Translate this page into:
Patchy alopecia in a young male: Trichoscopy to the aid
-
Received: ,
Accepted: ,
How to cite this article: Bhatia S, Prabhu S. Patchy alopecia in a young male: Trichoscopy to the aid. J Skin Sex Transm Dis 2019;1:38-40.
Sir,
Dermoscopy or epiluminescence microscopy was initially described in the early years of 20th century. By 1990s, handheld dermoscopes were introduced widely in dermatological practice for easy distinction of melanoma from non-melanomatous pigmented lesions. However, it soon grew popular and the use is now extended to other conditions too.[1]
Due to the wide range of conditions, where dermoscopy has found use as a diagnostic tool, different names such as trichoscopy, onychoscopy, inflammoscopy, and entomoscopy are used depending on etiology of the condition and the site examined.
Dermoscopy is found to be useful in diagnosing superficial mycoses as well. Worldwide, superficial mycoses are on the rise and are often presenting with atypical manifestations. When in doubt, the most common diagnostic test performed is skin scraping for KOH mount examination which reveals fungal hyphae and spores and Wood’s lamp examination which reveals fluorescence in certain species causing Tinea capitis. Although Wood’s lamp is not time-consuming, fluorescence can be false negative if the skin has been washed or cleaned. KOH mount is time-consuming and semi-invasive. Dermoscopy may be an easy, cost-effective, and time-saving alternative for the diagnosis of superficial mycosis.
Here, we describe the utility of a handheld dermoscope in almost instantaneous and definitive diagnosis of patchy alopecia in a 10-year old boy who presented with occasionally itchy and patchy hair loss over the occipital scalp of 4 months duration. He did not have any other skin lesions. The child as well as his parents denied a history of intentional hair pulling or any stressful events recently.
On examination, there was a single patch of hair loss measuring approximately 5 cm × 5 cm on the left side of the suboccipital area with mild scaling. Hair shafts within the patch were of varying lengths. [Figure 1] There was no lymphadenopathy. Our provisional diagnosis was alopecia areata, trichotillomania, and tinea capitis. Wood’s lamp examination was inconclusive showing doubtful fluorescence. [Figure 2] Direct microscopic examination of hair as well as examination of scrapings from affected area of scalp in 10% KOH were negative for fungus. A specimen was sent for fungal culture.
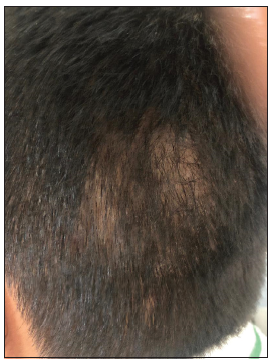
- Patchy hair loss with minimal scaling in a 10-year-old boy.
- Wood’s lamp showing inconclusive fluorescence.
Dermoscopic examination using DermLite DL4 with ×10 magnification revealed multiple black dots, broken hair, corkscrew hair, scaling, hair casts, and morse code hair which confirmed the diagnosis of tinea capitis and excluded alopecia areata and trichotillomania which have characteristic dermoscopic findings [Figure 3]. The child was prescribed topical sertaconazole lotion twice daily with an antifungal shampoo for scalp wash. At 2 weeks’ review, he had clinically improved, [Figure 4] but dermoscopy still showed the same features [Figure 5]. The culture was positive for Trichophyton rubrum and he was started on oral itraconazole 100 mg twice daily for 4 weeks.
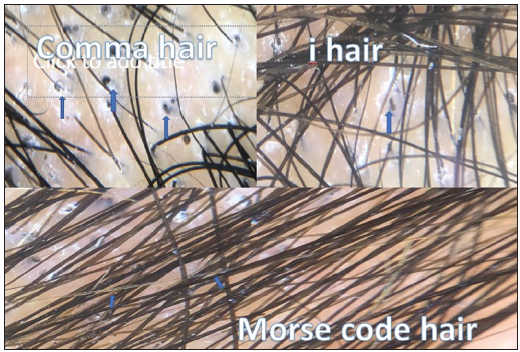
- Trichoscopy showing scaling, black dots, comma hair, I hair, and Morse code hair.

- Clinical picture at 2-week follow-up showing resolving lesions.
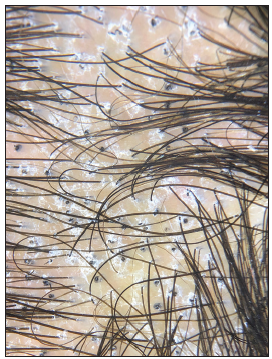
- Trichoscopy at 2-week follow-up showing persistent scaling, black dot, and corkscrew hair.
