Translate this page into:
Serpiginous plaques: An atypical presentation of secondary syphilis in human immunodeficiency virus
*Corresponding author: Sudhesshna Devi, Department of Dermatology, Saveetha Medical College and Hospital, Saveetha Institute of Medical and Technical Sciences University, Thandalam, Tamil Nadu, India dr.sudhesshnaderma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Devi S, Bhat RM. Serpiginous plaques: An atypical presentation of secondary syphilis in human immunodeficiency virus. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_93_2024
Abstract
Syphilis is known to run its natural course unless intervened, and the severity of clinical presentation in human immunodeficiency virus (HIV) co-infection is well established. Here, we report the case of a 47-year-old male on antiretroviral therapy for 9 years, who presented with a persistent serpiginous plaque over the neck, along with painless genital ulcers and painful oral ulcers. These lesions resolved rapidly after three doses of benzathine penicillin with subsequent follow-up showing declining Venereal Disease Research Laboratory titers. This case highlights the atypical presentation of syphilis and the need for a high index of suspicion while approaching cutaneous manifestations in HIV.
Keywords
Human immunodeficiency virus
Penicillin
Serpiginous plaques
Syphilis
INTRODUCTION
Syphilis is a sexually transmitted infection caused by an obligate intracellular spirochete, Treponema pallidum, known for its ability to evade the host immune system.[1] Syphilis poses a diagnostic conundrum as it modifies the clinical and serological markers with a myriad of unusual presentations in human immunodeficiency virus (HIV) co-infection. In this report, we describe an atypical manifestation of secondary syphilis that was misdiagnosed as dermatophytosis by a physician due to its mimetic potential. However, the bizarre presentation and serologic screening clinched the diagnosis of this great imitator.
CASE REPORT
A 47-year-old married male presented to our tertiary care center with a 3-month history of asymptomatic reddish lesions over the neck, chin, and forearms, which were initially diagnosed as dermatophytosis by his general physician and treated with antifungals without clinical improvement. This caused a delay in seeking dermatological evaluation, and the disease gradually progressed to involve the genital and oral mucosa with painful ulcers. Past medical history revealed HIV diagnosed 9 years ago, for which the patient has been on regular antiretroviral therapy with tab. Zidovudine 300 mg, tab. lamivudine 150 mg, and tab. nevirapine 200 mg. Since his diagnosis of HIV, he has proclaimed consistent use of condoms and reported that his last sexual activity occurred 5 years ago with his spouse, after which he has abstained from sexual intercourse. He denies any history of high-risk sexual behavior, and there was no history of similar complaints in the partner. In addition, the patient had no history of substance abuse or blood transfusions.
On dermatological examination, multiple discontinuous arcuate and serpiginous indurated erythematous plaques with scaling over the neck, chin, and right flexor aspect of the forearm with a positive Buschke-Ollendroff sign were noted [Figure 1]. Palms and soles were uninvolved. The patient also had four moist, flat-topped eroded papules over the prepuce [Figure 2] and healed atrophic scars with few eroded plaques on the ventral shaft of the penis and scrotum [Figure 3]. Multiple irregular linear erosions consistent with snail track ulcers were noted on the hard palate, and a few mucous patches were also observed on the lower gingival and lip mucosa [Figure 4]. Non-tender lymphadenopathy involving the right submandibular and the bilateral inguinal group of lymph nodes was observed. These findings raised a strong suspicion of secondary syphilis in the background of HIV co-infection. His ophthalmic, auditory, neurological, and other systemic examinations did not reveal any abnormality.

- Multiple discontinuous arcuate and serpiginous indurated erythematous plaques with scaling noted over the neck.

- Moist flat-topped exuberant eroded papules over the prepuce.

- Healed atrophic scars with few eroded plaques were noted on the ventral shaft of penis and scrotum.
