Translate this page into:
Pyoderma gangrenosum with Marfan syndrome and Crohn’s disease: A rare association
*Corresponding author: Pradeep S. Nair, Department of Dermatology and Venereology, Government Medical College, Thiruvananthapuram, Kerala, India. dvmchtvm@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Dhanesh D, Jayapalan S, Nair PS, Sudhesan A. Pyoderma gangrenosum with Marfan syndrome and Crohn’s disease: A rare association. J Skin Sex Transm Dis 2024;6:83-6. doi: 10.25259/JSSTD_20_2023.
Abstract
A 22-year-old man presented with multiple, painful ulcers on the thighs, legs, and face of 10-day duration and diarrhea and bleeding per rectum of 2-year duration. The ulcers were tender and had a peripheral violaceous border. General examination revealed tall stature, long extremities, kyphosis, arachnodactyly, and hyperextensible wrist and thumbs. The arm span was more than the height and the thumb sign and wrist sign were positive, diagnostic of Marfan syndrome. Skin biopsy from the edge of the ulcer showed infiltrates of neutrophils and lymphocytes in the dermis and subcutaneous tissue. A detailed evaluation ruled out other causes for skin ulceration and we made a diagnosis of pyoderma gangrenosum. Echocardiogram demonstrated mitral valve prolapse. Computed tomography of abdomen showed segmental mucosal thickening as skip lesions in the colon and rectum. Endoscopy showed chronic colitis with multiple punched out ulcers. Colonic biopsy showed noncaseating granulomas suggestive of Crohn’s disease. Although inflammatory bowel disease is a well-known association of pyoderma gangrenosum, we did not come across any previous reports of coexistence of pyoderma gangrenosum, Crohn’s disease, and Marfan syndrome.
Keywords
Marfan syndrome
Pyoderma gangrenosum
Crohn’s disease
INTRODUCTION
Pyoderma gangrenosum is a non-infectious, inflammatory, and neutrophilic dermatosis.[1] It often manifests as a painful furuncle or pustule that ruptures to form a rapidly spreading ulcer. Apart from the ulcerative variant, the other subtypes of pyoderma gangrenosum observed are bullous, vegetative, pustular, peristomal, and superficial granulomatous pyoderma gangrenosum. Pyoderma gangrenosum is a diagnosis of exclusion. In 50% cases, it is associated with systemic diseases such as inflammatory bowel disease, hematologic malignancy, rheumatoid arthritis, and monoclonal gammopathies.[1]
Marfan syndrome, a connective tissue disorder with autosomal dominant inheritance, presents with minimal skin lesions and severe systemic disorders, which primarily affects the bones, eyes and cardiovascular system.[2] The condition is now classified as a fibrillinopathy with heterozygous mutation in the profibrillin gene 1 (FBN1).[3] Involvement of cardiac valves, aorta, lungs, bones, and eyes contributes to morbidity and mortality.[2] The skin lesions are considered as minor criteria according to the revised criteria for diagnosis.[4] Here, we report a case of pyoderma gangrenosum in association with Crohn’s disease and Marfan syndrome.
CASE REPORT
A 22-year-old man presented with multiple, painful ulcers on the thighs, legs, and face of 10-day duration. The lesions first started as painful pustules and rapidly evolved into ulcers. There was no history of drug intake or systemic symptoms. The patient gave a history of reduced appetite and lack of sleep. He also gave a history of bleeding per rectum with lactose intolerance and bouts of diarrhea for the past 2 years.
General examination revealed tall stature (height 176 cm), long extremities, kyphosis, low body mass index (body mass index 11.6 kg/m2, body weight 36 kg), pallor, Grade 2 clubbing, and cervical and inguinal lymphadenopathy. Dermatological examination revealed multiple, discrete, and well-defined ulcers on the anterior aspect of thighs, anterior aspect of the right lower leg, and right infra-auricular region [Figures 1a-c]. The ulcer on the right leg was well defined and tender with a violaceous rim. The floor of the ulcer was covered with granulation tissue and necrotic slough [Figure 1a]. Musculoskeletal examination demonstrated kyphosis, arachnodactyly, and hyperextensible wrist and thumbs. The arm span was more than the height (177 cm vs. 176 cm) [Figure 2a]. The thumb sign and the wrist sign were positive [Figures 2b and c]. Except for a pansystolic murmur in the mitral area, the examination of systems was within normal limits.