Patchy or diffuse hair loss in children is not uncommon and may exhibit various symptoms such as pruritus, scaling, and erythema depending on the underlying cause, the common ones being tinea capitis, alopecia areata, trichotillomania, telogen effluvium, and tractional alopecia.[2,3]
Tinea capitis is an infection of hair and/or scalp caused by dermatophytes, which include Trichophyton violaceum, Trichophyton rubrum, Trichophyton tonsurans, Trichophyton verrucosum and Microsporum audouinii.[4,5] It is commonly seen in children in the age group of 3–7 years.[2,4,5] It can be transmitted through close contact by sharing combs, brushes, or linen and through inoculation due to trauma.
Tinea capitis can be classified into inflammatory and non-inflammatory types. Inflammatory tinea capitis comprises of kerion and favus, whereas non-inflammatory types are black dot and gray patch.[4] Different species of Trichophyton and Microsporum are found to be the causative agents. Studies done in both North India and South India have shown a predominance of Trichophyton violaceum.[4,5]
Patients present with patchy areas of hair loss with scaling, numerous broken off-dry, lusterless gray hair (in gray patch), or multiple hairs broken off at the level of scalp (in black dot variant). Inflammatory lesions usually comprise of boggy inflammatory nodular swelling in case of kerion and a yellow cup-shaped crust in favus type.
Diagnosis can be made with the aid of multiple modalities such as direct microscopic examination, mycological cultures, Wood’s lamp, and dermoscopy.
Direct microscopic examination is done with the help of 10% KOH mount which reveals spores and hyphae.
Dermatophytes can be easily grown on Sabouraud dextrose agar, though it takes weeks for the fungal growth and can be negative at times due to factors such as previous administration of medications or by faulty technique.[6]
Wood’s lamp examination can be helpful in cases of Microsporum and some Trichophyton species and would show a blue-green fluorescence.[7] In our case, we noticed a doubtful fluorescence.
Trichoscopy is a non-invasive and handy aid for quick diagnosis of tinea capitis and also helps in differentiating it from close mimics such as alopecia areata and trichotillomania.[8] In recent years, characteristic dermoscopic findings have been described in tinea capitis. At low magnification (×30), comma hair, corkscrew hair, zigzag hair, pigtail hair, and morse code hair are usually seen. Scaling, hair casts, and blotchy pigmentation are associated findings. At higher magnification (×150), horizontal white bands, bent and broken hair, and translucent deformable hair are observed. Short broken hairs are seen as irregularly distributed and shaped black dots.[9,10] Morse code is a rare and new dermoscopic feature which was observed in our case. It shows alternate white bands which corresponds to the localized area of fungal infection.[6,8] In addition, our findings included black dots, broken hairs, scaling, comma, and I hair.
Dermoscopic findings in trichotillomania would be the hair shaft damage observed as frayed hair of different lengths resembling tulip hair, broom hair, pigtail hair, flame hair, and irregular black dots along with extravasations and hemorrhages. Red dots corresponding to follicular microhemorrhages also may be seen.
In alopecia areata, cadaverised hairs seen as regular black dots admixed with yellow dots, which are dilated follicular infudibula filled with sebum, are seen. Tapering hair or exclamation mark hair and straight transverse hair are also seen. Regrowing tufts of short vellus hair are additional findings. Of these, regular black dots and tapering hairs are the most specific findings, whereas yellow dots correspond to disease severity.[11]
The mainstay of treatment of tinea capitis is the administration of oral antifungals such as griseofulvin and itraconazole, along with maintenance of local care and hygiene.
Trichoscopy, with its definite positive findings, aided us in early treatment of the child.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The scope of the dermoscope. Indian Dermatol Online J. 2016;7:359-63.
- [CrossRef] [PubMed] [Google Scholar]
- Hair loss in children: Common and uncommon causes; Clinical and epidemiological study in Jordan. Int J Trichol. 2013;5:185-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of alopecia in children. Pediatr Clin North Am. 2014;61:427-2.
- [CrossRef] [PubMed] [Google Scholar]
- Tinea capitis in the pediatric population: A study from north India. Indian J Dermatol Venereol Leprol. 2010;76:527-32.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical study of tinea capitis in Northern Karnataka: A three year experience at a single institute. Indian Dermatol Online J. 2013;4:226.
- [CrossRef] [PubMed] [Google Scholar]
- Tinea capitis in children: A report of four cases trichoscopic with trichoscopic features. Indian J Paediatr Dermatol. 2018;19:51-6.
- [CrossRef] [Google Scholar]
- Idiosyncratic findings in trichoscopy of tinea capitis: Comma, zigzag hairs, corkscrew, and morse code-like hair. Int J Trichol. 2016;8:180-3.
- [CrossRef] [PubMed] [Google Scholar]
- Newly described features resulting from high-magnification dermoscopy of tinea capitis. JAMA Dermatol. 2015;151:308-10.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy findings in tinea capitis: Case report and literature review. Ann Bras Dermatol. 2012;87:313-4.
- [CrossRef] [Google Scholar]
- Trichoscopy in alopecias: Diagnosis simplified. Int J Trichol. 2013;5:170-8.
- [CrossRef] [PubMed] [Google Scholar]





