Translate this page into:
Subcutaneous mammary swelling: An atypical presentation of dirofilariasis
*Corresponding author: Pranjal Marlecha, Department of Dermatology, Father Muller Medical College, Mangaluru, Karnataka, India. pranjalm01@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Marlecha P, Martis J, Saldanha E, Suresh HB. Subcutaneous mammary swelling: An atypical presentation of dirofilariasis. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_1_2025
Abstract
Human dirofilariasis is a rare zoonotic infection caused by Dirofilaria species, primarily Dirofilaria repens and Dirofilaria immitis. These parasites predominantly infect canines, with humans serving as accidental hosts. Transmission occurs through mosquito vectors such as Culex, Aedes, and Anopheles. Human infections typically present as subcutaneous nodules or pulmonary lesions, with breast involvement being exceedingly rare. A 41-year-old woman presented with a 7-month history of a painful, enlarging swelling in the upper outer quadrant of her right breast. Physical examination revealed a tender, mobile, erythematous mass measuring 1 cm × 1 cm without axillary lymphadenopathy. Ultrasonography showed a subcutaneous hypoechoic lesion containing coiled, worm-like echogenic structures suggestive of a parasitic infestation. Surgical excision yielded a 14.5 cm long worm, identified as Dirofilaria species. The patient was treated with oral antibiotics and diethylcarbamazine, with no recurrence noted on follow-up. Human dirofilariasis is an emerging zoonosis, with increasing reports worldwide, including in non-endemic regions. Breast involvement is particularly uncommon, often mimicking benign or malignant tumors, leading to diagnostic challenges. Definitive diagnosis is typically achieved through histopathological examination of the excised worm. Surgical removal of the lesion is the treatment of choice, with antiparasitic therapy considered in certain cases. Preventive measures, including mosquito control and public awareness, are essential to reduce the risk of transmission. Clinicians should maintain a high index of suspicion for dirofilariasis in patients presenting with subcutaneous nodules, even in atypical locations like the breast, to ensure prompt diagnosis and appropriate management.
Keywords
Dirofilariasis
Human
Subcutaneous
INTRODUCTION
Dirofilaria, especially Dirofilaria repens and Dirofilaria immitis, is the primary causes of the rare zoonotic infection known as human dirofilariasis.[1,2] Although these parasites primarily infect dogs and cats, there are very few known cases in humans.[3,4] The most common presentation is ocular dirofilariasis, and molecular identification has been done in a few instances; one such report was published as recently as 2018.[5]
Dogs are the primary natural reservoirs for the Dirofilaria species, which mostly afflict them. D. immitis causes cardiac dirofilariasis in animals, but D. repens usually causes subcutaneous infections. Understanding the disease’s epidemiology and management requires knowing which species are involved for better outcomes.[3]
CASE REPORT
In this report, we describe the case of a 41-year-old woman with a subcutaneous mass located at an unusual site. A 41-year-old female patient presented with a painful, gradually enlarging swelling on her right breast, which had developed over the course of 7 months. The initial symptoms included itching and discomfort, but the patient did not experience fever or other systemic symptoms. There was no history of travel in the past year, and she had no medical comorbidities. She also reported no exposure to mosquito bites or breeding sites around her residence and had no pets. In addition, she had not recently visited any water bodies.
Upon examination, a palpable 1 cm × 1 cm nodule was observed in the lower outer quadrant of the right breast. The mass had regular borders, was slightly mobile, tender, and of soft-to-firm consistency, with no signs of axillary lymphadenopathy. The overlying skin was erythematous and warm [Figure 1]. Ultrasound imaging revealed a hypoechoic, oval lesion measuring 16 × 6 mm at the 7 o’clock position of the right breast, along with hyperechoic linear coiled structures, which suggested an inflammatory response likely due to parasitic infection, specifically dirofilariasis [Figure 2]. Surgical removal of the nodule was performed, and a 14.5 cm worm was extracted [Figure 3]. The patient received oral antibiotics and diethylcarbamazine as treatment.

- Solitary erythematous nodule with surrounding erythema.