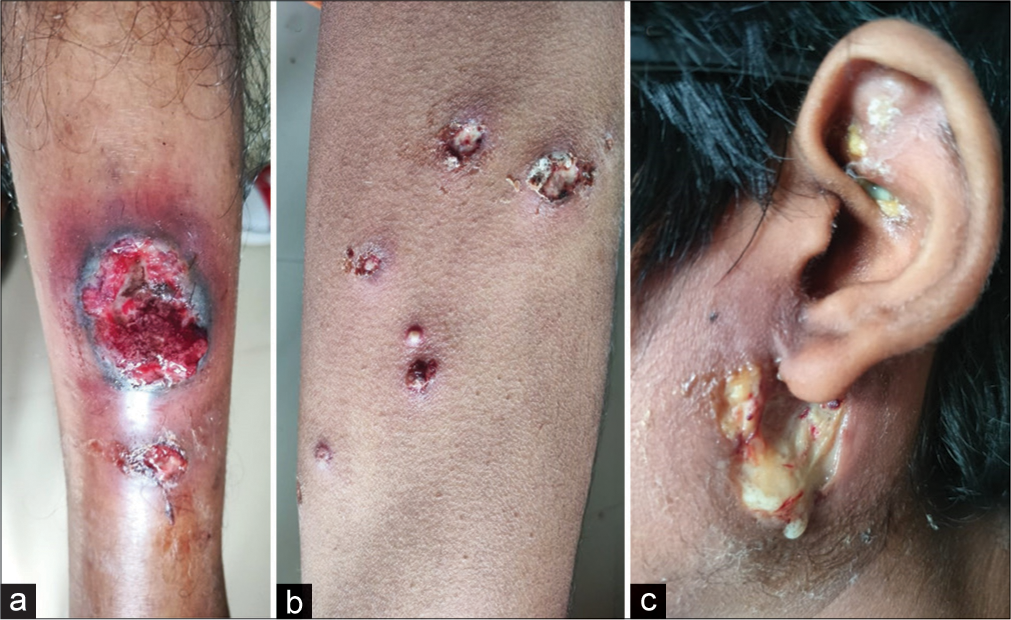
- (a): Well-defined ulcer with a violaceous border on the lower leg; (b): Multiple ulcers on thighs; (c): Infra-auricular ulcer.
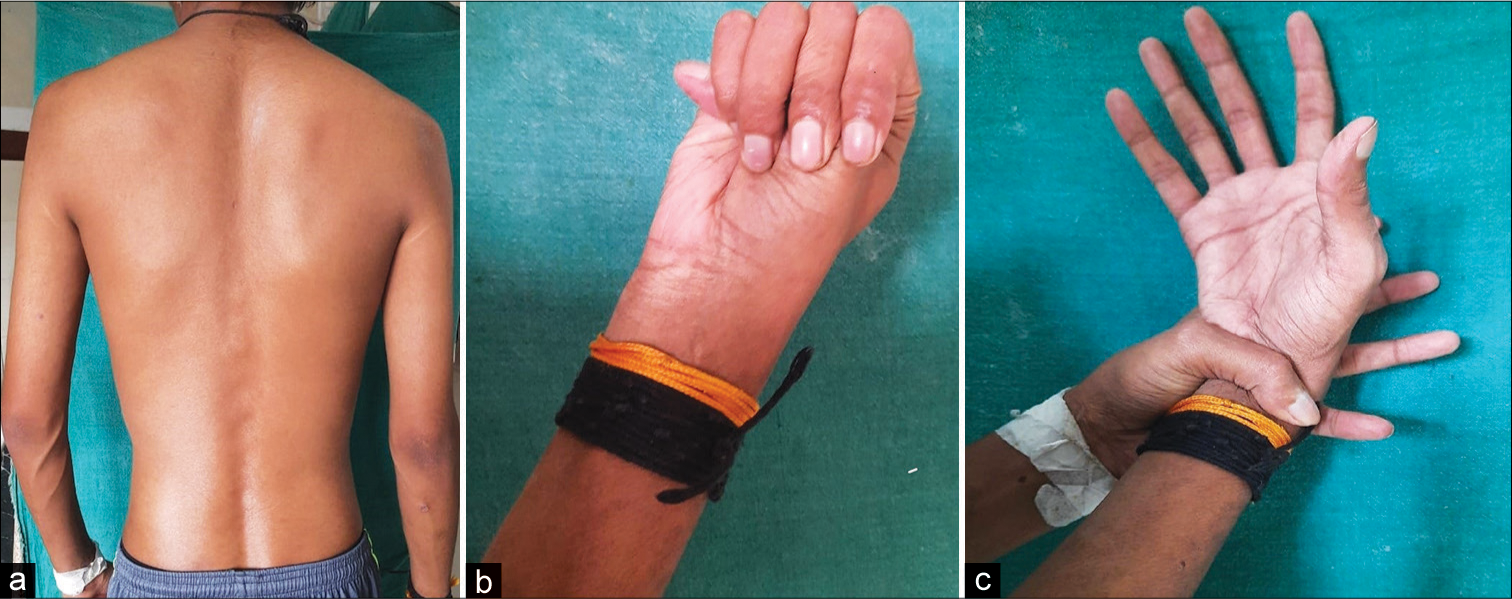
- (a): Kyphosis of Marfan syndrome; (b): Thumb sign; (c): Wrist sign.
Complete hemogram and liver and renal function tests were normal. Serological tests for syphilis and viral markers for human immunodeficiency virus and hepatitis B and C infections were negative. Stool occult blood analysis was negative. Pus culture from the ulcers showed mixed bacterial growth.
Echocardiogram demonstrated mitral valve prolapse and dilated aortic arch. Computed tomography (CT) of brain and CT aortogram were normal. CT abdomen showed malrotated kidneys and segmental mucosal