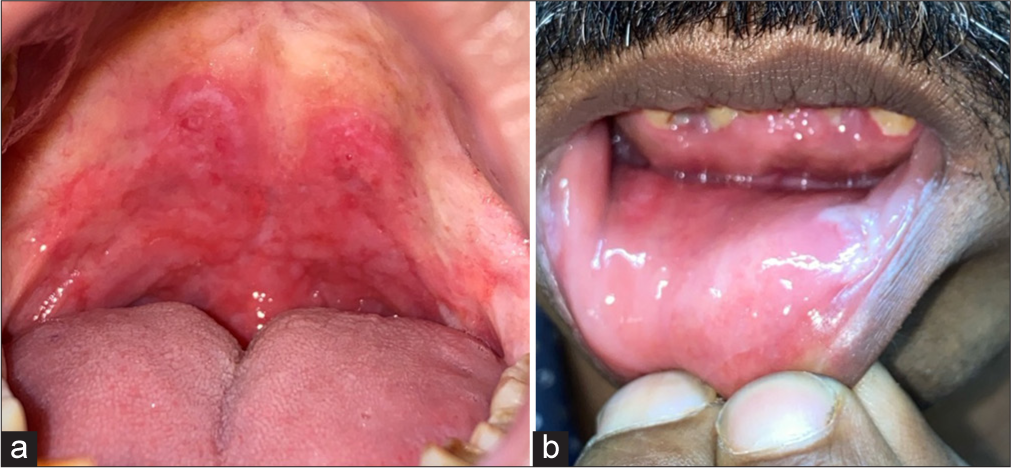
- (a): Multiple irregular linear erosions consistent with snail track ulcers were noted on the hard palate; and (b): few mucous patches noted over the lower labial and gingival mucosa.
Dark ground microscopy for T. pallidum performed on the mucosal lesion was negative. Routine investigations such as complete hemogram, chest X-ray, urine analysis, and liver and renal function tests were within normal limits. Serological tests for hepatitis B and C were negative. However, his rapid plasma reagin (RPR) test was reactive in 1:256 dilution, and the T. pallidum hemagglutination test was positive (>5120), confirming the diagnosis of secondary syphilis. Histopathological examination from the neck lesion revealed hyperkeratosis with acanthosis in the epidermis and lymphocytes with sparse plasma cell infiltration in the dermis, supporting the diagnosis [Figure 5]. His CD4 count was 527 cells/μL. Partner screening returned negative results for RPR and treponema pallidum haemagglutination assay (TPHA). The patient was treated with benzathine penicillin G 2.4 million units intramuscularly, administered in two divided doses on each buttock at weekly intervals for 3 weeks. The patient improved symptomatically and achieved clinical remission of skin and mucosal lesions within 3 weeks [Figure 6]. Three and half months later, the patient visited the hospital, and a repeat RPR titer indicated a declining value of 1:64, signifying the clinical and serological resolution of the disease. However, he did not attend the subsequent follow-up visits as advised.
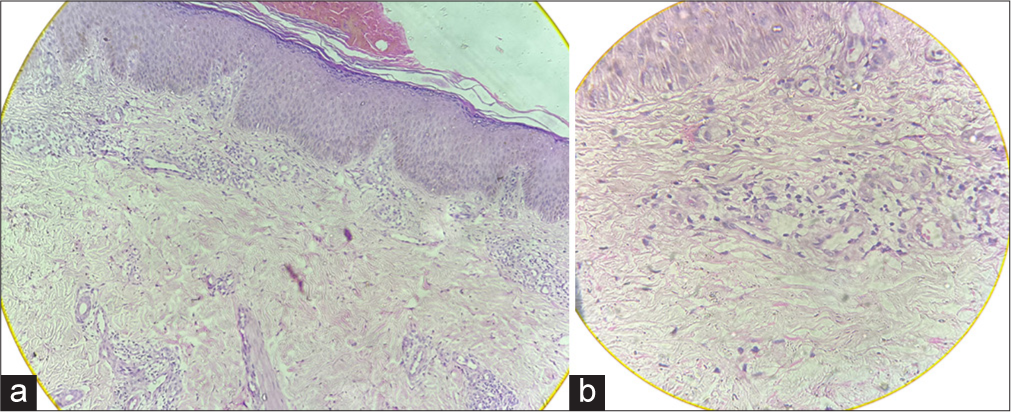
- Histopathology. (a): H&E x10, epidermis shows basket weave orthokeratosis with crusting and acanthosis, dermis shows perivascular and periadnexal infiltrate composed of lymphocytes, histiocytes, polymorphs, and few plasma cells; (b): H&E ×40 shows the perivascular dermal infiltrates composed of lymphocytes, histiocytes, and few plasma cells. H&E: Hematoxylin and eosin.
