Comparison of the sexual behaviors and syndromic diagnosis between rural and urban cases in east-central India: A retrospective hospital-based study
*Corresponding author: Suvesh Singh, MD, DNB, MNAMS, Assistant Profressor, Department of Dermatology, Narayan Medical College, Sasaram, Bihar, India suveshsingh2658@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta R, Singh S. Comparison of the sexual behaviors and syndromic diagnosis between rural and urban cases in east-central India: A retrospective hospital-based study. J Skin Sex Transm Dis. 2024;6:137-43. doi: 10.25259/JSSTD_23_2024
Abstract
Objectives:
Sexually transmitted infections (STIs) are a significant public health challenge in India. Limited healthcare access, socioeconomic inequalities, and gender-based vulnerabilities contribute to the disproportionate burden in rural and urban areas. The aim of this study was to compare the sociodemographic profile, sexual behavior, and the syndromic diagnosis of STIs between rural and urban cases attending an STI clinic.
Materials and Methods:
A cross-sectional retrospective study was conducted at an STI clinic in east-central region of India. All patients, irrespective of age and sex, who visited the clinic from July 2022 to November 2023, were included in the study. Demographic, clinical, and behavioral data were compared between urban and rural cases using appropriate statistical methods.
Results:
Out of 925 patients, rural and urban cases were 70.8% and 29.2%, respectively. Rural cases: 92.2% females, 7.8% male; urban cases: 81.1% females, 18.9% males. The majority were aged 20 -40 years. There were more cases aged below 20 years from urban areas (6.3% vs. 2.7%; P < 0.01). Illiterate cases were more from rural area (P < 0.01); and those educated >10th grade from urban area (P < 0.01). The predominant occupation was homemakers and incomes ranged between Rs 5000 and 10000. In both rural and urban areas, lower abdomen pain was the most common symptom, followed by vaginal discharge. Genital herpes (P < 0.01) and syphilitic genital ulcers to syphilis (P = 0.01) were more common in urban areas compared to rural. Retroviral infection was reported to be similar from both areas.: Mean age of sexual debut was 19.5 years in rural and 20.2 year in cases from urban areas (P < 0.01). Time since last sexual encounter (21.2 vs. 20.3 days, P = 0.01), and cases with multiple partners (4.1% vs. 8.8%; P < 0.01) were different in cases from rural and urban cases. The difference in drug abuse and contact with sex worker were not significantly different between the groups.
Limitations:
Retrospective study design, hospital-based study setting and lack of microbiological confirmation were the limitations of this study.
Conclusion:
There were disparities in the sociodemographic profile, STI patterns, and sexual behavior between rural and urban cases of the east-central zone of India.
Keywords
Sexual transmitted disease
Sexual behavior
Syndromic approach
Urban and rural population
East-central India
INTRODUCTION
Sexually transmitted infections (STIs) are a major public health issue that impacts on health, social, and economic state in many developing and developed countries. The burden of sexual/reproductive tract infections (RTIs) varies according to the regions with more public health issues in resource-poor-setting. In India, STIs/RTIs affects about 6% of the adult population, which roughly estimate around 30–35 million cases/year.[1]
Due to limited health facilities and access in developing countries like India, the syndrome approach to the management of STIs is still the cornerstone. It is already known that there are inequalities between rural and urban populations on various factors such as sociocultural, economical, educational, and physical environment.[2] The rising economic development and urbanization have led to accelerated epidemiological transition in the of STI pattern. In many developing countries, there is still a lack of sex education which has contributed to increased STI cases, unplanned pregnancies and complications. STIs in urban areas may be attributable to a greater proportion of migrant or bridging populations.[3,4]
The purpose of our study was to compare the sociodemographic profiles, the pattern of STIs syndrome, and sexual behavior among the rural and urban cases seeking treatment from a tertiary care center in the east-central zone of India.
MATERIALS AND METHODS
A cross-sectional hospital-based retrospective study was conducted in STIs clinic of a tertiary care center located in an urban area of an east-central India. All patients either staying and living in the rural or urban area presented to the STIs clinic were included, irrespective of age and gender from July 2022 to November 2023.
