Translate this page into:
Acantholytic dyskeratotic acanthoma: A rare clinicopathological entity – A case report and review of literature
*Corresponding author: B. M. Athira, Department of Pathology, Government Medical College, Trivandrum - 695 010, Kerala, India. athirapulari123@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nair NG, Athira BM. Acantholytic dyskeratotic acanthoma: A rare clinicopathological entity – A case report and review of literature. J Skin Sex Transm Dis 2020;2(2):115-8.
Abstract
Acantholytic dyskeratotic acanthoma (ADA) is a rare benign condition characterized by circumscribed epidermal proliferation displaying both acantholysis and dyskeratosis. It is of unknown etiology and pathogenesis. We report a case of ADA of long duration in a 75-year-old female along with a review of literature with special reference to cases reported during the past 10 years.
Keywords
Acantholytic dyskeratotic acanthoma
Verrucous plaques
Distinctive entity
INTRODUCTION
Acantholytic dyskeratotic acanthoma (ADA) is a rare benign condition characterized by circumscribed epidermal proliferation displaying both acantholysis and dyskeratosis. Most cases are clinically diagnosed as basal cell carcinoma, which leads to their excision and histopathologic examination.[1] The incidental finding of focal acantholytic dyskeratosis was first described by Ackerman.[2] Acantholytic acanthoma was originally described as a solitary lesion displaying histologic features of acantholysis without dyskeratosis.[3] Rarely, acantholytic acanthomas without major dyskeratosis or dyskeratotic acanthomas without acantholysis are seen.[1] Herein, we report a case of ADA in a 75-year-old female.
CASE REPORT
A 75-year-old female with no comorbidities presented with two verrucous plaques over the lateral aspect of the right thigh of 60 years duration. She complained of itching over the lesions since 1½ years. The patient noticed mild increase in the size of the lesion for 6 months. She did not have any other skin lesions. No one else in the family had similar lesions. Clinical examination showed two well-defined verrucous plaques with blackish discoloration over the lateral aspect of the right thigh; one measuring 1.3 × 1.5 cm and the other measuring 1 × 1.2 cm. With the differential diagnoses of chromoblastomycosis, squamous cell carcinoma, tuberculosis verrucosa cutis, viral wart, and lupus vulgaris, a biopsy was done from one of the lesions.
Hematoxylin and eosin stained sections showed hyperkeratosis, parakeratosis, crusting, papillomatosis, irregular acanthosis [Figure 1a], and nests of acantholytic cells along with a few dyskeratotic cells within the epidermis. Dermis showed sparse lymphocytes [Figure 1b-d]. With these histopathological features, a diagnosis of ADA was made. The biopsy site healed with secondary intention.
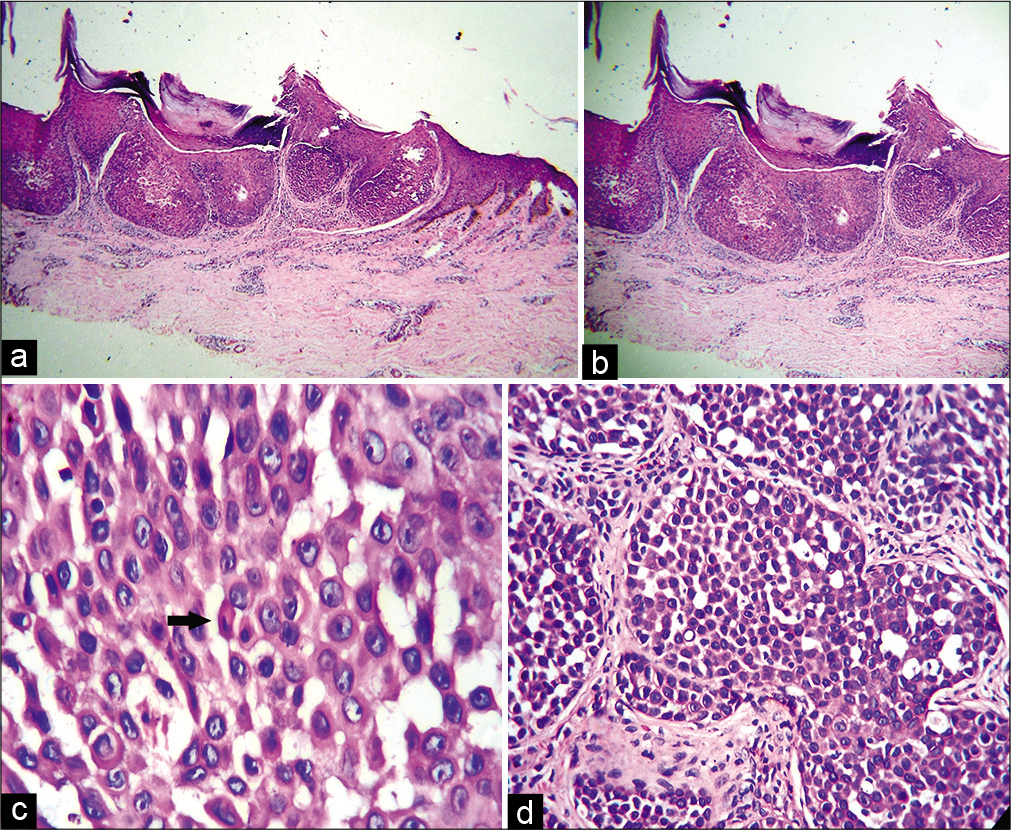
- (a) Exoendophytic epidermal lesion with hyperkeratosis and parakeratosis (H and E, ×40), (b) nests of acantholytic epidermal cells and dermis with sparse lymphocytes (H and E, ×100), (c) large number of acantholytic and dyskeratotic cells (black arrow) (H and E, ×400), (d) Nests of acantholytic cells (H and E, ×400).
DISCUSSION
ADA is a rare variant of epidermal acanthoma, characterized microscopically by acantholysis and dyskeratosis.[3]
