Translate this page into:
A rare case of purpura fulminans in an adult: Invasive meningococcal disease
*Corresponding author: Anuja Wijesundera, Department of Dermatology, Base Hospital, Wathupitiwala, Sri Lanka. anujaamarakoon@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wijesundera A, Liyanage DH, Fernando RP, Priyadarshika UR. A rare case of purpura fulminans in an adult: Invasive meningococcal disease. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_60_2024
Abstract
Purpura fulminans (PF) is a life-threatening dermatological condition characterized by acute purpuric lesions and skin necrosis due to microvascular thrombosis. In adults, PF is most commonly triggered by severe sepsis, particularly caused by Neisseria meningitidis. Invasive meningococcal disease (IMD) frequently leads to PF in children but is rare in adults. Early recognition and treatment are essential to avoid severe outcomes. We present a rare case of PF in an adult with IMD, successfully treated without long-term complications. A 32-year-old woman with epilepsy, recently adjusted on higher doses of carbamazepine, presented with fever, vomiting, and convulsions. Her condition worsened with the development of high fever (40°C), hypotension, and generalized tonic-clonic seizures. Physical examination showed purpuric and petechial skin lesions on her limbs and extremities. Initial differential diagnoses included infectious PF (bacterial, particularly meningococcal or rickettsial), toxic epidermal necrolysis, and vasculitis. Laboratory findings revealed elevated C-reactive protein and neutrophil leukocytosis. Blood cultures confirmed N. meningitidis, and a skin biopsy demonstrated neutrophilic vasculitis with thrombosis consistent with PF. The patient was initially treated with intravenous fluids and empirical antibiotics (cefotaxime and doxycycline). After blood cultures isolated meningococci with sensitivity to cefotaxime, doxycycline was omitted. Despite the initial neurological decline, intensive care management resulted in full recovery. Necrotic skin lesions required specialized wound care and surgical debridement. Chemoprophylaxis was administered to close contacts and healthcare staff. IMD is a serious global health issue, with approximately 1.2 million cases reported annually. PF, a rare but severe complication of IMD, leads to skin necrosis and is associated with disseminated intravascular coagulation. Although predominantly affecting children, PF in adults remains rare, particularly in regions with low incidence of meningococcal disease. Diagnosis is based on clinical presentation, laboratory results, and microbial identification. In this case, blood cultures and polymerase chain reaction confirmed N. meningitidis, and the patient responded well to cefotaxime, consistent with known sensitivity patterns. PF is a severe manifestation of meningococcal disease. Early identification and aggressive treatment are critical for favorable outcomes. This case underscores the need for clinical vigilance, a multidisciplinary approach, and the efficacy of timely antibiotic intervention in managing meningococcal infections.
Keywords
Case report
Meningococcal
Neisseria meningitidis
Purpura fulminans
INTRODUCTION
Purpura fulminans (PF) is a rare, life-threatening medical emergency characterized by rapid progression of skin necrosis secondary to microvascular thrombosis.
PF occurs in three distinct clinical contexts: Neonatal, idiopathic, and acute infectious types. Among adults, the most common form is acute infectious PF (AIPF), which is typically triggered by severe bacterial sepsis, particularly by endotoxin-producing organisms such as Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus.[1,2] Rare cases of PF due to rickettsial infection have also been reported in Sri Lanka.[3] Invasive meningococcal disease (IMD) remains one of the most recognized triggers of PF.[2] The estimated incidence of PF in patients with IMD ranges from 5% to 25%, with mortality rates reaching between 20% and 70%.[2]
CASE REPORT
A 32-year-old woman presented to the emergency department with a 1-day history of fever, vomiting, and generalized tonic-clonic seizures. She is a known epileptic, managed with anticonvulsants (carbamazepine and clobazam) for 12 years of age. Her dose of carbamazepine had been increased recently due to breakthrough seizures. She had no recent history of respiratory infections, travel, or exposure to individuals with known meningococcal disease. She is not a diabetic or known to have any other immunocompromised state.