thickening as skip lesions in the colon and rectum. Endoscopy showed chronic colitis with multiple punched out ulcers in the sigmoid colon and fistula in the rectum [Figure 3]. A colonic biopsy revealed non-caseating granulomas suggestive of Crohn’s disease. Ophthalmology examination showed myopia of >5 Diopters. Skin biopsy from the edge of the ulcer showed infiltrates of neutrophils and lymphocytes in the dermis and subcutaneous tissue with no evidence of vasculitis [Figure 4]. Direct immunofluorescence study was negative. These findings were consistent with the diagnosis of pyoderma gangrenosum.
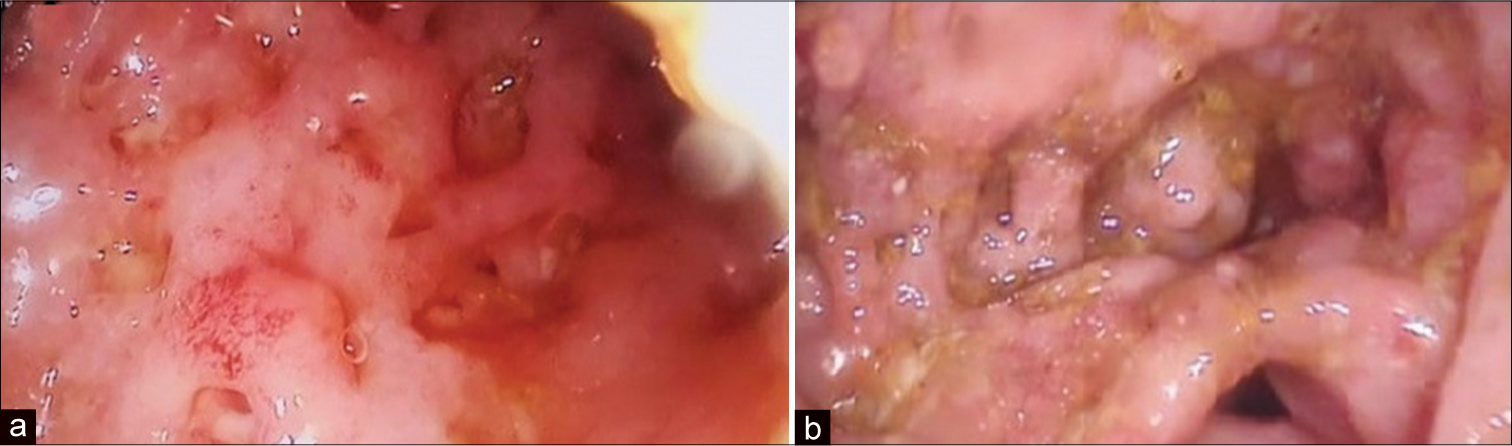
- (a): Colonoscopy showing segmental mucosal thickening of sigmoid colon; (b): colonoscopy showing ulcers and fistula in rectum.
