Translate this page into:
Plasma cell gingivitis – An enigma
*Corresponding author: Anju Joseph, Department of Dermatology Venereology and Leprosy, Pushpagiri Institute of Medical Sciences and Research Centre, Tiruvalla, Kerala, India. anjujoseph5991@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Joseph A, Pappen TT, Mathew L, Anjana JP. Plasma cell gingivitis – An enigma. J Skin Sex Transm Dis. 2024;6:167-9. doi: 10.25259/JSSTD_6_2024
Abstract
Plasma cell gingivitis (PCG) is a rare benign inflammatory disorder affecting the gingiva characterized by dense infiltration of plasma cells into the sub-epithelial connective tissue. It is considered a hypersensitivity reaction to various allergens; thus, the first step in management is to remove the causative factor. We are reporting a case of a 73-year-old male who presented with redness and swelling of upper gums, which bleeds easily on probing. The final diagnosis of PCG was confirmed by histology and immunochemistry. In this article, we report a rare case of PCG.
Keywords
Plasma cell gingivitis
Plasma cells
Gingiva
INTRODUCTION
Plasma cell infiltrates can present in the connective tissue in various conditions and it was documented by Zoon in 1952.[1] A rare benign gingival disorder known as plasma cell gingivitis (PCG) is characterized by well defined erythematous, edematous gingivitis which frequently extends to the mucogingival junction. As the name implies, there is a diffuse and extensive infiltration of plasma cells into the sub-epithelial gingival tissue.[2]
Histologically, lesions can resemble multiple myeloma and extramedullary plasmacytoma, as well as acute leukemia. As a result, hematological screening is necessary for the diagnosis in addition to clinical and histological analyses. The condition known as PCG is entirely benign and will improve the removal of the causative factor. Even with rigorous allergy testing, the allergen often remains unknown.[3]
CASE REPORT
The gingiva in a 73-year-old male appeared bright red, friable, and edematous in the vicinity of the upper central and lateral incisors over the previous two months. It was associated with bleeding on provocation. He noticed a gradual increase in the size of the gums to its present size. He had a history of using herbal toothpaste for the past few years. The patient’s medical history was unremarkable. The patient was prescribed antibiotics one month before, but with no improvement. Dermatological examination showed sharply demarcated erythematous gingival hyperplasia of the upper gums near the upper incisors, which easily bled on probing [Figure 1]. Peripheral blood smear showed mild erythrocytosis. No immature or abnormal cells were noted.

- Gingiva appears fiery red and friable with an edematous consistency near the upper central and lateral incisors.
An incision biopsy of the upper maxillary gingiva showed mild hyperkeratosis, hyperplasia, and focal ulceration. Subepithelium shows diffuse dense plasmacytic infiltrate along a few lymphocytes [Figures 2 and 3]. Immunohistochemistry with CD138 was positive. Plasma cells didn’t show clonality of either kappa or lambda chains on histo chemical staining. Sections showed no abnormal or malignant cells. These features were suggestive of PCG [Figure 4].
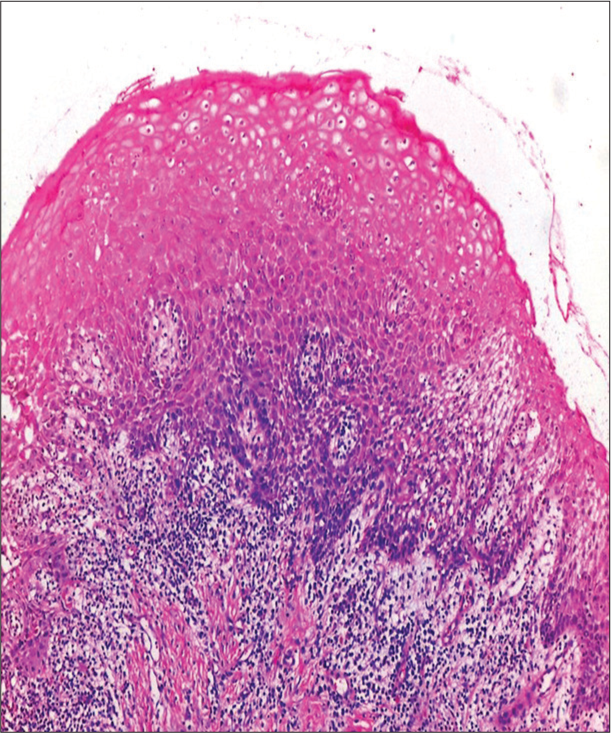
- Upper maxillary gingiva shows mild hyperkeratosis, hyperplasia, and focal ulceration. Hematoxylin and eosin, 10×.