The details from the STIs clinic record included age, gender education, address, marital status, income, occupation, drug abuse, and clinical complaints. Based on the clinical symptoms, the patients were further classified into different syndromes as per the National AIDS Control Organization. The data also included sexual behavior such as the age of sexual debut number of partners, duration of the marriage, last contact encounter, type of partner (regular/casual/sex worker male/sex worker female), symptoms in a partner if any, partner occupation of the partner and number of similar episodes in the past, history of drug abuse, nature of sexual contact (protected or unprotected), were also recorded. Relevant investigations, such as human immunodeficiency virus, hepatitis B surface antigen, hepatitis C, and rapid plasma regain, were also recorded. All these data were grouped according to the address based on the rural and urban area for further comparison between different parameters.
Statistical analysis
Data analysis
The data were entered in Microsoft Excel, and coding was done for further statistical analysis. Categorical variables were summarized in frequency percentages, and tests of proportion were used. Quantitative variables at baseline were summarized by mean ± standard deviation or median (range). The Shapiro–Wilk and Kolmogorov–Smirnov tests were applied for the quantitative variables to check normality. The Mann–Whitney U-test was used for non-parametric data, while the Student’s t-test was used for parametric data to test the significance. Similarly, for categorical data, the Chi-square test was used to compare the values in the two groups using IBM Statistical Package for the Social Sciences software version 20. To compare the significanct difference in the proportion between the two groups, the MedCalc Software Ltd. Comparison of Proportions Calculator (Version 22.023; accessed March 21, 2024) was used. P < 0.05 was considered a significant difference.
RESULTS
During the study period, out of 925 patients attending the STIs clinic, 655 (70.8%) were from rural areas, and 270 (29.2%) were from urban areas. Among the rural cases, 604 (92.2%) were female and 51 (7.8%) were male, while among the urban cases, 219 (81.1%) were female and 51 (18.9%) were male. There was a significant difference in the proportion of STIs among males from urban areas compared to rural areas (P < 0.01). The majority of STIs cases from both rural and urban areas were aged between 20 and 40 years. However, the proportion of STI cases aged below 20 years was higher in urban areas (6.3%) compared to rural areas (2.7%) (P < 0.01).
In rural STI cases, 226 (34.5%) had education below 10th class, while in urban areas, 99 (36.7%) had education above 12th class. There was a significant difference in the education profile between rural and urban areas (P < 0.01), with a higher proportion of illiterate individuals in rural areas and a higher proportion of individuals with education above 10th class in urban areas. The majority of STI cases reported were homemakers both from rural (79.7%) and urban (64.1%) areas. The proportion of married cases with STIs was higher compared to unmarried cases in both rural and urban areas. The pregnant females in rural and urban were 1.9% and 3.3% respectively. The frequency distribution of the sociodemographic profile of the participants is shown in Table 1.
