Translate this page into:
Solitary angiokeratoma closely mimicking nodular melanoma
*Corresponding author: Vinayak Viplav, Department of Dermatology, Katihar Medical College, Katihar, Bihar, India. vinayakviplav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Viplav V, Suman S, Hussain S. Solitary angiokeratoma closely mimicking nodular melanoma. J Skin Sex Transm Dis 2024;6:90-2. doi: 10.25259/JSSTD_48_2023
Dear Editor,
Angiokeratomas are small benign vascular lesions, presenting clinically as red, blue, or purple papules. Solitary angiokeratoma (SA), angiokeratoma of Mibelli, angiokeratoma of Fordyce, angiokeratoma corporis diffusum, and angiokeratoma circumscriptum are the different clinical types.[1] SA, due to its close clinical similarity with nodular melanoma (NM) requires careful evaluation for accurate diagnosis.
Our patient was a 25-year-old woman, who presented with a slowly growing, asymptomatic nodule on the right thigh of 1 year duration. The onset was spontaneous and the lesion gradually increased in size. The lesion did not bleed to the touch. There was no history of any associated weight loss. No other family members were similarly affected.
Examination revealed a black, smooth surfaced nodule of size 0.5 × 0.2 cm over the right thigh, with an adjacent macule of size 1 × 0.5 cm in shades of brown and black [Figure 1]. The nodule was firm in consistency with no evidence of bleeding following touch. No regional lymphadenopathy was noted. There was no organomegaly on systemic examination.

- A deep black smooth-surfaced nodule of size 0.5 × 0.2 cm over the right thigh, with an adjacent pigmented macule demonstrating shades of brown and black of size 1 × 0.5 cm. The inset shows a close-up of the lesion.
Based on the above morphology, we considered the differential diagnoses of NM, atypical melanocyte nevus (AMN), and pigmented spindle cell nevus of Reed. We did an excision biopsy of the nodule with a margin, which included a portion of the adjacent pigmented macule. Histopathology revealed a slightly atrophic epidermis with elongated rete ridges, partially enclosing dilated papillary vessels resembling large cavernous channels [Figure 2]. Dermis showed sparse, lymphocytic interstitial, and perivascular infiltrate. With these findings, we made a final diagnosis of angiokeratoma. The patient was counseled regarding the benign nature of the lesion. On follow-up after 2 weeks, a portion of the lesion that was not excised, resolved spontaneously.
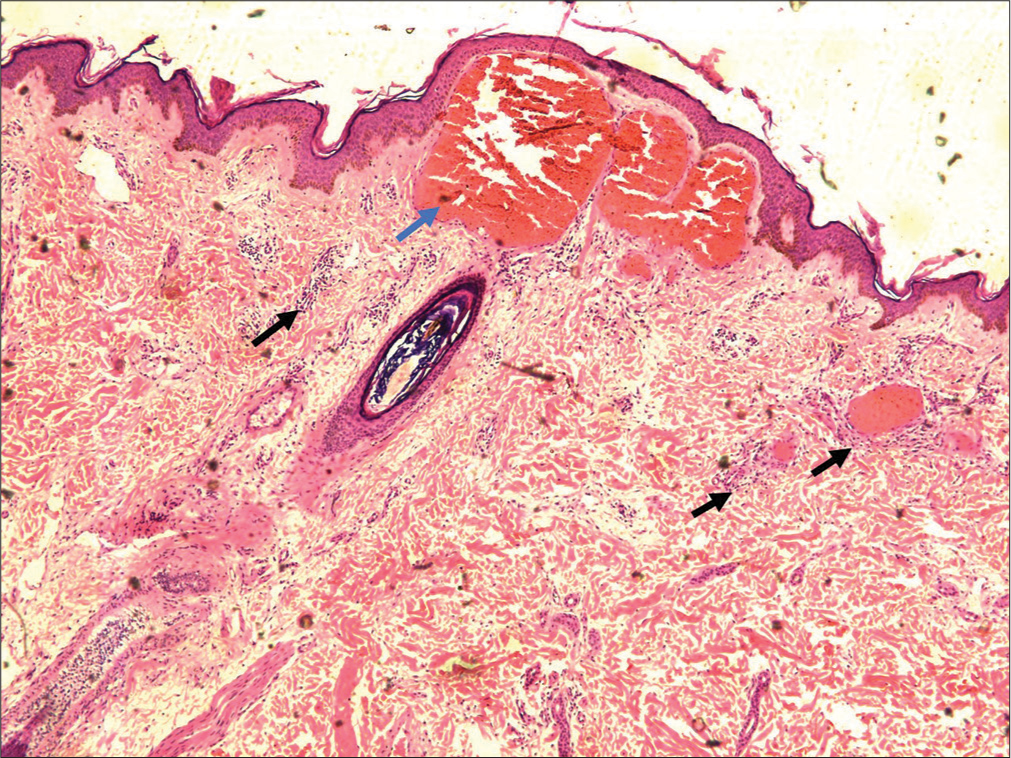
- Histopathology demonstrating a slightly atrophic epidermis with elongated rete ridges partially enclosing dilated papillary vessels resembling large cavernous channels (blue arrow), and sparse perivascular lymphocytic infiltrates (black arrows) (H&E, ×10).
