Translate this page into:
Artificial intelligence in dermatology
*Corresponding author: Amitha Abraham, Department of Dermatology Venereology and Leprosy, Government TD Medical College Alappuzha, Alappuzha, Kerala, India. amithaabraham23@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abraham A, Sobhanakumari K, Mohan A. Artificial intelligence in dermatology. J Skin Sex Transm Dis 2021;3(1):99-102.
Abstract
Artificial intelligence (AI) refers to the ability of a machine to communicate, reason, and operate independently. There is a need to understand this technology’s progress for future medical care. AI has many applications in the field of medicine, but its use in dermatology is comparatively new. Applications that commonly analyse and classify images and tools like risk assessment calculators are available. Even though many applications exist, the important implementation barriers inclue difficulty in standardization, interpretability, and acceptance by patient and doctor.
Keywords
Artificial intelligence
Machine learning
Melanoma
Tele-dermatology
INTRODUCTION
Artificial intelligence (AI) can be defined as the branch of computer science dealing with the simulation of intelligent human behavior in computers. It is done by creating algorithms that can solve problems and are programmed for all the specificities of the problem. The term AI is credited to John McCarthy. Dermatology has taken the leading position for the implementation of AI in the medical field because of its large clinical, dermoscopical, and dermatopathological image database.
PRINCIPLES AND TYPES
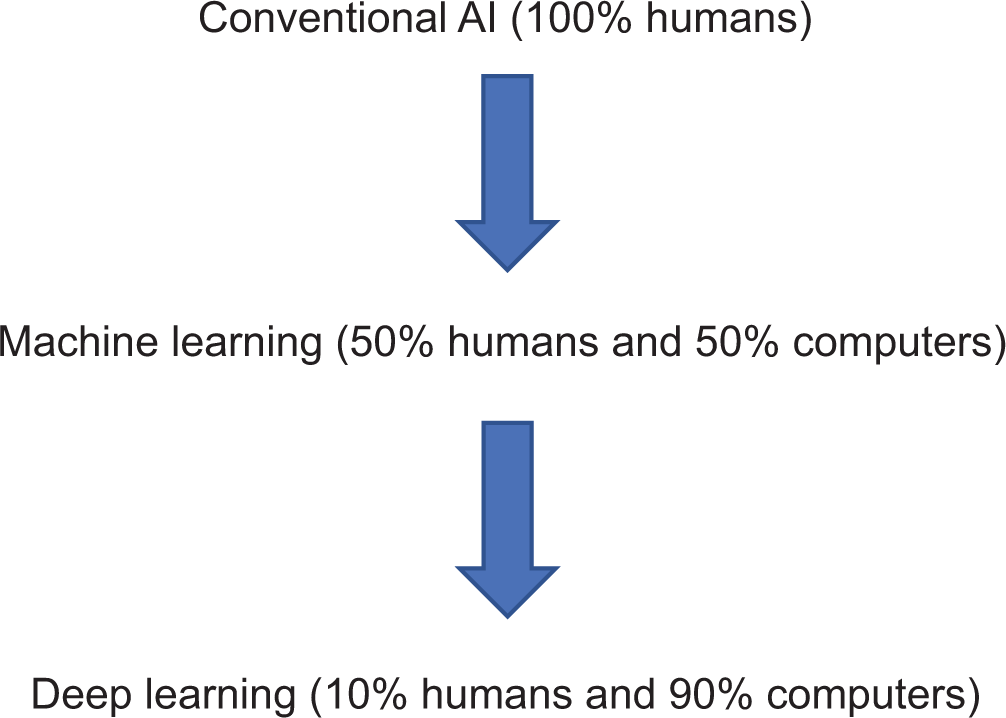
AI is continuously evolving from
Machine learning
Machine learning process involves
Input – in the form of data
Algorithms consume the training data
Output – a machine learning model is the output generated.
MACHINE LEARNING PROCESS
Most commonly used learning processes are:
Supervised learning We train the machine to match a set of inputs (e.g., images) to their correct output (diagnosis).
Unsupervised learning After training the machine by supervised learning, the machine is made to analyze new/novel patterns from the data and to give output.
TYPES OF AI
Narrow AI – Capable of handling one particular task. For example: Identification of consolidation in lungs.
General AI – Capable of handling a wide range of tasks. For example: Identification of consolidation/pleural effusion/cardiomegaly.
Two learning methods of AI are:
Shallow learning Based on predefined engineered features as per expert knowledge.