| Sociodemographic variables | Frequency (%) among the rural population (n=655) | Frequency (%) among the urban population (n=270) | P-value |
|---|---|---|---|
| Sex | |||
| Male | 51 (7.8) | 51 (18.9) | <0.01 |
| Female | 604 (92.2) | 219 (81.1) | |
| Age | |||
| Below 20 years | 18 (2.7) | 17 (6.3) | 0.06 |
| 20–30 years | 335 (51.1) | 124 (45.9) | |
| 31–40 years | 225 (34.4) | 90 (33.3) | |
| 41–50 years | 62 (9.5) | 33 (12.2) | |
| Above 50 years | 15 (2.3) | 6 (2.2) | |
| Education | |||
| Illiterate | 167 (25.5) | 21 (7.8) | <0.01 |
| Below 10th class | 226 (34.5) | 91 (33.7) | |
| 10th –12th class | 86 (13.1) | 59 (21.9) | |
| Above 12th class | 176 (26.9) | 99 (36.7) | |
| Occupation | |||
| House wife | 522 (79.7) | 173 (64.1) | <0.01 |
| Pvt Job | 94 (14.4) | 56 (20.7) | |
| Business | 14 (2.1) | 17 (6.3) | |
| Student | 25 (3.8) | 24 (8.9) | |
| Income | |||
| Up to 5K | 8 (1.3) | 2 (0.7) | <0.01 |
| 5K–10K | 498 (76.0) | 153 (56.7) | |
| 10K–20K | 95 (14.5) | 59 (21.9) | |
| 20K | 54 (8.2) | 56 (20.7) | |
| Marital status | |||
| Unmarried | 36 (5.5) | 33 (12.2) | <0.01 |
| Married | 619 (94.5) | 237 (87.8) |
Clinical symptoms based on a syndromic approach in rural and urban population
In a rural area, out of 655 cases of STIs, patients presented with lower abdomen pain in 81.7% of cases, followed by vaginal discharge in 17.1%, urethral discharge in 10.1%, cervical discharge in 4.9%, genital herpes in 4.3%, and genital ulcers secondary to syphilis in 3.7% [Figure 1]. In the urban area, out of 270 patients, clinical symptoms of lower abdomen pain were seen in 70% of cases, followed by vaginal discharge in 21.1%, urethral discharge in 11.1%, genital herpes in 10.4%, genital ulcers secondary to syphilis in 7.4%, and cervical discharge in 4.4% [Figure 1]. Genital herpes (P < 0.01) and genital ulcers secondary to syphilis (P = 0.01) were more common in urban areas. Retroviral HIV infection was present in 8 (1.2%) cases in the rural area and 3 (1.1%) cases in the urban area. Many patients presented with multiple clinical symptoms in both areas [Supplementary File 1].