On initial assessment, the patient was febrile with a temperature of 40°C, tachycardic (pulse 114/min), hypotensive (blood pressure 78/48), and had a respiratory rate of 20 breaths/min with an oxygen saturation of 99% on room air. She was fully conscious with a Glasgow Coma Scale score of 15/15 and exhibited purpuric and ecchymotic lesions over the extremities of limbs, particularly over the heels, ankles, dorsi of feet, shins, and forearms. There were petechial lesions on the palms of both hands. The skin lesions were well demarcated with reticulate borders exhibiting moderate-to-severe cutaneous tenderness [Figure 1]. Genital areas were not involved. Neurological examination revealed no photophobia, neck stiffness, or signs of meningeal irritation.

- (a-b) Skin on the second day of the illness, including petechial, ecchymotic, and purpuric lesions.
Given the rapid onset of fever, skin lesions, and seizures, the initial differential diagnosis was as follows:
AIPF: Likely triggered by sepsis, particularly meningococcal or rickettsial
Toxic epidermal necrolysis (TEN): Given her recent increase in carbamazepine dosage, drug-induced TEN was considered
Vasculitis: Autoimmune process causing cutaneous and systemic vasculitis.
Initial laboratory investigations revealed neutrophilic leukocytosis, with a white blood cell (WBC) count of 20.5 × 109/L with 90% neutrophils. Her C-reactive protein (CRP) was elevated at 203 mg/L and rose sharply to 503.5 mg/L by the 2nd day of hospitalization. Random blood sugar was 90 mg/dL and blood urea was 4.7 mmol/l. Serum bicarbonate level was within the normal range, being 25 mEq/L. Her liver function tests and coagulation profiles were within normal limits. D dimer level performed to rule out disseminated intravascular coagulation (DIC) was 300 ng/mL. Considering drug-induced TEN, The SCORTEN score to estimate the severity of illness was calculated and was zero.
Blood and urine cultures were taken soon after admission to identify a potential infectious source, and she was screened for rickettsial infections. A skin biopsy was performed to look for an etiology. A direct smear from skin lesions over the heel was taken for microscopy and culture.
Within 24 h, Gram-negative diplococci were detected in her blood smear, raising strong suspicion of N. meningitidis infection, confirmed by subsequent blood cultures grown in chocolate agar with antibiotic sensitivity tests showing susceptibility to cefotaxime [Figure 2]. Polymerase chain reaction assay detected bacterial DNA of N. meningitidis, which confirmed the diagnosis. Both gram stain and culture of the direct smear from skin lesions taken one day after starting antibiotics showed negative results.
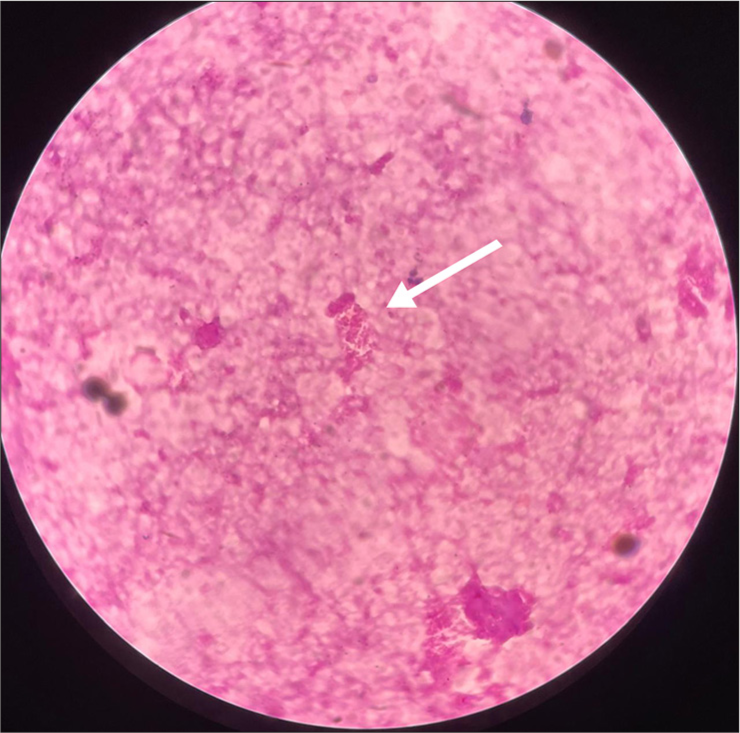
- Gram-negative diplococci in blood film. Gram stain ×1000.