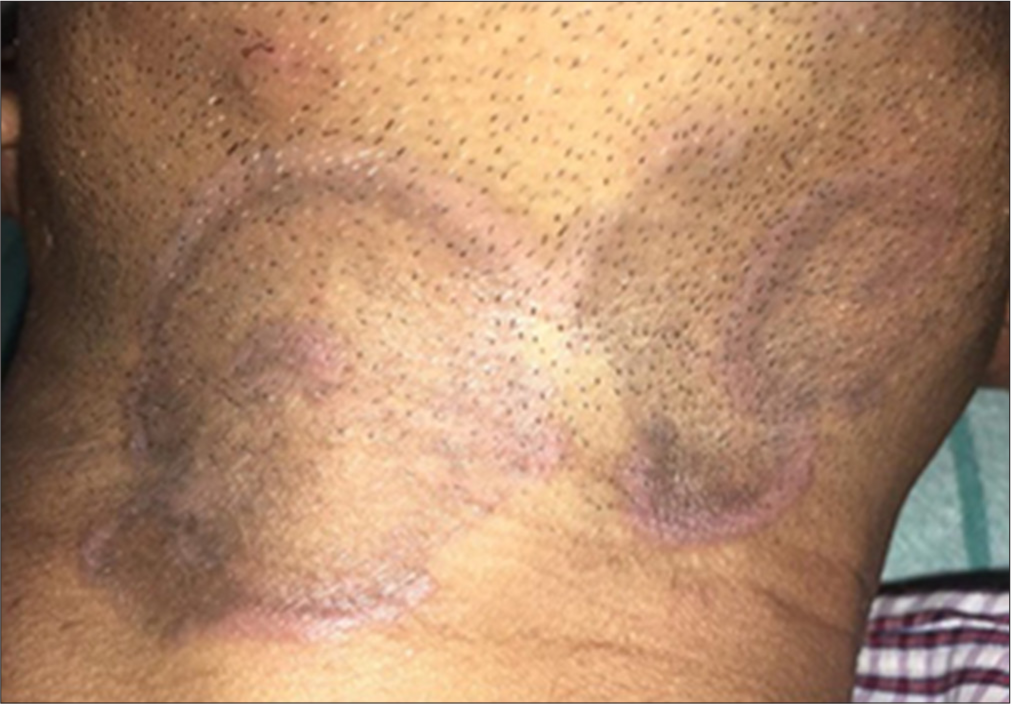
- Post-treatment resolution of lesions within one week.
DISCUSSION
Syphilis is an ancient, systemic disease that prevails as a public health problem despite the availability of effective treatment,[2] which could be attributed to the versatility in presentation and delay in diagnosis. The interaction between syphilis and HIV is complex. While the former augments the risk of HIV transmission,[3] the latter affects the course, evolution, diagnosis, and treatment response in syphilis through immune modulation.[4] The natural course of syphilis evolves through primary, secondary, latent, and tertiary stages when left untreated,[5] and the secondary stage is the paradigm of diverse morphological presentation, especially in concurrent HIV infection.
Our case illustrates the atypical and florid manifestation of secondary syphilis lesions in HIV co-infection. A relapse of secondary syphilis can be considered in this patient due to the last reported sexual contact 5 years ago, the presence of HIV-co-infection, and markedly elevated VDRL and TPHA titers. The occurrence of secondary syphilis despite the absence of recent sexual contact may be explained by several factors, such as untreated early syphilis progressing to a latent phase with subsequent relapse and clinical reactivation, or the possibility of an undisclosed recent sexual encounter.[6] In addition, immunological alterations associated with HIV can facilitate the reactivation of latent syphilis, resulting in atypical and recurrent manifestations accompanied by persistently high serological titers.[1] The negative dark field microscopy result in our case could be attributed to the patient’s use of topical antibiotic cream on the mucosal lesions at the time of presentation.
An initial cerebrospinal fluid (CSF) analysis was not performed as the patient did not consent for it. Also, there were no neurological symptoms or signs at the time of evaluation.[7] The role of CSF analysis in cases of syphilis is a topic of debate.[8,9] In the presence of HIV co-infection, a CSF examination can be valuable during the initial visit and follow-up if the CD4 count < 350/L or when non-treponemal titers are persistently high or increasing despite adequate treatment of early syphilis. This is especially relevant as neurosyphilis carries an increased risk in HIV-positive individuals and may present or co-exist with early stages of syphilis.[7] Our patient did not consent for a CSF analysis during follow-up and did not return for subsequent visits, thereby limiting the scope for further diagnostic investigation.