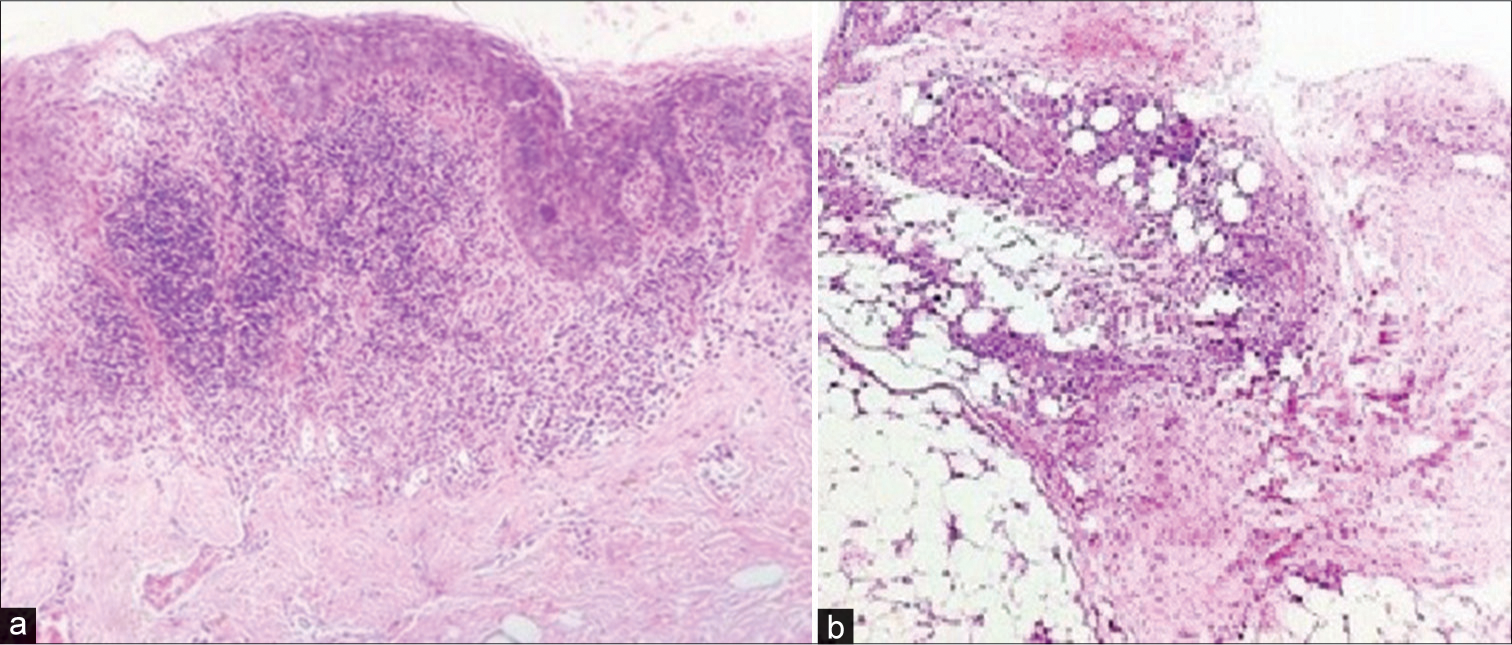
- (a): Skin biopsy from leg ulcer showing neutrophilic infiltration in the dermis (H and E, ×100); (b): Same specimen showing inflammatory infiltrate in the subcutaneous tissue (H and E, ×100).