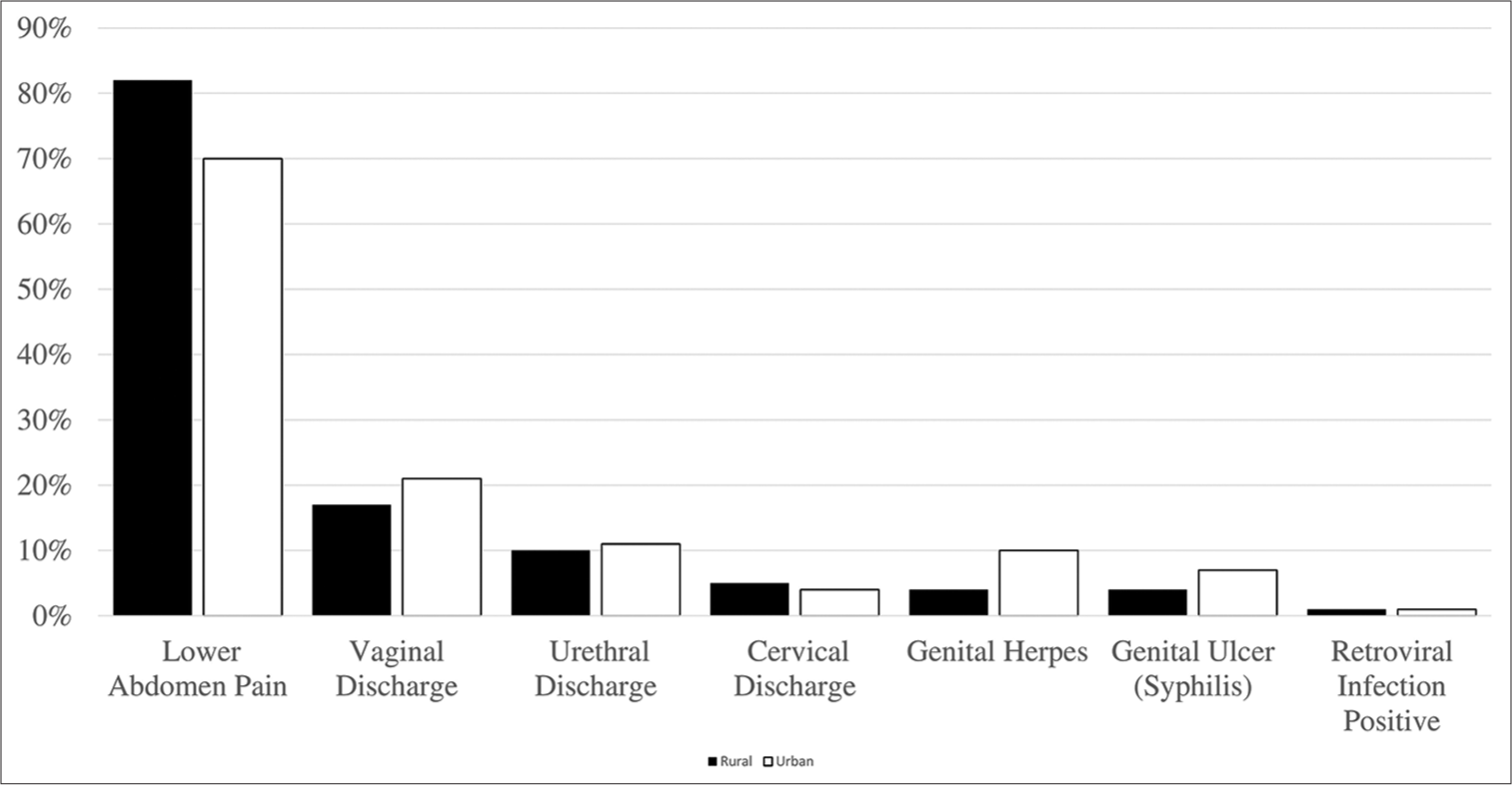
- The distribution of various clinical symptoms based on the syndromic approach between rural and urban area.
Comparison of sexual behavior between the rural and urban area
The mean age of onset (in years) of sexual activity in the rural population was 19.48 ± 4.09 years, while in urban areas, 20.20 ± 4.17, with a significant difference with P < 0.01. The mean duration of marriage (in years) in rural (14.27 ± 9.11) and urban (14.29 ± 9.69) had no statistical difference (P = 0.81). The majority of the patients in both rural (90.7%) and urban (92.2%) areas had presented to our clinic with the first episode (P = 0.45) STI. In 94.6% of rural and 89.6% of urban STIs, cases had a single partner. In 4.1% of rural and 8.8% of urban STIs, cases had multiple partners (P < 0.01). In 6.3% of rural and 8.1% of urban cases had a history of drug abuse before sexual activity (P = 0.32). In rural areas, the type of partners were regular (73.9%), casual (18.8%), sex worker (4.6%), and men sex with men (0.5%). Similarly, the distribution of sex partners in urban areas were regular (66.7%), casual (17.8%), sex worker (9.3%), and men sex with men (2.2%). The majority of the cases did not use any protection in their last contact in both the rural (97.7%) and urban (97%). In 4.6% of rural and 2.6% of urban STIs, cases had a symptomatic partner (P = 0.16). The mean duration since the last sexual contact in days in the rural was 21.16 ± 11.01 days, while in the urban was 20.29 ± 11.29 days with a statistical difference of P = 0.01. The details of the comparison of sexual behavior between both are mentioned in Table 2.
