cell histiocytosis (Hand-Schuller-Christian disease) | Yellow-brown nodules or tumors Associated with lytic bone lesions, exophthalmos, diabetes insipidus |
Langerhans cells along the epidermal-dermal junction | Vascular blotch, brown homogenous area, absence of dotted and non-dotted vessels. |
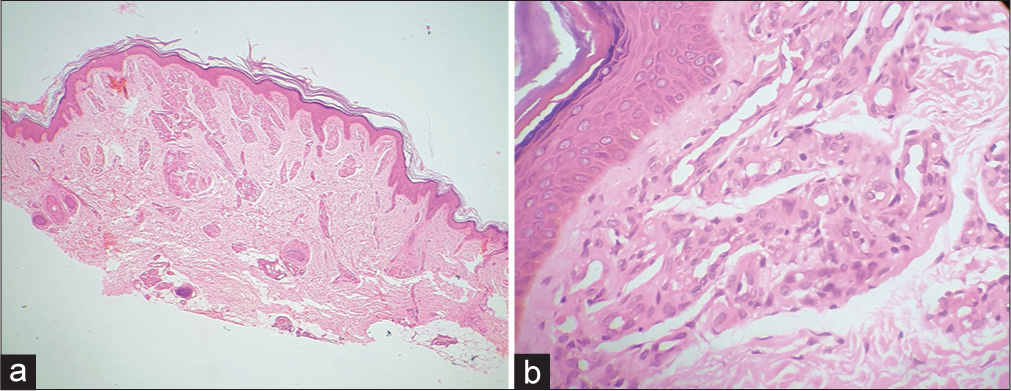
- Multiple lobules composed of plump endothelial cells lining vascular spaces with inconspicuous lumens and endothelial cell proliferation in the dermis. (a): Hematoxylin and eosin ×40; (b): Hematoxylin and eosin ×400.
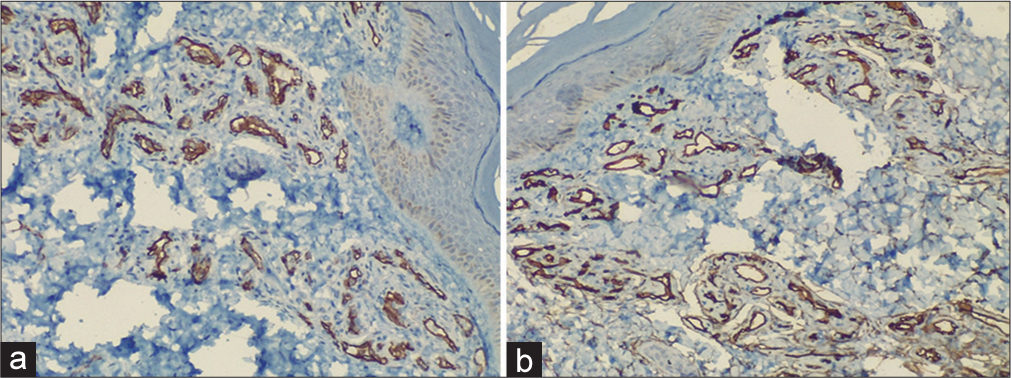
- (a): Immunohistochemistry (IHC): CD 31 positive; (b): IHC: CD 34 positive.
A final diagnosis of multifocal IHs was made based on the following features: The appearance of multiple hemangiomas on multiple sites of the skin soon after birth, with a gradual increase in size and number; suggestive features on histopathology and immunochemistry markers of skin lesions.
IHs are classified based on pattern into focal, multifocal, segmental, and indeterminate. The precursor lesions are telangiectasias and ecchymosis. Residual lesions include telangiectasia, scarring, pigment changes, fibrofatty tissue, and atrophic skin. Multifocal IH is multiple discrete focal IHs, usually more than five in number, and they occupy different anatomic sites. It is often associated with hemangiomas in other organs, especially the liver. The complications are high-output cardiac failure and obstructive jaundice.[2]
Prematurity and low birth weight can lead to tissue hypoxia, which, in turn, can trigger disordered angiogenesis mediated by elevated vascular endothelial growth factor.[3] Prematurity and low birth weight might have predisposed to the occurrence of multiple IHs in our child.
Although the Anti-Ro antibody was positive in our child, there were no other features to suggest neonatal lupus erythematosus. Multifocal IHs have also been described in neonatal lupus.[4] Elevated TSH may occur as a part of consumptive hypothyroidism due to increased levels of catalysts of thyroidinactivating enzymes. It is usually seen in hepatic hemangiomas and reported in cutaneous hemangiomas also.[5]
Treatment of IH depends on the location, morphology, stage of evolution, impact on function, risk of disfigurement, and comorbidities related to IH.[6] Topical treatment options are timolol maleate 0.5% eye drops and becaplermin gel (recombinant human platelet-derived growth factor). Becaplermin gel is indicated in ulcerated IH. In a study conducted among 724 children with superficial IH, topical timolol was noted to be as effective as oral propranolol.[7] Oral propranolol is administered as 1–3 mg/kg/day divided into three equal doses until the clearance of IH with regular cardiac monitoring.[8] The mechanisms of action of propranolol are inducing vasoconstriction, apoptosis of endothelial cells, and curbing of angiogenesis. Timolol and propranolol are beta blockers. The R (+) enantiomers of β-blockers, which could increase the efficacy of IH management with fewer adverse effects, are being researched.[9] Indications for pulsed dye laser in IH are ulcerations, post–involution telangiectasis, and erythema. Though multifocal IH has a benign histology, prognosis is determined by the extent of visceral involvement.
Our patient was treated with timolol maleate 0.5% eye drops, one drop on each lesion twice daily. A marked response was noted about three months after therapy. Although extracutaneous hemangiomas were not detected in our baby, follow-up is necessary.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr Neelakandhan Asokan is on the editorial board of the journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Multifocal infantile haemangioma: A diagnostic challenge. BMJ Case Rep. 2016;2016:bcr2016214827.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features and management of multifocal hepatic hemangiomas in children: A retrospective study. Sci Rep. 2016;6:31744.
- [CrossRef] [PubMed] [Google Scholar]
- Association of infantile hemangiomas and retinopathy of prematurity: Analysis of the multicenter KID. Biomed Hub. 2022;7:24-30.
- [CrossRef] [PubMed] [Google Scholar]
- Infantile haemangioma with neonatal systemic lupus erythematosus, rare combination, case report and review of literature. Experience from King Abdulaziz Medical City. Riyadh Saudi Arabia: Acad J Ped Neonatol. 2019;7:555772.
- [CrossRef] [Google Scholar]
- Spontaneous regression of severe acquired infantile hypothyroidism associated with multiple liver hemangiomas. Pediatrics. 2003;112:1424-26.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of infantile hemangiomas in the neonate. Pediatr Clin North Am. 2019;66:437-59.
- [CrossRef] [PubMed] [Google Scholar]
- Topical timolol vs. Oral propranolol for the treatment of superficial infantile hemangiomas. Front Oncol. 2018;8:605.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical practice guideline for the management of infantile hemangiomas. Pediatrics. 2019;143:e20183475.
- [CrossRef] [PubMed] [Google Scholar]
- Non-beta blocker enantiomers of propranolol and atenolol inhibit vasculogenesis in infantile hemangioma. J Clin Invest. 2022;132:151109.
- [CrossRef] [PubMed] [Google Scholar]





