Translate this page into:
Neutrophilic dermatosis of dorsal hands: A unilateral presentation
*Corresponding author: Anju Joseph, Department of Dermatology, Venereology and Leprosy, Pushpagiri Institute of Medical Sciences and Research Centre, Thiruvalla, Kerala, India. anjujoseph5991@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Joseph A, Pappen TT, Kunjukunju BP, Mathew L, Jayaprakash A. Neutrophilic dermatosis of dorsal hands: A unilateral presentation. J Skin Sex Transm Dis 2024:6:41-3. doi: 10.25259/JSSTD_57_2023
Abstract
A rare localized version of Sweet syndrome known as neutrophilic dermatosis of dorsal hands is characterized by bluish or hemorrhagic papules, bullae, and nodules on the dorsal hands. Cases have been associated with myeloproliferative disorders, malignancy, inflammatory bowel disease, and rheumatoid arthritis. We are reporting a case of a 39-year-old male presented with sudden onset hyperpigmented raised lesions studded with fluid-filled vesicles on the left dorsal hands. Histology confirmed the clinical diagnosis of neutrophilic dermatosis of dorsal hands. Unilateral presentation of neutrophilic dermatosis of dorsal hands is rarely encountered in day-to-day practice. Hence, we are reporting this case.
Keywords
Neutrophilic dermatosis of dorsal hands
Neutrophils
Sweet syndrome
INTRODUCTION
Dr. Robert Douglas Sweet originally described Sweet syndrome in 1964, which was characterized by an acute onset of fever, leukocytosis, and tender erythematous plaques infiltrated by mature neutrophils. A localized pustular variant of Sweet syndrome where the lesions are restricted to the dorsal hands was initially described in 1995 as “Pustular vasculitis of dorsal hands” by Strutton et al. and later described by Galaria et al. in 2000 as “Neutrophilic dermatosis of dorsal hands (NDDH).”[1,2] Patients with neutrophilic dermatosis of dorsal hands develop erythematous to violaceous plaque, and they may become bullous or ulcerative. The characteristic histologic presentation is a diffuse and nodular neutrophilic infiltrate without any evidence of vasculitis. Occasionally, the dermal infiltrate can extend into the subcutis.[3] The lesions are similar to Sweet syndrome in morphology and show rapid resolution on treatment with systemic corticosteroids and dapsone.[4]
CASE REPORT
A 39-year-old male presented with multiple vesicles and bullae surrounded by a violaceous border on the dorsum of the left hand for 1-month duration [Figure 1]. It began as multiple reddish-raised lesions on the dorsal aspect. There was a history of fever two days before the onset of lesions, which lasted for one week. He had associated pain and itching sensation. There is no history of trauma, insect bite, or any drug intake.

- Vesicles and bullae surrounded by a violaceous border on the left dorsal hand.
On examination, the patient was febrile. Dermatological examination showed 4–5 vesicles and bullae surrounded by a violaceous border on the left dorsal hand. There was associated crusting and a central erosion. It was tender on palpation with no induration.
With the details mentioned above, we considered differential diagnosis of localized neutrophilic dermatosis, insect bite reaction, and secondary pyoderma.
Blood hemogram showed a total leukocyte count of 11.4 × 109/L with 61% neutrophils, 30% lymphocytes, and raised erythrocyte sedimentation rate and C-reactive protein. Pus culture and sensitivity were done to rule out secondary pyoderma, which was sterile. Tzanck test showed the presence of neutrophils. To confirm the diagnosis, a punch biopsy was taken which showed dermal edema along with diffuse infiltrate composed of predominantly neutrophils with lymphocytes and eosinophils [Figures 2 and 3].
