Translate this page into:
Clinicopathological analysis of basal cell carcinoma – A retrospective study
*Corresponding author: Mohamed Nazeer, Department of Dermatology Venereology and Leprosy, Amala Institute of Medical Sciences, Amala Nagar, Thrissur, Kerala, India. drnazeerkv@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: George RM, Nazeer M, Criton S, Abraham UM, Francis A. Clinicopathological analysis of basal cell carcinoma – A retrospective study. J Skin Sex Transm Dis 2021;3(1):51-5.
Abstract
Objectives:
The objective of the study was to analyze the demographic profile, histopathological features, risk factors, and recurrence rates in patients with basal cell carcinoma.
Materials and Methods:
A retrospective study was conducted from 2012 to October 2018 in 29 patients with histopathologically confirmed basal cell carcinoma. All the patients had undergone either excision or cryotherapy as per the institution protocol. Information on the history of the disease, occupation, history of sun exposure and clinical and histopathological features were collected and analyzed.
Results:
A female preponderance was found (n = 18, 62.1%), majority of the patients were unemployed (44.8%), 19 patients (65.5%) gave a history of sun exposure, and the nose was the most common site of disease. Ten females (34.5%) did not have any excessive exposure to the sun, but gave a history of exposure to heat and fumes in the kitchen. Six patients (20.7%) had a preexisting nevus at the same site and superficial spreading type was the most common histopathological type (n = 24, 82.8%). Excision gave the best result. Four patients (13.8%) had recurrence of the disease.
Limitations:
Small sample size was the major limitation. The risk factors and occupation could not be analyzed objectively.
Conclusion:
This is a pioneer study from Kerala. A female preponderance (62.1%) was observed. The role of heat, fumes, type of oven, and use of reheated oil in cooking as risk factors for the development of BCC needs analysis in future studies. Superficial spreading type was the most common pattern observed in histopathology slides (82.8%). Excision gives near-complete clearance and a good cosmetic result with less risk of recurrence.
Keywords
Basal cell carcinoma
Non-melanoma skin cancer
Superficial spreading
Cutaneous
Neoplasm
INTRODUCTION
Basal cell carcinoma is the most common cutaneous malignancy, and along with squamous cell carcinoma, is grouped together as non-melanoma skin cancer (NMSC), to differentiate them from melanomas. About 74% of NMSCs are basal cell carcinomas.[1] There is a 10% rise in the incidence of basal cell carcinoma per year worldwide.[2] This neoplasm is common in fair Caucasians and is rare in dark skin phenotypes. NMSCs comprise 1%–2% of cutaneous neoplasms in India, compared to one-third in Caucasians.[3] This can be explained by the protection offered by melanin pigment against ultraviolet radiation, which is carcinogenic.
UVB is the most important risk factor as 80% of lesions are seen on the head-and-neck area.[4] Risk of disease increases with intermittent periods of sun exposure.[5] Other risk factors include ionizing radiation, arsenic exposure, inherited syndromes, and immunosuppression.[6]
Clinical types of BCC include nodular, superficial spreading, pigmented, morpheaform, and fibroepithelioma of Pinkus. Majority of the lesions appear on the head and neck, usually above the line joining the tragus of the ear and the angle of the mouth. Histopathological variants are nodular, miconodular, superficial, pigmented, infiltrative, morphemic, metatypical, and fibroepithelioma. Less common types are keratotic, adenoid, clear cell, granular type, and BCC with sebaceous and eccrine differentiation. Basosquamous cell carcinoma is a rare subtype of BCC with areas of both basaloid and squamoid differentiation. Some consider basosquamous cell carcinoma and metatypical BCC as synonyms, whereas others are of the view that they are separate entities.[7]
BCC is a slow-growing tumor that invades local structures and usually does not metastasize. Poor prognostic factors are size >2 cm, depth of invasion, mid-facial area, ill-defined margins, long-standing disease, and immunosuppression. Perineural and vascular invasion increases the risk of metastasis.[8]
Although the incidence of BCC in India is low, the number of cases is significant due to our large population. The existing Indian literature is limited with lack of clinical studies. Hence, this study was undertaken to determine the epidemiology, risk factors, type of disease, histopathological type, and treatment response.