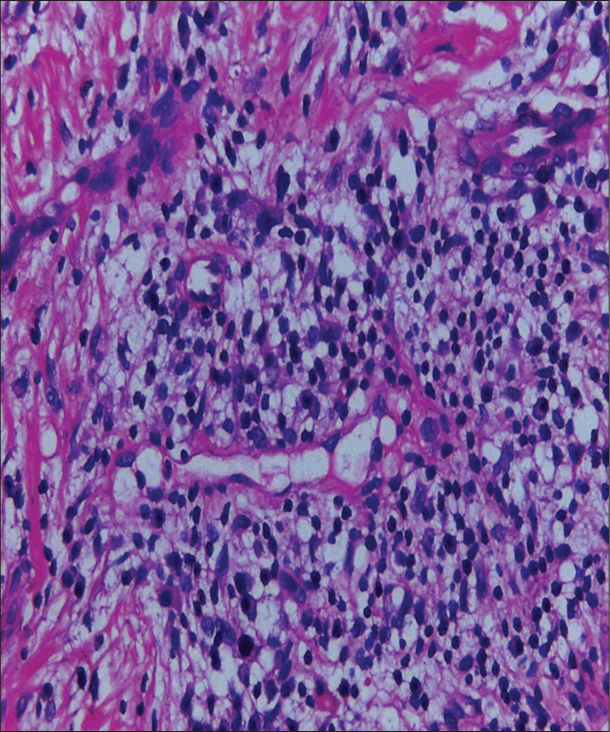
- Plasma cell with a characteristic eccentrically placed nucleus and abundant cytoplasm with few lymphocytes. Hematoxylin and eosin, 40×.
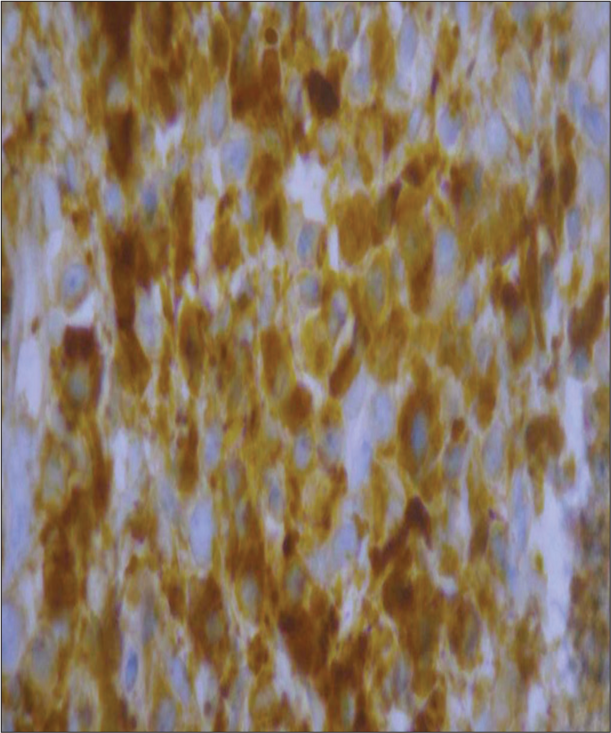
- Immunohistochemistry shows CD 138 positive for plasma cells with no evidence of monoclonality of light chains (40×).
