Translate this page into:
Ross syndrome: A rare and complex disorder of thermoregulation
*Corresponding author: Vinitha Panicker, Department of Dermatology and Venereology, Amrita Institute of Medical Sciences, Amrita Viswapeedam, Kochi, Kerala, India. vinithaanil28@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Panicker V, Pradeep L, Jagadeesan S, Mathew D. Ross syndrome: A rare and complex disorder of thermoregulation. J Skin Sex Transm Dis. 2024;6:207-9. doi: 10.25259/JSSTD_31_2024
Dear Editor,
Ross syndrome is an uncommon dysautonomia defined by a triad of segmental anhidrosis or hypohidrosis, areflexia, and tonic pupil.[1] However, compensatory segmental hyperhidrosis and heat intolerance constitute the most distressing complaints among patients. Since its original description in 1958, approximately 50 cases have been reported in the literature. We report the case of a 51-year-old female patient with features of Ross syndrome.
A 51-year-old female with no known comorbidities presented with a history of excessive sweating and hyperpigmentation on the right side of the face, right half of the trunk, right upper limb, and right lower limb of 4 years duration [Figure 1a and b]. The patient also noticed facial asymmetry [Figure 2] and relative sweating of the contralateral side. Dermatological examination revealed patchy areas of increased and decreased sweating over the face, trunk, and limbs. There was no history of application of any topical medications on the affected area. There was no history of any syncope or trauma to the spine. A general examination revealed no abnormalities. Blood pressure recordings performed in both supine and prone positions were within the normal range. A detailed neurological examination revealed diminished sensations, sluggish deep tendon reflexes, and autonomic dysfunction in the right half of the body. The above findings were confirmed with nerve conduction studies. Nerve conduction velocity showed mild distal sensory polyneuropathy of axonal type. Routine blood investigations were within normal limits. Anti-nuclear antibody was negative. Skin biopsy taken from the right side of the abdomen showed homogenous dermal hyalinization with scattered eccrine glands [Figure 3]. The ophthalmologic evaluation showed normal pupils bilaterally. This constellation of features pointed toward Ross syndrome, probably in evolution. The patient was started on oxybutynin (2.5 mg twice daily) for three weeks and was advised periodic ophthalmic evaluation and other therapeutic options, such as botulinum toxin injection that was offered; however, she deferred injections and did not follow up.
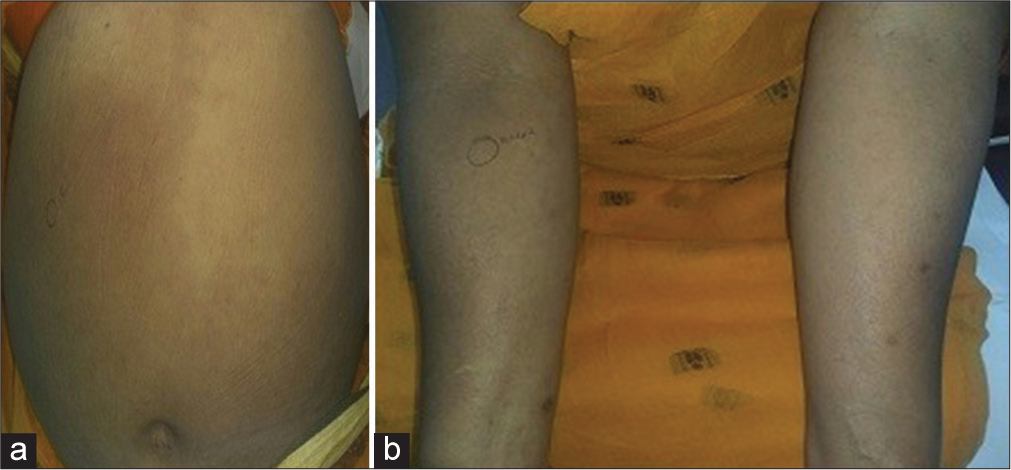
- (a): Hypohidrosis over the left side with hyperpigmentation and hyperhidrosis over the right side of the abdomen; (b): Diffuse hyperpigmentation over the right forearms.

- Asymmetry of the face.