Deep learning Based on deep features processed by convolutional neural network (CNN). Imitates the working of the human brain in processing the data. Deep learning algorithm does not require explicit feature definition by human experts.
CNN
It is the most prevalent deep learning architecture. Computational models comprise series of layers and successively match inputs to desired end points.
AI IN MEDICINE
The main applications of AI are in radiology, pathology, and dermatology. AI ranges from simple automated blood pressure monitors to robot-assisted surgery. In 2018, FDA approved unguided AI tool (IDx-DR) for the diagnosis of diabetic retinopathy, based on retina images. Furthermore, there are FDA approved mobile applications that help to treat opioid addiction and aid with contraception (2018), further enhancing the digital human partnership.
AI IN DERMATOLOGY
Dermatology is a field with a growing interplay of digitalization, tele-health, and informatics. Hence, AI can be used for dermatological applications as well.
Distinguishing between benign and malignant lesions
The main principle behind this application is that dermoscopic or non-dermoscopic images of lesions can be broken down into individual pixels for analysis. These applications are typically validated by comparing their ability to correctly diagnose lesions with the ability of a certified dermatologist. Jafari et al. described 60 features based on images to classify them.[1] In 2017, Stanford university published a study on deep learning of skin tumors. They trained CNN, using more than 1 lakh images of around 2000 different diseases and tested its performance against that of 21 board-certified dermatologists on biopsy-proven clinical images. It was found that machine had a competence, comparable to that of board-certified dermatologists in identifying and classifying skin cancers.[2]
For example: Benign nevi versus malignant melanoma, nonmelanoma skin cancers versus benign and premalignant lesions.
Although most of the research on AI is based on photorecognition algorithms, numerical values can also be applied.
For example: To predict the complexity of Mohs micrographic surgery based on variables assessed at the initial evaluation visit such as tumor size and patient age. These can be used to triage patients and prioritize Mohs referrals. Hence, risk factor assessment is possible with AI. These applications were described by Tan et al.[3]
In recent years, smartphone applications are available and easily accessible for diagnosis of melanoma. Actually, they offer an instant risk assessment of likelihood of malignancy so that the patients can seek medical advice at an early stage. Disadvantage is the possibility of missing melanomas or giving a false sense of security to the user. Sensitivities and specificities for this applications range from 7% to 73% and 37% to 94%, respectively.[4]
Furthermore, Al can assist in histopathological diagnosis of malignancies. CNN is trained with a data set of histopathological and corresponding clinical images to generate diagnosis. Studies by Hekler et al. showed promising results on the role of CNN in the definite diagnosis of melanoma.[5]
Ulcer assessment
AI is mainly employed for diabetic and pressure ulcer assessment at present. Applications are capable of measuring precise wound boundaries and are able to differentiate between the types of tissue involved. They can classify granulation, slough, and necrotic tissue. Mukerjee et al. described an AI application for classification of wound tissues.[6] Risk prediction tools also exist, for example, to predict the tendency for the development of pressure ulcers.
Psoriasis and other inflammatory skin diseases
In psoriasis, AI mainly focuses on improving psoriasis classification methods using image recognition. Emam et al. demonstrated systems’ ability to predict response to biologic therapy in psoriasis patients, using parameters gauged at initial visit, so as to optimize treatment.[7]
Other applications
Other dermatological conditions where AI has found a role are acne, lichen planus, pityriasis lichenoides, dermatomyositis, and seborrheic dermatitis.
For example: smartphone application that grades and classifies acne lesions.
Atopic dermatitis
There are artificial neural networks for differentiating atopic dermatitis from unaffected skin using information derived directly from images. This was designed by De Guzman et al.[8]
Onychomycosis
Diagnostic accuracy for onychomycosis is increased using deep learning AI with a reference set comprising all possible images. Han et al. used more than 49,000 images in their data set.[9]
Predicting skin sensitization substances
There are applications capable of analyzing the physiochemical properties of substances. They can determine whether the substance could be a sensitizer or not. Studies were conducted by Zang et al. They described an application, capable of determining the melting point of a substance and deciding whether it could be a sensitizer or not.[10]
Dermatopathology
Applications that can automate histopathology image processing and classification (mainly for skin malignancies) have been described.
Tele-dermatology
It is one of the fast growing fields of dermatology, especially in areas where access to a dermatologist is difficult. AI can be integrated into smartphone applications to photograph skin lesions, collect relevant clinical information, and generate referral when needed. At present, tele-dermatology is an integral part of clinical practice due to the ongoing COVID pandemic.