The punch skin biopsy from the edge of a developing lesion over the right foot demonstrated neutrophilic vasculitis with thrombi formation in capillaries and small veins, consistent with PF secondary to meningococcal septicemia [Figure 3].
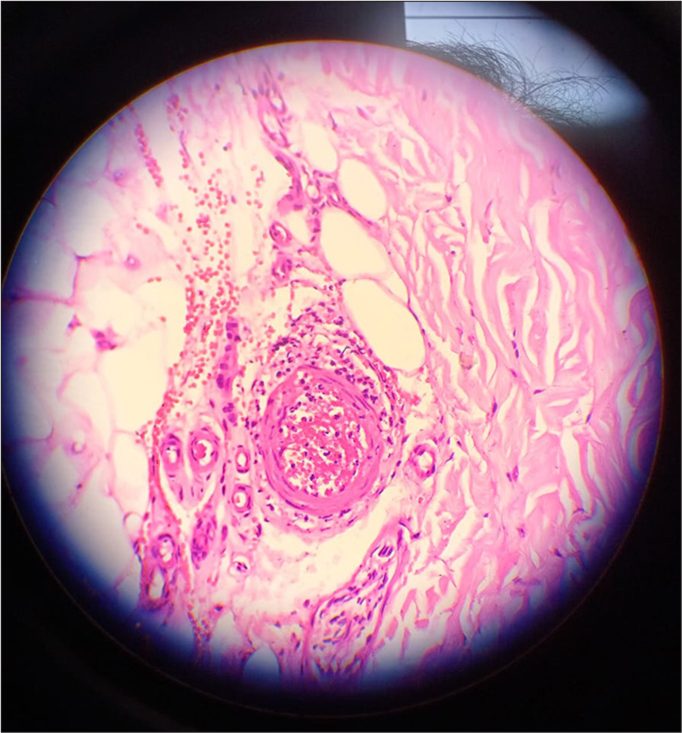
- Skin biopsy showing thrombi in vessels and neutrophilic vasculitis. hematoxylin and eosin ×10.
The patient was initially resuscitated with intravenous fluid boluses and drips, which stabilized her vital parameters. Empirical antibiotic therapy with intravenous cefotaxime and oral doxycycline was initiated while awaiting culture results.
On day two, the patient’s level of consciousness fluctuated, becoming drowsy and lethargic. Upon receipt of the blood culture results, her antibiotics were adjusted by continuing intravenous cefotaxime 2 g every 12 h and omitting doxycycline. Within 48 h, her CRP levels began to decrease, falling to 400 mg/dL, and her total WBC count normalized to 12 × 109/L. Her fever also began to subside, though intermittent spikes persisted.
Considering the deteriorating level of consciousness, she was transferred for intensive care on 4th day after admission, where she received continued antibiotics for 14 days in addition to supportive therapy, and she recovered without any serious complication or sequelae. Some of her skin patches progressed to flaccid bullae, which later turned into necrotic areas and slough formation [Figure 4]. There was cutaneous necrosis noted over both heels and the left 4th and 5th toes, with signs of early digital gangrene. After regular wound debridement and removal of necrotic areas by the surgical team, her wounds improved within 6-8 weeks [Figure 5].

- Skin lesions at three weeks after presentation showing necrotic areas.

- Healing wound on left heel at eight weeks.
All the healthcare staff who handled the patient and her close contacts were given oral ciprofloxacin as prophylaxis. Her condition was notified to relevant authorities according to local protocol.