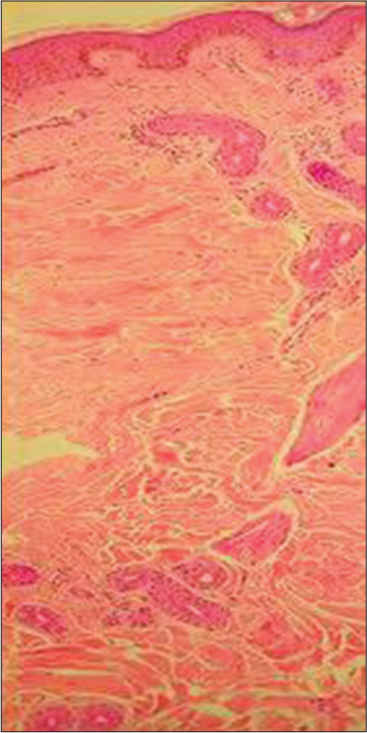
- Homogenous dermal hyalinization with scattered eccrine glands over the affected side (Hematoxylin and eosin stain, ×40).
Ross syndrome is a rare disorder of sweating characterized by widespread hypohidrosis accompanied by patchy compensatory hyperhidrosis and often associated with areflexia and tonic pupil.[1] No gender predilection has been noticed. The anhidrosis may be localized or widespread. In cases of extensive anhidrosis, the unaffected areas may exhibit increased sweat production as compensatory hyperhidrosis, which can sometimes be severe enough to require treatment. However, this may diminish over time as complete anhidrosis evolves. [2] The exact etiopathogenesis of Ross syndrome remains unknown. The degeneration of parasympathetic neuronal structures, though non-specific, is widely regarded as the most probable cause. Hypohidrosis or anhidrosis is thought to originate from degeneration of postganglionic projections. Impaired regulation of cutaneous blood flow, leading to dilatation of dermal vasculature, has also been observed. Furthermore, damage to the ciliary ganglion leads to the development of a tonic pupil, while changes in deep tendon reflexes are due to injury to the dorsal root ganglion. This condition has a close overlap with other rare syndromes such as Holmes-Adie syndrome (hyporeflexia with tonic pupil) and Harlequin syndrome (segmental hypohidrosis without pupillary abnormalities).[3]
Sweating disturbances are typically the first indication of Ross syndrome, and they are a diagnostic prerequisite. The majority of patients are unaware of their anhidrotic areas and usually present with patchy localized hyperhidrosis. In Ross syndrome, hyperhidrosis is a compensatory mechanism that often affects unilateral regions of the trunk, most frequently between the T5 and T12 dermatomes. A decrease or absence of deep tendon reflexes during a neurological examination is the second most reliable indicator. Given that our patient’s ocular characteristics were lacking at the time of initial presentation, incomplete or partial Ross syndrome may be the cause.[2] Long-term follow-up and evaluation are mandatory to watch for the development of other associated features of dysautonomia as well as ocular features. The darkening over the hyperhidrotic areas was a unique cutaneous characteristic observed in our patient. After a comprehensive review of the literature, it was discovered that there have only been four reports of similar cases of Ross syndrome with pigmentary alterations from India to date.[4]
The treatment choices for this illness are limited. Wearing moist clothing during physical exertion can help avoid hyperthermia and hyperhidrosis, as can iontophoresis and botulinum toxin injections.[3] Recently, topical glycopyrrolate was tested for the treatment of compensatory hyperhidrosis and found to be successful.[5] The first point of consultation varies from patient to patient, depending on the symptomatology and timing of symptom onset. Unfortunately, many cases may go undiagnosed or be misdiagnosed. An accurate diagnosis can assist reduce the patient’s worry and, thereby, enhance their quality of life. The relevance of this case report is from the identification of certain cutaneous lesions that led to the diagnosis of autonomic nerve dysfunction.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Vinitha Panicker and Dr. Soumya Jagadeesan are on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Disorders of the sweat glands In: Rook's textbook of dermatology (9th ed). United States: Wiley; 2016. p. :1-22.
- [CrossRef] [Google Scholar]
- Progressive selective sudomotor denervation: A case with coexisting Adie's syndrome. Neurology. 1958;8:809-17.
- [CrossRef] [Google Scholar]
- Ross syndrome: A case report and review of cases from India. Indian J Dermatol. 2016;61:348.
- [CrossRef] [Google Scholar]
- Use of topical glycopyrrolate in Ross syndrome. J Am Acad Dermatol. 2006;55:S111-2.
- [CrossRef] [Google Scholar]