The patient was advised to stop using herbal toothpaste and to practice strict oral hygiene. Dental scaling was done. He was advised steroid gargle thrice daily for six weeks, along with oral antihistamines, which provided significant relief.
DISCUSSION
PCG is a benign disorder caused by the infiltration of plasma cells, most commonly found in old age.[3] Some other names include atypical gingivostomatitis, idiopathic gingivostomatitis, soft-tissue plasmacytosis, stomatitis venenata, and irritating contact stomatitis.[4] Examination reveals a diffuse red gingival swelling in the anterior maxillary and mandibular gingival margin across its width. The exact mechanism behind this reaction is uncertain, but it is thought to be a hypersensitive reaction.[5]
PCG can be classified into three categories based on etiology: Unknown origin, neoplastic origin, and allergens and these are classified type 1 to 3. The most common causes are cinnamon, red pepper, chewing gums, specific components of toothpaste, etc.[5] Based on the previously indicated categorization, a Type 1 PCG is discussed in this case. Kerr et al. reported a case in which chewing gum’s cinnamaldehyde was the cause. When these gums were stopped, the problem fully reversed.[6] Plasma cell gingivostomatitis, as defined by Silverman and Lozada, is a condition that includes gingivitis, cheilitis, and glossitis.[7] Although Dhir et al. proposed Candida albicans as an etiological agent, it was ruled out in this patient.[8]
The various differential diagnoses of this presentation were PCG, erosive lichen planus, and plaque-induced gingivitis. This case report presents pronounced erythematous enlargement of the maxillary region covering almost complete width till the mucogingival junction, whereas plaque-induced gingivitis would only involve the marginal gingiva. In the present case, gingiva responded to local therapy but it did not resolve completely, whereas plaque-induced gingivitis would have resolved entirely.[9] The absence of saw-toothed ridges and a band-like lymphocytic infiltrate at the dermo-epidermal junction on histopathology excludes the diagnosis of erosive lichen planus. The other differentials that can be included are myeloma and leukemia which can be excluded by investigations.[10] The first step in treating the issue is figuring out the cause, and avoiding it. Despite using several techniques such as liquid nitrogen, carbon dioxide laser, electrocoagulation, topical, intralesional, systemic corticosteroids, antibiotics, and radiation therapy, no single treatment is proved consistently useful.[3]
CONCLUSION
We report a case of plasma cell Gingivitis a less often detected condition which responded to avoidance of possible provocative factor including herbal tooth paste.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Chronic benign circumscript plasmacytic balanoposthitis. Dermatologica. 1952;105(1):1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell gingivitis. J Indian Soc Periodontol. 2015;19:221-3.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell gingivitis associated with cheilitis: A diagnostic dilemma! J Indian Soc Periodontol. 2012;16:115-9.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell gingivitis among herbal toothpaste users: A report of three cases. J Contemp Dent Pract. 2007;8:60-6.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic gingivostomatitis (due to gum chewing) J Periodontol. 1971;42:709-12.
- [CrossRef] [PubMed] [Google Scholar]
- An epilogue to plasma-cell gingivostomatitis (allergic gingivostomatitis) Oral Surg Oral Med Oral Pathol. 1977;43:211-7.
- [CrossRef] [PubMed] [Google Scholar]
- The plasma cell gingival enlargement: The diagnostic and esthetic concerns. Indian J Oral Sci. 2012;3:117.
- [CrossRef] [Google Scholar]
- Plaque-induced gingivitis: Case definition and diagnostic considerations. J Clin Periodontol. 2018;45(Suppl 20):S44-67.
- [CrossRef] [Google Scholar]
- Plasma cell gingivitis-a conflict of diagnosis. J Clin Diagn Res. 2016;10:D01-3.
- [CrossRef] [PubMed] [Google Scholar]