| Sexual behavior assessment parameters | Frequency (%) among the rural population (n=655) | Frequency (%) among the urban population (n=270) | P-value |
|---|---|---|---|
| Age of onset of sexual contact | |||
| Mean±SD in years | 19.48±4.09 | 20.20±4.17 | 0.004 |
| Median (range) in years | 18 (6–50) | 20 (5–35) | |
| Marital status | |||
| Married | 619 (94.5) | 237 (87.8) | <0.01 |
| Unmarried | 36 (5.5) | 33 (12.2) | |
| Duration of marriage | |||
| Mean±SD in years | 14.27±9.11 | 14.29±9.69 | 0.81 |
| Median (range) in years | 13 (1–55) | 13 (1–57) | |
| Number of episode | |||
| Single | 594 (90.7) | 249 (92.2) | 0.45 |
| Multiple | 61 (9.3) | 21 (7.8) | |
| Number of sexual partner | 0.01 | ||
| Multiple | 27 (4.1) | 24 (8.8) | |
| Single | 620 (94.6) | 242 (89.6) | |
| Denied | 8 (1.3) | 4 (1.6) | |
| Drug abuse before sex | |||
| Yes | 41 | 22 | 0.30 |
| No | 614 | 248 | |
| Type of partner | |||
| Casual | 123 (18.8) | 48 (17.8) | 0.03 |
| Regular | 484 (73.9) | 180 (66.7) | |
| Sex worker | 30 (4.6) | 25 (9.3) | |
| MSM | 3 (0.5) | 6 (2.2) | |
| Denied | 14 (2.2) | 11 (4.0) | |
| Protection used or not in last contact | |||
| Yes | 15 (2.3) | 8 (3) | 0.55 |
| No | 640 (97.7) | 262 (97) | |
| Symptoms in partner | |||
| No | 625 (95.4) | 263 | 0.16 |
| Yes | 30 (4.6) | 7 (2.6) | |
| Last contact | |||
| Mean±SD in days | 21.16±11.01 | 20.29±11.29 | 0.01 |
| Median (range) in days | 20 (1–180) | 18 (3–180) |
SD: Standard deviation
The occupation of the sexual partner in the rural area was as follows: Private job (222; 33.9%); business (156; 23.8%); farmer (80; 12.2%); driver (43; 6.6%); labor (39; 6%); government job (36; 5.5%); teacher (13; 2%); engineer (9; 1.4%); painter (6; 0.9%); student (4; 0.6%); carpenter (4; 0.6%); plumber (3; 0.5%); guard (2; 0.3%); and tailor (1; 0.2%). The occupation of the sexual partner in the urban area was as follows: Private job (77; 28.5%); business (72; 26.7%); government job (30; 11.1%); driver (14; 5.2%); teacher (12; 4.4%); engineer (7; 2.6%); student (7; 2.6%); labor (4; 1.5%); painter (4; 1.5%); farmer (3; 1.1%); tailor (2; 0.7%); carpenter (1; 0.4%); and guard (1; 0.4%).
DISCUSSION
This study provides a comprehensive review of the demographic, clinical, and behavioral characteristics of patients with STIs in rural and urban areas of the east-central part of India. Out of a total of 955 cases, 70.8% were from rural areas, and 29.2% were from urban areas. This disparity of representation can be explained based on the rural-urban gap, limited healthcare access, lack of health awareness, and resource constraints, thereby driving rural residents to seek better services in urban areas.[5] Similar findings were also seen in the study by Nandan et al., the prevalence of STIs cases in the rural population (49%) was higher compared to urban area (27%).[6] Female presented with STIs, majorly compared to males in both rural and urban areas, which is comparable with other studies.[7-12] The distribution of STIs among males was significantly different (P < 0.01), with a higher proportion of cases in the urban areas compared to rural areas could be due to access to/health facilities, awareness, and education of STIs in urban areas. The proportion of female cases with STIs was more in rural compared to urban areas due to differences in education, lack of health facilities, less frequent STIs screening visits by healthcare personnel, and social and cultural beliefs in our study, comparable with study by Masoumirad et al.[12]
The predominant age group in our study, presented with STIs, was 20–30 years, followed by 30–40 years in both the rural and urban areas, which was also consistent with various studies.[6,8,12,14,15] A higher proportion of cases aged below 20 years was seen in urban areas compared to rural areas (P < 0.01) access to social media leading to psychological factors, experimentation of sexual needs along with incorrect sex education information and an environment which make discuss sexuality are attributed to this in various studies.[11,16,17] There was a significant difference in the education profile between rural and urban areas, with illiterate more in rural areas and >10th class education profile in urban areas with similar findings in other studies.[14,15] In our study, STIs were more in female sex, married couples, young adults (20–40 years), housewife occupation, and low income groups in both areas. Similarly, in a study by Kosambiya et al. in Surat and Singh et al. in east-central India, the prevalence of STIs was higher in married housewife, lower education status, and young adults with income among the rural population.[4,13] In the study by Kannan et al. in Tamil Nadu, the prevalence of STIs was 44.6% in married women belonging to the age group of 15–45 years.[18] In a study by Sharma and Gupta, the rural female population of Himachal Pradesh showed significant STIs prevalence among the age group 25–34 years, married (52.4%), below 10th class education and housewives with agriculture background.[19] In a study by Philip et al., in urban females, the population of Ludhiana showed STIs majorly among age group 24– 25 years, housewives, monthly income ≥1000, and education profile of illiterate and primary level.[20]
Lower abdomen pain was the predominant clinical symptom as per the syndromic approach, followed by vaginal discharge in both the rural and urban areas, which was contradictory with other studies showing vaginal, cervical, or urethral discharge as most common, followed by genital ulcer.[8,21-23] However, in comparison, genital ulcers secondary to herpes and syphilis were more prevalent in urban areas. This could be due to differences in socio-cultural beliefs, education status, awareness level, sexual behavior, and lack of primary health care facilities among the east-central regions compared to other regions of India, which would have led to a delayed presentation like complications, such as pelvic inflammatory disease causing lower abdomen pain, at our STIs center, which is the highest referral center in the region.