MATERIALS AND METHODS
Sample size was calculated as follows:
p = proportion of wide local excision (80.20)
q = 1-p
d = relative precision (20% p)
α = significance level 5% (3.84)
n = 24
The study population comprised 29 patients with histopathologically confirmed BCC who attended the dermatology outpatient department of our tertiary care center from January 2012 to October 2018. Previous medical records of all patients were collected and data analyzed retrospectively. Histopathology slides were reviewed by two separate pathologists. Data were tabulated with regard to patient demographics and clinical findings. Patients were then personally contacted to know about the status of their disease. Institutional ethics committee approved the study. The study participants gave informed verbal consent for the follow-up information.
Statistical analysis
Data were analyzed using SPSS Software 23.0. Descriptive statistical methods such as percentage, mean, and standard deviation were used to describe the background variables of the study population.
RESULTS
A total of 29 histopathologically confirmed cases of BCC were enrolled in the study from January 2012 to October 2018. All the patients had the nodular variety as the clinical presentation.
Demographic profile
Majority of the patients (n = 11, 37.9%) were in the age group between 41 and 60 years with a mean of 64.2 and standard deviation 12.9. There were 11 males (37.9%) and 18 females (62.1%).
Occupation
Majority of the patients were unemployed (13, 44.8%). Three patients (10.3%) were manual laborers, four (13.8%) were professionals, and nine patients (31.03%) had office jobs.
Triggering factors
Nineteen (65.5%) patients gave a history of sun exposure. All 29 households used earth ovens and coconut oil for cooking purposes. Ten females (34.5%) had no excessive exposure to the sun and gave a history of exposure to heat and fumes in the kitchen. Six patients (20.7%) had a preexisting nevus at the same site.
Site of the lesion
The sites of the lesions were nose (10 patients, 34.5%), forehead (4 patients, 13.8%), ear (7 patients, 24.1%), cheek (5 patients, 17.2%), eye (1 patient, 3.4%), abdomen (1 patient, 3.4%), and breast (1 patient, 3.4%).
Histopathology
The superficial spreading variant was the most common histopathological type (24, 82.8%) [Table 1 and Figures 1-4].
| Histopathology | Frequency | Percent |
|---|---|---|
| Superficial spreading | 24 | 82.8 |
| Nodulocystic | 1 | 3.4 |
| Metatypical | 1 | 3.4 |
| Pigmented | 1 | 3.4 |
| Basal cell carcinoma with squamoid differentiation | 2 | 6.9 |
| Total | 29 | 100.0 |

- (a) Skin biopsy specimen from the lesion of basal cell carcinoma showing superficial spreading type (H and E, ×40). (b) Higher magnification of Figure 1a (H and E, ×100).
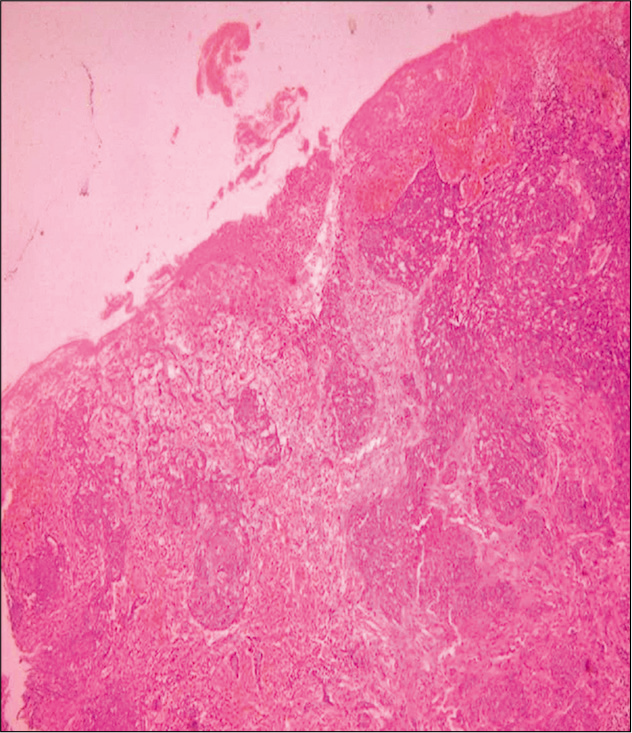
- Skin biopsy specimen from the lesion of basal cell carcinoma showing metatypical type (H and E, ×100).