Acantholytic dyskeratosis is a histological reaction pattern characterized by suprabasilar clefting with acantholytic and dyskeratotic cells at all levels of the epidermis. It may also be regarded as special subdivision of the vesiculobullous tissue reaction, but the vesiculation is not usually apparent clinically. The primary abnormality involves the tonofilamentdesmosome complex with disordered epidermal maturation. Acantholytic dyskeratosis may be found in a number of different conditions such as Darier’s disease, Grover’s disease, warty dyskeratoma, acantholytic solar keratosis, and vulval and anal acantholytic dyskeratosis. When incidental, it is known as focal acantholytic dyskeratosis.[4]
The term warty dyskeratoma is used to denote solitary lesion displaying a cup-shaped, cystic or nodular architecture with features suggestive of a follicular adnexal lesion.[5] Solitary, nongenital lesions with prominent acantholysis and dyskeratosis without cup-shaped architecture or follicular involvement have been described as a distinct histologic entity: ADA.[3,6]
The term “papular acantholytic dyskeratoma” has been applied to the clinically apparent solitary lesions and “papular acantholytic dyskeratosis” to the exceedingly rare cases, in which multiple lesions have developed on the vulva, perianal area, or penis. A clinically apparent lesion has also been reported on the lip. A case reported as “congenital acantholytic dyskeratotic dermatosis” appears to be a variant of papular acantholytic dyskeratosis. This patient presented with multiple erosive papules and plaques located on the left thigh, left ankle, and right neck since birth. The patient had no family history of Darier’s disease. Genetic studies were not performed. Incidental focal acantholytic dyskeratosis is statistically increased in atypical melanocytic lesions.[4]
Histopathology of the lesion shows, nests of cells with acantholytic dyskeratosis. Hyperkeratosis is less prominent in incidental lesions compared to Darier’s disease. Warty dyskeratomas differ from focal acantholytic dyskeratomas by having more prominent villi, clefting, and corps ronds. Some of the genital and crural cases, mentioned above, have a histological resemblance to Hailey–Hailey disease, with marked acantholysis and little dyskeratosis. They belong to the recently recognized acantholytic subset of acantholytic dyskeratosis, another subset features dyskeratosis alone. In one case of papular acantholytic dyskeratosis of the anogenital region, immunofluorescence showed intercellular IgG and C3 within the epidermis.[4]
Acantholytic subset
Acantholysis, with little or no dyskeratosis, can be seen as an incidental phenomenon or as a solitary tumor of the skin referred to as acantholytic acanthoma. A high proportion of the rare genital, crural, and perineal cases referred to as papular acantholytic dyskeratosis had a histological resemblance to Hailey–Hailey disease, with prominent acantholysis and little or no dyskeratosis. An appropriate designation for these cases would seem to be “acantholytic dermatosis of the genitocrural/perineal region.”[4]
Acantholysis has been observed in a small percentage of seborrheic keratosis. Degenerative changes along with spongiosis result in the acantholysis in seborrheic keratosis and this is more common in the irritated type. Here, the acantholysis is prominent in the upper portion of the epidermal growth and is seen between and around horn cysts. Prominent dyskeratosis is not a feature of seborrheic keratosis.[7] The classical features of seborrheic keratosis such as papillomatosis and irregular acanthosis are not so prominent in ADA. These features help to differentiate acantholytic variant of seborrheic keratosis from ADA.[8,9]
Dyskeratotic subset
It combined dyskeratotic cells throughout the epidermis with a parakeratotic horn containing large rounded cells at all levels.