There was a difference in the sexual behavior pattern among the cases of STIs between the rural and urban areas in our study. Sexual behavior parameters such as early age of onset of sexual activity, less cases of multiple sexual partners, and increased duration of gap of last sexual encounter were seen in rural population compared to urban areas. The STI cases in urban areas, despite having late onset of sexual activity, people were more engaged in high-risk behavior – like sexual contact with sex workers (11.5%), multiple partners (8.8%), unprotected sexual activity (97%), frequent sexual engagement, and drug abuse (8.2%), which also attribute to higher incidence of STIs in young adult below 20 years of age. In a study by Carey et al., 25% of patients on treatment for drug abuse or alcohol had suffered once in a lifetime with STIs.[24] A study by Ranjan et al, in the rural population of Bihar showed 5-10% of males had multiple sexual partners. Predominant partners were female, mainly being sisters-inlaw, agricultural laborers, friend’s wife and sex workers.[25] The sexual partners for women were brothers-in-law, distant relatives, and rich landlords. In a study by Singh et al. in the rural population of east-central India, the sexual partner was predominantly regular partner (78%), sex worker (8.5%), and causal partner (7.6%), which is similar to our study in the rural population.[13] The majority of patients not frequently taking precautions before engaging in sexual activity was consistent with other studies.[17] In our study, in both the rural and urban areas, the sexual partner’s occupation was a private job followed by business. However, farmers were the third common occupation of the partner in rural area while it was a government job in urban area.
Limitation of our study
The hospital-based setting, retrospective design, re-call biases, absence of microbiological confirmation are significant limitations that constrain the generalizability of the study findings to the general population.
CONCLUSION
This study highlights the differences in sociodemographic profile, STIs patterns, and sexual behaviors between rural and urban populations in the east-central zone of India. The findings underscored the need for interventions to address the higher prevalence of STIs in rural areas as compared to urban areas. The difference in education, occupation, and income level highlights the disparities in the sociodemographic profile of STIs cases between rural and urban areas.
Ethical approval
The Institutional Review Board approval was waived off in view of retrospective design of the study.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Prevention, management and control of reproductive tract infections and sexually transmitted infections New Delhi: Ministry of Health and Family Welfare Government of India; 2014.
- [Google Scholar]
- Urban-rural inequities in the parental attitudes and beliefs towards human papillomavirus infection, cervical cancer, and human papillomavirus vaccine in Mysore, India. J Pediatr Adolesc Gynecol. 2018;31:494-502.
- [CrossRef] [PubMed] [Google Scholar]
- Reproductive health service utilization and social determinants among married female rural-to-urban migrants in two metropolises, China. J Huazhong Univ Sci Technolog Med Sci. 2016;36:904-9.
- [CrossRef] [PubMed] [Google Scholar]
- RTI/STI prevalence among urban and rural women of Surat: A community-based study. Indian J Sex Transm Dis AIDS. 2009;30:89-93.