- Skin biopsy specimen from the lesion of basal cell carcinoma showing nodulocystic variant (H and E, ×100).

- Skin biopsy specimen from the lesion of basal cell carcinoma showing squamoid differentiation (H and E, ×400).
Treatment
Twenty-two patients (75.9%) underwent excision and closure [Figure 5a and b], 5 (17.2%) had excision with skin grafting, and two (6.9%) underwent multiple sittings of cryotherapy [Table 2].

- (a) Basal cell carcinoma in a 70-year-old female; (b) picture of the same patient taken after 6 months following surgical excision of the lesion.
| Treatment done | Frequency | Percentage of total |
|---|---|---|
| Excision and closure | 22 | 75.9 |
| Excision with skin grafting | 5 | 17.2 |
| Cryotherapy | 2 | 6.9 |
| Total | 29 | 100.0 |
Four patients (13.8%) came back with a recurrence at the same site. The nose was the common site that had recurrence. The histopathological diagnoses in recurred cases were superficial spreading (2/4, 50%), metatypical (1, 25%), and BCC with squamoid differentiation (1/4, 25%). Out of the four, two patients had undergone cryotherapy as they did not get fitness for surgery and multiple sittings were required.
The other two who suffered recurrence of BCC had received excision and closure as treatment.
DISCUSSION
Basal cell carcinoma is a common cutaneous malignancy.[1] It is considered as a disease of the fair skinned population, explaining the paucity of studies from developing countries. Jina et al. reported that skin changes were more common in males due to increased sun and chemical exposure.[9] Al-Zou et al. reported an increasing trend of basal cell carcinoma in southern governorates of Yemen.[10] A male preponderance with ulceroproliferative type of disease as the most common variety was found in a study conducted in 21 patients.[9] Kumar et al. noticed an increasing trend of BCC with female preponderance and involvement of nose.[11] Ammasaigoundan et al. also observed a female preponderance. They reported predominance of nodular variety of BCC in their study conducted in 30 patients.[12] Our findings of nodular type being the most common clinical form and nose being the most common site were consistent with the literature.[11-13]
We observed a higher number of females in our study and they did not give any history of excessive sun exposure. This is against the popular thinking that sun exposure is the primary cause for basal cell carcinoma since the pathogenesis commonly involves exposure to ultraviolet light as explained by Leffell and Brash.[14] It can be explained by the fact that females tend to spend a considerable amount of time in the kitchen and less time in the sun. In the kitchen, they are constantly exposed to the heat and fumes generated from cooking. In our study, all the households were in the practice of using coconut oil for cooking purposes. Srivastava et al. have studied the carcinogenic risk associated with consumption of heated coconut oil.[15] Repeated heating of vegetable oil generates polycyclic aromatic hydrocarbons, which are known to have carcinogenic potential. All the households in our study were also using earth ovens for their cooking needs rather than gas stoves. These ovens are lit using wood. This practice also increases the risk of exposure to polycyclic aromatic hydrocarbons, whose primary source is from burning carbon containing compounds such as wood and fuel. James et al., in a study among rural women in South India, reported that exposure to biomass fuel (during cooking) had significant association with dermatological symptoms like skin irritation.[16] Since the female patients gave a history of exposure to heat and fumes with majority denying sun exposure, the role of the former as a risk factor for BCC needs to be analyzed in prospective studies with large sample size.
The superficial spreading type was the common histopathological variant observed. This type accounts for 15%–26% of the total cases of BCC in literature.[17] Jadotte et al. reported a case of superficial spreading pattern of BCC that was treated with Mohs micrographic surgery. The patient also received topical imiquimod considering the risk of recurrence.[18] Two of the 24 patients (8.3%) who showed the superficial spreading pattern of histopathology in the current study, later developed recurrence of the disease. The other two patients who suffered a recurrence had histopathology features of metatypical variant and BCC with squamoid differentiation respectively. According to the literature, a more aggressive clinical course is observed in metatypical variant.[7]
We found excision to be the best modality of treatment. This was in agreement with other studies.[19-22] Cryotherapy required multiple sittings which proved cumbersome for patients. Moreover, both the patients (100%) who received cryotherapy reported back with recurrence at the same site as against the 7.4% (2/27) who developed recurrence following excision.