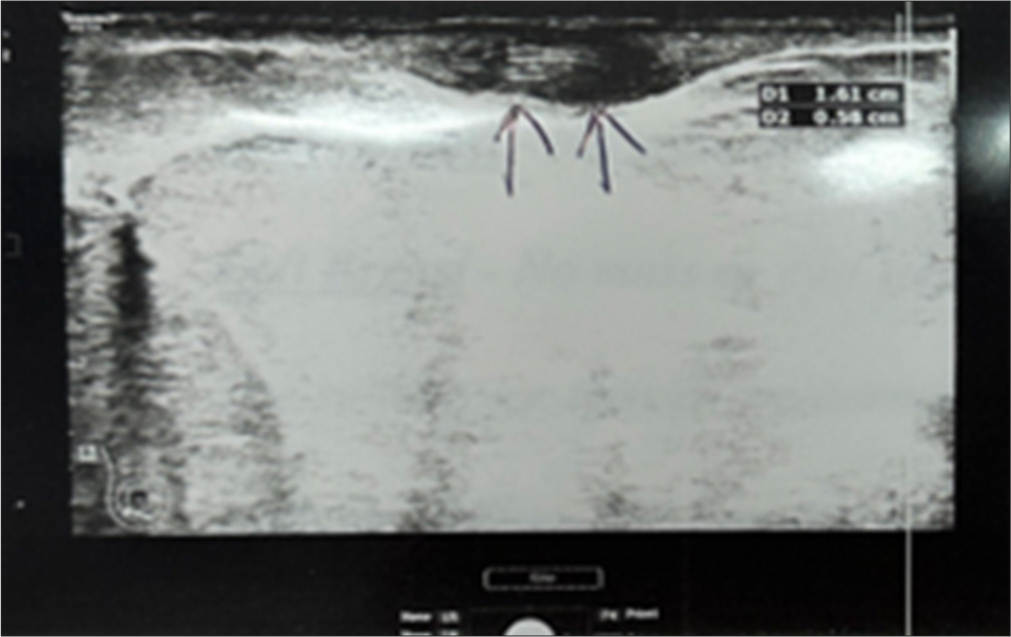
- Ultrasonography image showing a subcutaneous hypoechoic lesion. Internal thin worm-like structures with parallel echogenic borders and anechoic centres can be seen.
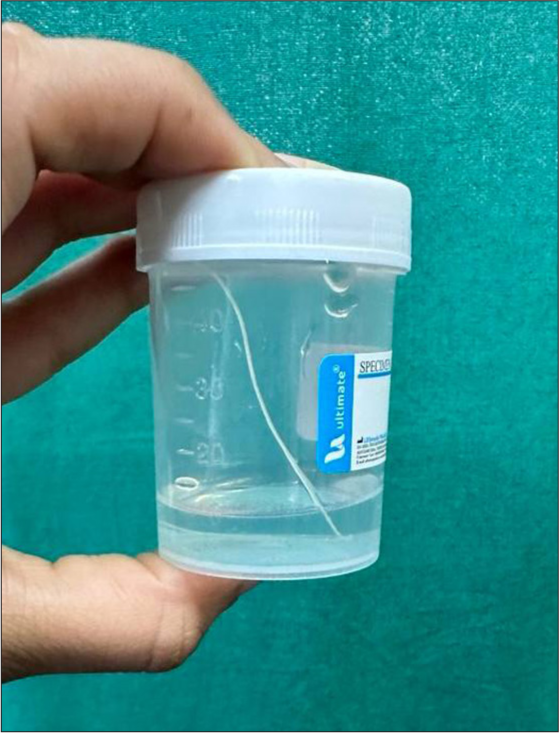
- Coiled worm extracted from the nodule.