The patient was started on intravenous (IV) dexamethasone (4 mg twice a day), ciprofloxacin (200 mg IV twice a day for 7 days), mesalamine (800 mg/day per orally), and hydroxychloroquine (200 mg twice a day/orally), to which the patient showed prompt response. Parenteral corticosteroid was changed to oral prednisolone, which we plan to taper gradually in consultation with the gastroenterologist. Patient is continued on mesalamine and hydroxychloroquine.
DISCUSSION
Our patient presented with tall stature, arm span more than height, kyphosis, arachnodactyly, positive thumb and wrist signs, mitral valve prolapse, dilated aortic arch, and myopia, which satisfied the revised Ghent criteria for diagnosis of Marfan syndrome.[4] The patient presented with painful ulcers with characteristic peripheral violaceous margins. A detailed evaluation ruled out other probable causes. Histopathology was suggestive of pyoderma gangrenosum. Endoscopy, CT scan, and colonic biopsy were in favor of Crohn’s disease. The cutaneous ulcers responded to treatment with systemic steroids [Figure 5] and immunomodulators (mesalamine and hydroxychloroquine), which also supported our final diagnosis of pyoderma gangrenosum (coexisting with Marfan syndrome and Crohn’s disease).

- (a): Leg ulcer of pyoderma gangrenosum showing resolution after treatment with systemic corticosteroids and immunomodulators; (b): infra-auricular ulcer in the same patient showing resolution after treatment.
Stria distensae, subcutaneous atrophy, and elastosis perforans serpiginosa are the cutaneous manifestations described in Marfan syndrome.[4] There are reports of hypertrophic and hyperpigmented scars at unusual sites in Marfan syndrome and of Marfan syndrome coexisting with Ehler-Danlos syndrome[5,6] Marfanoid features have been described in multiple endocrine neoplasia.[7] Aortic dissection is the dreaded complication in Marfan syndrome, which contributes to mortality.[2] Beta-blockers, losartan, and angiotensin converting enzyme inhibitors are found useful to prevent cardiovascular complications in Marfan syndrome.[8] Some patients may require surgery.[8]
CONCLUSION
Association between pyoderma gangrenosum and inflammatory bowel disease is well reported in the literature. However, we did not come across any previous report of coexistence of pyoderma gangrenosum, Crohn’s disease, and Marfan syndrome.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Pradeep Nair is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Pyoderma gangrenosum-a guide to diagnosis and management. Clin Med (Lond). 2019;19:224-8.
- [CrossRef] [PubMed] [Google Scholar]
- FBN1 mutations largely contribute to sporadic non-syndromic aortic dissection. Hum Mol Genet. 2017;26:4814-22.
- [CrossRef] [PubMed] [Google Scholar]
- The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010;47:476-85.
- [CrossRef] [PubMed] [Google Scholar]
- A case-control study of cutaneous signs in adult patients with Marfan Disease: Diagnostic value of straie. J Am Acad Dermatol. 2011;64:290-5.
- [CrossRef] [PubMed] [Google Scholar]
- Distinct defects in collagen microarchitecture underlie vessel wall failure in advanced abdominal aneurysms and aneurysms in Marfan syndrome. Proc Natl Acad Sci. 2010;107:862-65.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple endocrine neoplasia type 2B: Frequency of physical stigmata--results of the GPOH-MET registry. Pediatr Blood Cancer. 2020;67:e28056.
- [CrossRef] [PubMed] [Google Scholar]
- Losartan in combination with propranolol slows the aortic root dilatation in neonatal Marfan syndrome. Pediatr Neonatol. 2018;59:211-13.
- [CrossRef] [PubMed] [Google Scholar]