Limitations
The small sample size was a limitation. Large multicentric studies are needed to better quantify the risk factors. The risk factor analysis is incomplete as the various factors could not be objectively assessed, for example, the duration of sun exposure and the time at which the patients were exposed to the sun. A proper definition for considerable sun exposure needs to be made. The occupation also could not be assessed objectively because even those who claimed to have office jobs had field work as part of their routine duties.
CONCLUSION
This is the first study of its kind from Kerala. In agreement with other studies, a female preponderance was noted. The authors propose that the role of heat and fumes generated during cooking and the types of oil and oven used (for cooking) in causing BCC needs analysis in future studies since these factors increase the exposure time to compounds with carcinogenic potential like polycyclic aromatic hydrocarbons. The superficial spreading type was the most common histopathological type. We found excision as an effective therapeutic option in basal cell caracinoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Basal cell carcinoma: A 6-year clinicopathological study from the Sub-Himalayan region of North India. Chrismed J Health Res. 2019;6:254-8.
- [CrossRef] [Google Scholar]
- Basal cell carcinoma: 10 years of experience. J Skin Cancer. 2011;2011:476362.
- [CrossRef] [PubMed] [Google Scholar]
- Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-60.
- [CrossRef] [PubMed] [Google Scholar]
- Basal cell carcinoma: What's new under the sun. Photochem Photobiol. 2010;86:481-91.
- [CrossRef] [PubMed] [Google Scholar]
- Does intermittent sun exposure cause basal cell carcinoma? A case-control study in Western Australia. Int J Cancer. 1995;60:489-94.
- [CrossRef] [PubMed] [Google Scholar]
- Environmental risk factors predisposing to the development of basal cell carcinoma. Dermatol Surg. 2004;30:248-52.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic concordance rates in the subtyping of basal cell carcinoma by different dermatopathologists. J Cutan Pathol. 2014;41:9-13.
- [CrossRef] [PubMed] [Google Scholar]
- Nonmelanoma skin cancers: An Indian perspective. Indian J Dermatopathol Diagn Dermatol. 2014;1:55-62.
- [CrossRef] [Google Scholar]
- Clinicopathological profile, diagnosis and treatment of skin cancers at a tertiary care center: A retrospective study. Int Surg J. 2017;4:2549-55.
- [CrossRef] [Google Scholar]
- Skin cancer: ClinicoPathological study of 204 patients in Southern Governorates of Yemen. Asian Pac J Cancer Prev. 2016;17:3195-9.
- [Google Scholar]
- A study of basal cell carcinoma in South Asians for risk factor and clinicopathological characterization: A hospital based study. J Skin Cancer. 2014;2014:173582.
- [CrossRef] [PubMed] [Google Scholar]
- Basal cell carcinoma-a prospective clinico epidemiological and pathological study. Int J Res Med Sci. 2017;5:2712-7.
- [CrossRef] [Google Scholar]
- Epidemiological and excision margin status of basal cell carcinoma--three years armed forces institute of pathology experience in Pakistan. Asian Pac J Cancer Prev. 2010;11:1421-3.
- [Google Scholar]
- Genotoxic and carcinogenic risks associated with the dietary consumption of repeatedly heated coconut oil. Br J Nutr. 2010;104:1343-52.
- [CrossRef] [PubMed] [Google Scholar]
- Household cooking fuel use and its health effects among rural women in Southern India-A cross-sectional study. PLoS ONE. 2020;15:e0231757.
- [CrossRef] [PubMed] [Google Scholar]
- Superficial basal cell carcinoma on the face is a diagnostic challenge. Indian J Dermatol. 2016;61:236.
- [CrossRef] [PubMed] [Google Scholar]
- CASE REPORT superficial spreading basal cell carcinoma of the face: A surgical challenge. Eplasty. 2010;10:e46.
- [Google Scholar]
- Nonsurgical options for the treatment of basal cell carcinoma. Dermatol Pract Concept. 2019;9:75-81.
- [CrossRef] [PubMed] [Google Scholar]
- Nonsurgical treatment options for basal cell carcinoma. J Skin Cancer. 2011;2011:571734.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of basal cell carcinoma: European consensus-based interdisciplinary guidelines. Eur J Cancer. 2019;118:10-34.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges and new horizons in the management of advanced basal cell carcinoma: A UK perspective. Br J Cancer. 2014;111:1476-81.
- [CrossRef] [PubMed] [Google Scholar]