DISCUSSION
A zoonotic disease called human dirofilariasis is spread by mosquito bites and is brought on by nematodes. The three most prevalent species of Dirofilaria that infect humans are D. immitis, D. repens, and Dirofilaria tenuis.[6] Dogs and other wild canids are the main hosts of these parasites. The infection is primarily spread by mosquitoes, including Aedes, Anopheles, Culex, and Mansonia.[4]
D. repens more frequently forms subcutaneous or submucosal nodules harboring adult worms, whereas D. immitis usually generates pulmonary lesions, which can manifest as asymptomatic coin lesions.[6] When mosquitoes from infected animals consume the larvae, they develop into third-stage larvae inside the mosquito. Humans are unintentional hosts where the larvae develop into adult worms without causing microfilaremia, yet the larvae are spread when a mosquito bites a human. D. repens is known to harbor a bacterial endosymbiont, Wolbachia, which can influence the host’s immune response during infection.[7]
In coastal areas like Kerala, where the environment and mosquito vectors are favorable for transmission, human dirofilariasis – which is mostly caused by D. repens – is very common. Common infections of the eyes and subcutaneous tissues might be mistaken for cancerous growths, resulting in needless operations. The parasite is spread by mosquito species such as Culex, Aedes, and Anopheles. By changing mosquito behavior and transmission dynamics, climate change is also causing zoonotic filariasis to spread. Breast involvement is uncommon, with the majority of cases affecting the lungs and subcutaneous tissues.[6] Benign and malignant tumors, lipomas, granulomas, abscesses, and infected cysts are among the differential diagnosis for subcutaneous dirofilariasis. Usually, there is no blood eosinophilia or increased immunoglobulin E levels.[5]
Microfilaremia is rare in humans, and no human-to-human transmission cases have been documented. Histopathology confirms the diagnosis, revealing a multilayered cuticle with longitudinal ridges and circumferential musculature interrupted by lateral chords.[7] Magnetic resonance imaging scans may show hyperintense lesions with hypointense curvilinear strands indicative of parasitic cysts, while ultrasound imaging usually shows moving tubular structures with echogenic stripes within a cyst.
The principal treatment for human subcutaneous dirofilariasis is still surgical removal; however, systemic medications such as diethylcarbamazine and ivermectin are frequently employed. Reducing the risk of infection requires preventing mosquito bites, and public health initiatives should concentrate on using ivermectin and doxycycline together to decrease dog infections caused by Dirofilaria.[5]
By changing mosquito breeding habits and disease transmission dynamics, climate change is predicted to raise the prevalence of zoonotic illnesses such as dirofilariasis.[1] The life cycle of mosquitoes can be shortened by rising temperatures, which makes it easier for pathogens to spread. Furthermore, land use and vector habitats may be impacted by climate change, increasing the chance of disease spread to new regions and people.
CONCLUSION
Although rare, human subcutaneous dirofilariasis is being reported more frequently, especially in tropical regions. Early diagnosis is essential to prevent unnecessary invasive procedures. Preventive measures, such as using insect repellent and sleeping under insecticide-treated bed nets, can significantly reduce the risk of mosquito bites and subsequent infection. This case is noteworthy due to its occurrence in a non-endemic region and the unusual site of presentation. A high index of suspicion is required for early diagnosis and appropriate treatment.
Acknowledgment
The authors are grateful to the technical teams involved in laboratory work and radiology.
Ethical approval
The research/study was approved by the Institutional Review Board at Father Muller Institutional Ethics Committee, number ECR/540/Inst/KA/2014/RR-20, dated September 24, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Human and animal dirofilariasis: The emergence of a zoonotic mosaic. Clin Microbiol Rev. 2012;25:507-44.
- [CrossRef] [PubMed] [Google Scholar]
- Dirofilaria repens from the eyelid of a woman in Thailand. Am J Trop Med Hyg. 1983;32:1456-7.
- [CrossRef] [PubMed] [Google Scholar]
- The first case report of subcutaneous dirofilariasis caused by Dirofilaria repens in Thailand. Trop Parasitol. 2021;11:125-7.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous human dirofilariasis. J Parasit Dis. 2011;35:140-3.
- [CrossRef] [PubMed] [Google Scholar]
- Hidden intruder: A rare encounter of dirofilaria masquerading as a breast lump. Cureus. 2023;15:e50535.
- [CrossRef] [Google Scholar]