Although innocuous in nature, SA assumes significance due to its close clinical similarity with NM and AMN.
A previous study on angiokeratomas reported that 15% of patients received a clinical diagnosis of malignant melanoma. Moreover, an accurate clinical diagnosis was possible in only 3% of cases. Even on histopathology, an incorrect diagnosis of hemangioma was made in 33%.[2-5] The correct diagnosis was made when the entire section was studied, following complete excision of the lesion.
Atypical presentations of targetoid hemosiderotic hemangioma (THH) could also closely mimic SA. Conventionally, THH demonstrates an immediate zone of pallor, with an outer ring of ecchymosis. However, early lesions of THH may overlap phenotypically with SA and histopathology is needed to differentiate between the two.[6,7] Ectatic vascular channels lined by plump endothelial cells showing intraluminal papillary projections in the upper dermis favor a diagnosis of THH, which is not demonstrated in angiokeratomas. Further, immunohistochemistry with CD34 and D2-40 (lymphatic markers) may be of value that is positive only in THH.[6,7]
Dark lacunae are the most frequent dermoscopic findings in SA and denote the most valuable criterion for the diagnosis of this vascular tumor. This feature is not seen in NM, and in this way, a precise diagnosis can be established. Other dermoscopic features in SA include a whitish veil, peripheral erythema, red lacunae, and hemorrhagic crusts. In NM, on the other hand, a blue-white veil, irregular blotches, irregular brown dots, and globules, and a variegated color pattern scored from tan, dark brown, red, blue, gray, and black constitute the major findings.
In general, histopathology is sufficient to distinguish between SA and NM. However, in cases of diagnostic dilemma immunohistochemistry using melanocytic markers such as S-100 protein, SOX-10, MART-1, HMB-45, and MiTF can be utilized for confirmation.
Our case was treated with excision. Other treatment options include curettage and cautery, cryotherapy, and ablative laser treatment.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Angiokeratoma. A clinicopathological study. Arch Dermatol. 1967;95:166-75.
- [CrossRef] [PubMed] [Google Scholar]
- Angiokeratoma presenting as a melanoma: A case report. J Am Podiatr Med Assoc. 2013;103:241-2.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombotic angiokeratoma circumscriptum simulating melanoma. Arch Dermatol. 1981;117:138-9.
- [CrossRef] [PubMed] [Google Scholar]
- Solitary angiokeratoma of the vulva mimicking malignant melanoma. Cutis. 2018;101:E6-7.
- [Google Scholar]
- Hobnail hemangiomas (targetoid hemosiderotic hemangiomas) are true lymphangiomas. J Cutan Pathol. 2004;31:362-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hobnail hemangioma: A pseudomalignant vascular lesion with a reappraisal of targetoid hemosiderotic hemangioma. Am J Surg Pathol. 1999;23:97-105.
- [CrossRef] [PubMed] [Google Scholar]