The term “acquired dyskeratotic acanthosis” has recently been applied to a case in which multiple maculopapules, 3–8 mm in diameter, developed in sun-exposed areas. There were clusters of parakeratotic cells which appeared eosinophilic to “ghostlike.” The epidermis was papillomatous and acanthotic with foci of dyskeratotic keratinocytes.[4]
For literature review, we searched relevant case reports published in English language during the past 10 years.
They included eight cases of cutaneous ADA (including our case) and two subungual cases. The cases are summarized in [Table 1].[1,2,5,10-15]
| Year | Author | Age | Gender | No./size | Location | Clinical presentation | Duration | Medical history |
|---|---|---|---|---|---|---|---|---|
| 2012 | Wan et al.[11] | 33 | Male | 1/4 × 2.8 cm | Lower side of internal malleolus | Yellow plaque with hyperkeratotic surface | 7 years | No other illness |
| 2013 | Park et al.[12] | 42 | Female | Multiple/ 2–3 mm |
Face | Erythematous pruritic papule and tiny vesicles | Several years(b) | Associated with Rosacea |
| 2013 | Pezzolo et al.[10] |
49 | Male | 1/4 × 4 mm | Calf | White-brownish hyperkeratotic papule | 3 years | On immunosuppressive therapy for kidney allograft |
| 2014 | Goldenberg et al.[2] | 72 | Female | 1/10 × 4 mm | Beneath breast | Plaque with erosion in center | 3 months | No other illness |
| 2016 | Kim et al.[13] | 38 | Female | 1/a | Face | Erythematous pruritic plaque | 1 month | Associated with DLE |
| 2018 | Burgler et al.[1] |
60 | Male | Multiple/(a) | Back and lateral chest wall | Papules with slight central umbilication/core | 1 week | Heart transplant patient on immunosuppression |
| 2019 | Kanitakis et al.[14] |
74 | Male | Multiple/(a) | Lower back | Red-brown keratotic papule | Recent onset(b) | Liver transplant patient on immunosuppression |
| 2020 | Present case | 75 | Female | 2/1.3 × 1.5 and 1 × 1.2 cm | Thigh | Verrucous plaques with blackish discoloration | 60 years | No other illness |
| 2017 | Vargas-Laguna et al.[15] |
32 | Male | Single nail/(a) | First toe nail | Pain and serous exudation, round reddish area in nail, subungual hyperkeratosis | 2 years | No other illness |
| 2017 | Ng et al.[5] | 25 | Male | Single nail/(c) | Right thumb nail | Ill-defined paramedian erythronychia and distal onycholysis | 1 year | No other illness |
(a): Not available, (b): Exact duration not given, (c): Not applicable. DLE: Discoid lupus erythematosus
Among the cutaneous cases, the age ranged from 33 to 75 years with a mean age of 55 years. No sex predilection was seen which is in contrast to the study by Ko et al. which showed a female predilection.[3] The size of the lesion varied from 2 mm to 2.8 cm. The most common location was trunk (50%) followed by extremities (25%) and face (25%).The lesions were asymptomatic or pruritic. The lesions presented usually as red-brown, blackish, yellow plaque, or papule. The lesions varied in duration from 1 week to 60 years. Three out of the eight patients had a history of immunosuppression following organ transplant surgery and one of the articles speculated that the immunosuppression necessitated in organ transplant recipients may have prevented the elimination of those cell clones that give rise to this peculiar benign lesion.[1] The immunosuppressive therapy of all the three patients had prednisolone in common. The other drugs used were cyclosporine, tacrolimus, everolimus, and mycophenolate mofetil.[1,14,10]
Both the subungual cases were seen in young adults. They were either asymptomatic or presented with pain and serous exudation. The main clinical features seen were onycholysis, hyperkeratosis, and erythronychia.[5,15]