Augmenting face-to-face assessment
Rather than functioning alone, AI and humans (dermatologist) working together can achieve better results in diagnosing and managing skin conditions.
AI as an educational tool
AI is as excellent educational resource for training dermatologists, researchers, students, and skin cancer specialists. After going through visually similar images, medical experts are able to gain deeper insights into their cases which help them to make a more accurate diagnosis.
AI in the field of dermoscopy
This technology uses AI algorithms and content-based image retrieval to provide medical professionals dermoscopic images that are visually similar to their submitted cases.
Limitations
Generalizability
Most of the studies available are from Western world and from developed nations. The findings may not be applicable to the rest of the world. Each population should have their own data based on the local prevalence of the disease and should develop individual algorithm. Although difficult in developing countries at present, it will definitely become a part of clinical practice in future.
At present, image data of different skin diseases are insufficient, and the quality of images is not uniform.[11] This leads to lack of standardization.
Image quality
Technical variation, difference in image acquisition, and image quality can all affect interpretation.
Data requirement
One large barrier is the pre-requisite of large quantity of data of appropriate quality to process AI algorithms.
Interpretability
AI is flexible, it forms algorithms, re-evaluates, and constantly brings changes without human input by means of neural networks. Therefore at times, the logic behind the decision-making may not be interpretable.
Acceptance by patients
A proper history, followed by examination, eliciting specific signs complemented by additional investigations or biopsy, is a standard way of diagnosis in dermatology. This holistic approach cannot be fully replaced by any methods including AI.
Liability/ethical issues
If there is an adverse outcome from AI, who should be made liable, is another question.
Multidisciplinary approach
AI researchers come from different fields of science such as computer science and biomedical, and medical science. Hence, it is a difficult task to coordinate the group.
CONCLUSION
While AI is helpful in diagnosing disease into broad categories, dermatological expertise and clinical correlation will still be needed for accurate diagnosis and for decision-making, at present. Currently, most of the data are based on Western studies; hence, studies from this part of the world are essential. AI is a rapidly advancing field, hence, a basic knowledge about the fundamental principles, potential uses, and limitations becomes all the more important.
Declaration of patient consent
Not required as there are no patients in this article.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Sobhanakumari K is on the editorial board of the Journal.
References
- Extraction of skin lesions from nondermoscopic images for surgical excision of melanoma. Int J Comput Assist Radiol Surg. 2017;12:1021-30.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115-8.
- [CrossRef] [PubMed] [Google Scholar]
- A practical decision-tree model to predict complexity of reconstructive surgery after periocular basal cell carcinoma excision. J Eur Acad Dermatol Venereol. 2017;31:717-23.
- [CrossRef] [PubMed] [Google Scholar]
- Smartphone applications for triaging adults with skin lesions that are suspicious for melanoma. Cochrane Database Syst Rev. 2018;12:CDO13192.
- [Google Scholar]
- Pathologist-level classification of histopathological melanoma images with deep neural networks. Eur J Cancer. 2019;115:79-83.
- [CrossRef] [PubMed] [Google Scholar]
- Automated tissue classification framework for reproducible chronic wound assessment. Biomed Res Int. 2014;2014:851582.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting the long term outcomes of biologics in psoriasis patients using machine learning. Br J Dermatol. 2020;182:1305-7.
- [CrossRef] [PubMed] [Google Scholar]
- Design and evaluation of a multi-model, multilevel artificial neural network for eczema skin lesion detection. 2015 3rd International Conference on Artificial Intelligence, Modelling and Simulation (AIMS), Kota Kinabalu, Malaysia 2015:42-7. Available from: https://www.ieeexplore.ieee.org/document/7604549 [Last accessed on 2019 Dec 18]
- [CrossRef] [Google Scholar]
- Deep neural networks show an equivalent and often superior performance to dermatologists in onychomycosis diagnosis: Automatic construction of onychomycosis datasets by region-based convolutional deep neural network. PLoS One. 2018;13:e0191493.
- [CrossRef] [PubMed] [Google Scholar]
- Prediction of skin sensitization potency using machine learning approaches. J Appl Toxicol. 2017;37:792-805.
- [CrossRef] [PubMed] [Google Scholar]
- Use of artificial intelligence in dermatology. Indian J Dermatol. 2020;65:352-7.
- [CrossRef] [Google Scholar]