- [CrossRef] [PubMed] [Google Scholar]
- What explains the rural-urban gap in the use of hygienic methods of menstrual protection among youth in the East Indian State of Bihar? Indian J Community Med. 2022;47:182-6.
- [CrossRef] [PubMed] [Google Scholar]
- Estimation of prevalence of RTIs/STDs among women of reproductive age group in district Agra. Indian J Community Med. 2002;27:110.
- [Google Scholar]
- A crosssectional study on healthseeking behavior in relation to reproductive tract infection among evermarried rural women in Kancheepuram district, Tamil Nadu. J Family Med Prim Care. 2021;10:34248.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern of sexually transmitted infections: A profile from a rural-and tribalbased sexually transmitted infections clinic of a tertiary care hospital of Eastern India. J Family Med Prim Care. 2018;7:10426.
- [CrossRef] [PubMed] [Google Scholar]
- National STI/RTI Control and Prevention Programme. 2007. India: NACP; Phase III Available from: https://naco.gov.in/sites/default/files/STI-Report_7.pdf [Last accessed on 2022 Dec 23]
- [Google Scholar]
- Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site. PLoS Med. 2018;15:e1002512.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern and clinico-epidemiological profile of female patients of RTI/STIs attending an STI clinic in Uttarakhand, India. J Family Med Prim Care. 2022;11:7357-61.
- [CrossRef] [PubMed] [Google Scholar]
- Use of sexual and reproductive health services among women living in rural and urban Oregon: Impact of the affordable care act medicaid expansion. J Womens Health (Larchmt). 2023;32:300-10.
- [CrossRef] [PubMed] [Google Scholar]
- Syndromic diagnosis, sexual behavior, and management in rural population among all cases attending sexually transmitted infection clinic in a tertiary care center from the east-central zone of India: A retrospective study. Indian J Sex Transm Dis AIDS. 2024;45:34-8.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of reproductive tract infections and sexually transmitted diseases in India: Levels and differentials. J Fam Welfare. 2011;57:48-59.
- [Google Scholar]
- A comparative study of prevalence of RTI/STI symptoms and treatment seeking behaviour among the married women in Urban and Rural Areas of Delhi. Int J Reprod Med. 2015;2015:563031.
- [CrossRef] [PubMed] [Google Scholar]
- Rashtriya Kishor Swasthya Karyakram. 2014. Adolescent health Division Ministry of Health and Family Welfare Government of India. Available from: https://nhm.gov.in/images/pdf/programmes/RKSK/RKSK_Strategy_Handbook.pdf [Last accessed on 2023 Apr 11]
- [Google Scholar]
- Pattern of sexual behavior in adolescents and young adults attending STD clinic in a tertiary care center in South India. Indian J Sex Transm Dis AIDS. 2017;38:171-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of reproductive tract infections among recently married women in Veerapandi Panchayat union of Salem district, Tamil Nadu. Indian J Community Med. 2007;32:144-5.
- [CrossRef] [Google Scholar]
- The prevalence of reproductive tract infections and sexually transmitted diseases among married women in the reproductive age group in a rural area. Indian J Community Med. 2009;34:62-4.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of symptoms suggestive of reproductive tract infections/sexually transmitted infections in women in an urban area of Ludhiana. Indian J Sex Transm Dis AIDS. 2013;34:83-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sexually transmitted infections based on the syndromic approach in Gondar town, northwest Ethiopia: A retrospective study. BMC Public Health. 2013;13:143.
- [CrossRef] [PubMed] [Google Scholar]
- Study of syndromic management approach in the management of sexually transmitted diseases in rural population. Indian J Sex Transm Dis AIDS. 2012;33:146-7.
- [CrossRef] [PubMed] [Google Scholar]
- High prevalence of gynaecological diseases in rural Indian women. Lancet. 1989;1:85-8.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for sexually transmitted infections at a DeAddictions service in South India. Drug Alcohol Depend. 2006;82:127-34.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern of sexual behavior among people in a rural area of Bihar: A qualitative study on wives of migrant workers. J Family Med Prim Care. 2019;8:1637-41.
- [CrossRef] [PubMed] [Google Scholar]