There is currently neither a World Health Organization statement nor an agreement in explicative dermatopathology whether ADA is a distinct entity. Indeed, in Lever’s histopathology textbook, acantholytic dyskeratosis is described as a phenomena and not a separate entity.[7] In contrast, in the latest edition of Weedon’s Skin Pathology, authors consider cutaneous ADA to be a separate entity, which usually clinically presents with features suggestive of basal cell carcinoma.[4] Many of the articles propose that ADA should be considered as a separate distinct entity.[2]
The etiopathogenesis of this rare entity is still to be established. In different studies, the etiology had been attributed to various factors including hormones, viral infection, immunologic factors, tobacco use, physical stimuli, and sunlight exposure.[12] Surgical excision of the lesion appears to be the definitive treatment.[2]
CONCLUSION
ADA is a rare benign lesion which usually present as plaque or papule of typically <3 cm in size. Subungual cases present as onycholysis and erythronychia. Our case is that of a 75-year-old female with a verrucous plaque on the lateral side of thigh. In our review of literature, we found that ADA occurs over a wide age group and the main histopathological features are intraepidermal nests of acantholytic and dyskeratotic cells along with subtle additional features in the epidermis. We consider it as a clinically and pathologically distinct entity which requires more studies to establish its exact nature and etiopathogenesis.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Nandakumar Gopinathan Nair is on the Editorial Board of the Journal.
References
- Multiple acantholytic dyskeratotic acanthomas in an organ transplant recipient. JAAD Case Rep. 2018;4:695-7.
- [CrossRef] [PubMed] [Google Scholar]
- Acantholytic dyskeratotic acanthoma: Case report and review of the literature. Dermatol Pract Concept. 2014;4:25-30.
- [CrossRef] [Google Scholar]
- Acantholytic dyskeratotic acanthoma: A variant of a benign keratosis. J Cutan Pathol. 2008;35:298-301.
- [CrossRef] [Google Scholar]
- Disorders of epidermal maturation and keratinization In: Patterson JW, ed. Weedon's Skin Pathology (4th ed). London: Churchill Livingstone Elsevier; 2015. p. :302-5.
- [Google Scholar]
- Subungual acantholytic dyskeratotic acanthoma: An unusual cause of longitudinal erythronychia. Pathology. 2018;50:482-4.
- [CrossRef] [PubMed] [Google Scholar]
- Plaque form of warty dyskeratoma-acantholytic dyskeratotic acanthoma. J Cutan Pathol. 2007;34:494-6.
- [CrossRef] [PubMed] [Google Scholar]
- Tumors and cysts of the epidermis In: Elder DE, Elenitsas R, Rosenbach M, Murphy GF, Rubin AI, Xu X, eds. Lever's Histopathology of the Skin (11th ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2015. p. :973.
- [Google Scholar]
- Seborrheic keratosis: Acantholytic variant. J Cutan Pathol. 1978;5:145-9.
- [CrossRef] [Google Scholar]
- Acantholytic dyskeratotic acanthoma in an immunosuppressed patient: A case report with review of literature. Clin Dermatol. 2013;1:149-52.
- [Google Scholar]
- Incidental focal acantholytic dyskeratosis in the setting of rosacea. Ann Dermatol. 2013;25:518-20.
- [CrossRef] [PubMed] [Google Scholar]
- Incidental focal acantholytic dyskeratosis in a patient with discoid lupus erythematosus: A possible role for SPCA1 in the pathogenesis of the disease. Ann Dermatol. 2017;29:655-7.
- [CrossRef] [Google Scholar]
- Multiple acantholytic dyskeratotic acanthomas in a liver-transplant recipient. Dermatol Online J. 2019;25:6.
- [Google Scholar]
- An unusual location of subungual warty dyskeratoma: A case report and review of the literature. Case Rep Dermatol Med. 2017;2017:3613109.
- [CrossRef] [Google Scholar]