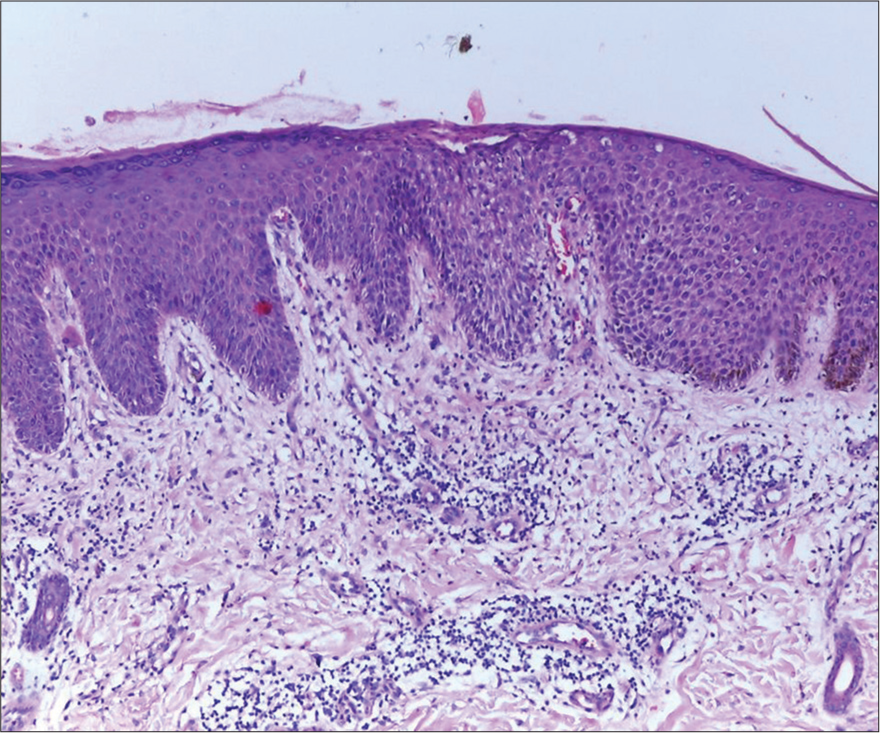
- Dermal edema along with diffuse infiltrate composed of predominantly neutrophils with lymphocytes and eosinophils (H&E ×100).
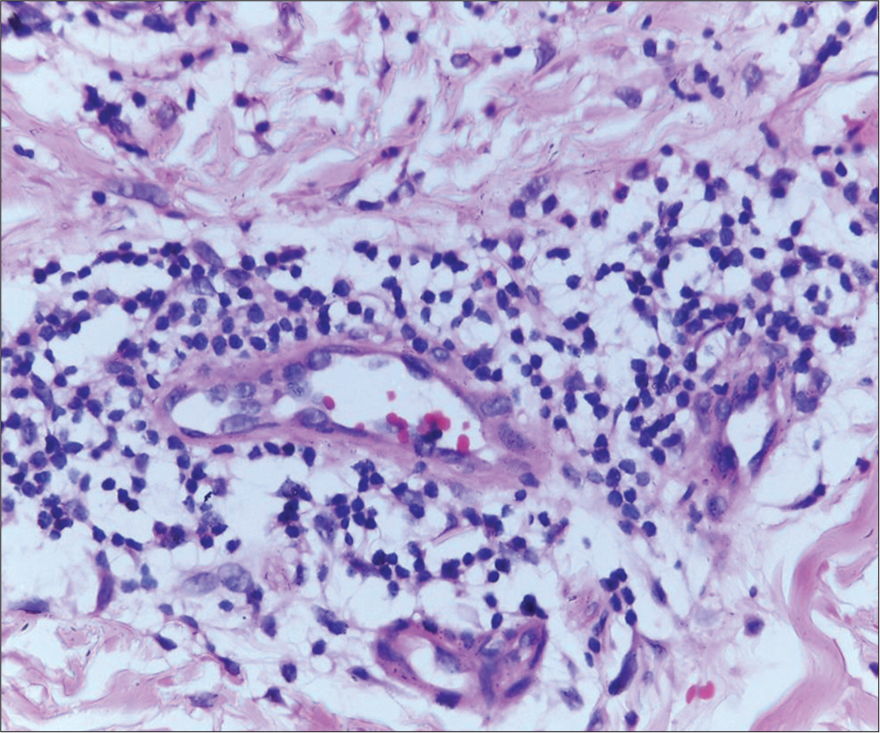
- Perivascular infiltrate composed predominantly (H&E ×100) of neutrophils with few lymphocytes and eosinophils.
Thyroid function test and rheumatoid factor were found to be within normal limits. There malignancy or inflammatory bowel disease and patient did not consent for further investigations.
All the features confirmed the diagnosis of neutrophilic dermatosis of dorsal hands, which is a recently described entity. Azithromycin 500 mg OD was given for a 7-day duration but did not show any response. It was changed to dapsone 100 mg once daily, and it showed marked improvement in 2 weeks. The treatment was continued for two months, following which there was complete resolution of lesions.