Syphilis in HIV-positive individuals often presents with overlapping or co-existing early stages of the disease, more florid presentation at each stage, an increased incidence of malignant syphilis,[8] and a higher likelihood of rapid progression or concurrent neurosyphilis during the primary and secondary stages.[9] Diagnosis can be challenging, as post-treatment serologic titers may remain higher than expected, fluctuate, or produce false-negative results, and delayed seroreactivity has also been reported.[10] The management of syphilis in HIV co-infected individuals is similar to non-infected individuals. While a single dose of benzathine penicillin G is recommended as the treatment for secondary syphilis in HIV,[7] we opted for three-dose regimen due to the florid presentation and possibly a longer duration of disease.[11] After three doses, he improved significantly, as evidenced by clinical resolution and the declining VDRL titers.
As secondary syphilis mimics several other dermatological conditions[2,12,13] and has a potential to relapse, especially in HIV co-infection as observed in our patient, a differential diagnosis of secondary syphilis should be considered in all atypical presentations of common dermatoses, and concomitant HIV must be ruled out in aggressive presentation of typical lesions. The spirochete’s ability to evade detection, even by experienced physicians, necessitates maintaining a low threshold of suspicion in patients with HIV co-infection, given the recent global resurgence of the disease.[14,15]
CONCLUSION
Uncommon clinical presentations, relapse, and recurrence have become increasingly common in secondary syphilis, particularly in the context of HIV. The atypical presentation of serpiginous plaques associated with relapse, which has not been widely documented in the literature, highlights the evolving and deceptive nature of secondary syphilis. This case emphasizes the importance of recognizing the unusual morphological and serological presentations of syphilis, especially in immunocompromised individuals.
Ethical approval
The research/study was approved by the Institutional Ethics Committee at Father Muller Medical College, number FMIEC/CCM/05/2021, dated April 01, 2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Syphilis and HIV: A dangerous combination. Lancet Infect Dis. 2004;4:456-66.
- [CrossRef] [PubMed] [Google Scholar]
- A case of secondary syphilis mimicking palmoplantar psoriasis in HIV infected patient. An Bras Dermatol. 2015;90:216-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of syphilis infection on HIV acquisition: A systematic review and meta-analysis. Sex Transm Infect. 2021;97:525-33.
- [CrossRef] [PubMed] [Google Scholar]
- Syphilis treatment in the presence of HIV: The debate goes on. Curr Opin Infect Dis. 2015;28:44-52.
- [CrossRef] [PubMed] [Google Scholar]
- Infectious syphilis In: Gupta S, Kumar B, eds. Sexually Transmitted Infections (2nd ed). New Delhi: Elsevier; 2012. p. :429-57. Ch. 36
- [Google Scholar]
- Relapse of secondary syphilis after benzathine penicillin G: Molecular analysis. Sex Transm Dis. 2004;31:196-9.
- [CrossRef] [PubMed] [Google Scholar]
- Centers for disease control and prevention's sexually transmitted diseases infection guidelines. Clin Infect Dis. 2022;74(74 Suppl 2):S89-94.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of asymptomatic neurosyphilis in patients with latent syphilis: A 4-year retrospective study from a tertiary care center. J Skin Sex Transm Dis. 2024;6:54-6.
- [CrossRef] [Google Scholar]
- Letter in response to Frequency of asymptomatic neurosyphilis in patients with latent syphilis: A 4-year retrospective study from a tertiary care center. J Skin Sex Transm Dis. 2024;6:62-3.
- [CrossRef] [Google Scholar]
- Syphilis and HIV infection: An update. Clin Infect Dis. 2007;44:1222-8.
- [CrossRef] [PubMed] [Google Scholar]
- Erroneous treatment of syphilis with benzyl penicillin in an era with benzathine benzylpenicillin shortages. Sex Transm Infect. 2020;96:552.
- [CrossRef] [PubMed] [Google Scholar]
- Syphilis cornee mimicking lichen planus clinically and histologically. Indian J Sex Transm Dis. 2018;39:130-2.
- [CrossRef] [PubMed] [Google Scholar]
- Syphilis mimicking tinea imbricata and erythema annulare centrifugum in an immunocompromised patient. J Am Acad Dermatol. 2009;61:165-7.
- [CrossRef] [PubMed] [Google Scholar]
- Syphilis: Is it making resurgence? Indian J Sex Transm Dis AIDS. 2015;36:178-81.
- [CrossRef] [PubMed] [Google Scholar]
- Resurgence of syphilis, the great imitator. Med J Armed Forces India. 2022;78:131-5.
- [CrossRef] [PubMed] [Google Scholar]