DISCUSSION
Strutton et al., in 1995, described violaceous papulonodules on the radial aspect of dorsal hands in six women. The histopathological picture was that of neutrophilic dermatosis and leukocytoclastic vasculitis. He proposed the term “pustular vasculitis of hands.”[2] In 2000, Galaria et al. introduced the term neutrophilic dermatosis of hands after clinical and histopathological examination of three similar patients with lesions limited to the hands. These lesions lacked true vasculitis.[3]
The pathogenesis of this condition remains to be elucidated. It could result from a hypersensitivity reaction to either bacterial, viral, or tumor antigens, causing modifications in cell signaling and cytokine production, which further increase the production and migration of neutrophils toward the skin and tissues.[5] Elevation in the levels of granulocyte colony-stimulating factor has also been reported.[1]
Bluish or hemorrhagic papules, bullae, and nodules on the dorsal hands characterize neutrophilic dermatosis of dorsal hands. Clinical differentiation from pyoderma gangrenosum, especially the bullous variant, and pustular vasculitis is difficult.[1]
The clinicopathological characteristics of Sweet syndrome are sufficiently distinctive, which led to the development of diagnostic criteria by Su and Liu in 1986, later modified by von den Driesch in 1994 to include the abnormal laboratory values.[6,7]
The diagnostic criteria include two major criteria: (1) Sudden onset eruption of tender, painful plaques or nodules and (2) neutrophilic infiltrate in the dermis without vasculitis. Both must be present to establish a diagnosis of Sweet syndrome. For diagnostic confirmation of Sweet syndrome, there should be at least two minor clinical features present; these include (1) fever >38°C, (2) illness preceded by an upper respiratory or gastrointestinal infection or associated with an underlying typical inflammatory disorder, malignancy, or pregnancy, (3) elevated white cell count with neutrophil predominance and elevated inflammatory markers, and (4) positive response to corticosteroids.[7]
NDDH is reported in association with various malignant and non malignant conditions. These include acute myelocytic leukemia, lymphoma, cancers of the lung, breast, and colon, influenza vaccine, glomerulonephritis, inflammatory bowel disease, IgA gammopathy, seropositive arthritis, sarcoidosis, infections like hepatitis C, urinary tract infection, streptococcal tonsillitis, and exposure to chemicals like thalidomide chemotherapy, fertilizers.
Histopathology holds the key to the diagnosis of the disease. There is a dense infiltrate of neutrophils in the dermis with papillary edema occasionally producing subepidermal vesiculation or bullae.[4] Few cases show the presence of vasculitis, which is thought to be an epiphenomenon rather than a primary immune complex-mediated disease, i.e., vasculitis occurring due to vessel wall transmigration of inflammatory cells.[8] The absence of vasculitis helps to differentiate Sweet syndrome from other neutrophilic dermatoses, such as leukocytoclastic vasculitis and erythema elevatum diutinum.[9]
NDDH responds promptly to treatment with prednisolone or dapsone.[1]
Our patient had a unilateral presentation of multiple papules and plaques superimposed with vesicles on the dorsal hands. The diagnostic criteria proposed by von den Driesch were satisfied. No specific cause for the development of lesions was identified. There was a rapid response to treatment with dapsone along with antihistamines and topical antibiotics.
CONCLUSION
Unilateral presentation of NDDH is rarely reported in the literature. This case shows that prompt clinical recognition and management of the condition can result in rapid cure.
Ethical approval
Institutional review board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Neutrophilic dermatosis In: Griffiths CE, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook’s textbook of dermatology (9th ed). Oxford: Wiley Blackwell; 2016. p. :49.10.
- [Google Scholar]
- Pustular vasculitis of the hands. J Am Acad Dermatol. 1995;32:192-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic dermatosis of the dorsal hands: Pustular vasculitis revisited. J Am Acad Dermatol. 2000;43:870-4.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema and urticaria In: Andrews' diseases of the skin: Clinical dermatology (13th ed). Netherlands: Elsevier; 2020. p. :147.
- [Google Scholar]
- An unusual association between sweet's syndrome and metastatic papillary follicular thyroid carcinoma. Ann Dermatol. 2013;25:84-7.
- [CrossRef] [PubMed] [Google Scholar]
- Sweet's syndrome (acute febrile neutrophilic dermatosis) J Am Acad Dermatol. 1994;31:535-56.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic dermatosis of the dorsal hands in a patient with polycythemia vera. Acta Dermatovenerol Alp Pannonica Adriat. 2013;22:53-4.
- [Google Scholar]
- Vascular inflammation (Vasculitis) in sweet syndrome: A clinicopathologic study of 28 biopsy specimens from 21 patients. Arch Dermatol. 2002;138:345-9.
- [CrossRef] [PubMed] [Google Scholar]