DISCUSSION
IMD is a global public health concern, causing significant morbidity and mortality, especially in developing regions such as sub-Saharan Africa. Worldwide, there are an estimated 1.2 million cases annually, resulting in approximately 135,000 deaths.[4]
In Sri Lanka, although meningitis, by all causes, is a notifiable disease, pathogen-specific surveillance is not in place.[5] Between 1,000 and 1,500 cases of meningitis are reported annually[6] which includes both viral and bacterial meningitis cases, although the number of IMD cases within this group is not known. A study in 2019–2020 documented eleven cases of IMD over an 8-month period.[5]
Although we were unable to identify any in our case, usual risk factors for developing IMD are young age, living in crowded households or communal settings, weakened immunity, lack of spleen, recent respiratory infection, smoking, genetic susceptibility, travel to high-risk areas, and certain occupations with high risk of exposure like laboratory handlers.[7]
N. meningitidis is a Gram-negative diplococci with a polysaccharide capsule. It produces endotoxin lipooligosaccharide that induces a strong inflammatory response. Asymptomatic nasopharyngeal carriers are presumably the major source of infection.
There are 12 known serogroups of N. meningitidis, but commonly six serogroups (A, B, C, W135, X, Y) are associated with most IMD cases worldwide.[8]
Meningococcal PF involves N. meningitidis adhering to endothelial cells, leading to prothrombotic responses such as tissue factor activation, von Willebrand factor release, and impaired anticoagulant systems, including protein C and thrombomodulin. This adhesion triggers endothelial dysfunction, promoting microvessel thrombosis and hemorrhagic necrosis. The presence of bacterial endotoxins and high levels of inflammatory cytokines further exacerbate the coagulation cascade. PF’s development is not solely due to DIC but is driven by these specific bacterial-host interactions.[9]
Diagnosis of IMD relies on a high index of suspicion, particularly in patients presenting with acute febrile illness, purpura, and signs of shock. In our patient, the combination of neutrophilic leukocytosis, elevated CRP, and Gram-negative diplococci in the blood smear helped confirm the diagnosis early. A recent study done in Sri Lanka revealed that N. meningitidis serogroup B was the most common type which showed excellent susceptibility to cefotaxime and meropenem, whereas only 25% showed susceptibility to penicillin.[8] Blood culture sensitivity to cefotaxime of our patient was also in line with this study.
In managing septic shock, antibiotics, fluid resuscitation, vasopressors, and coagulopathy correction with fresh frozen plasma or platelets are essential. Extensive necrosis may require surgical debridement or amputation. Activated protein C may reduce mortality and amputation risk.[2]
Vaccination against meningococcal disease is a critical preventive strategy, particularly for at-risk populations and children. Chemoprophylaxis for close contact with infected individuals is also recommended during outbreaks.
CONCLUSION
PF secondary to IMD is a rare, life-threatening condition in adults. Clinicians should be alert to sudden purpuric rashes with systemic infection signs, particularly in regions with sporadic IMD cases. Recent outbreaks and resistant strains suggest the need for meningococcal vaccines in national immunization programs.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Purpura fulminans. 2020. Treasure Island, FL: StatPearls Publishing; Available from: https://www.ncbi.nlm.nih.gov/books/NBK532865 [Last accessed on 2024 Oct 12]
- [Google Scholar]
- Purpura fulminans in meningococcal septicaemia in an adult: A case report. Ann Burns Fire Disasters. 2010;23:43-7.
- [Google Scholar]
- Rare presentation of rickettsial infection as purpura fulminans: A case report. J Med Case Rep. 2018;12:145.
- [CrossRef] [PubMed] [Google Scholar]
- Global epidemiology of invasive meningococcal disease. Popul Health Metr. 2013;11:17.
- [CrossRef] [PubMed] [Google Scholar]
- Case series of meningococcal sepsis; are we seeing the real picture. Sri Lankan J Infect Dis. 2021;11:94-4.
- [CrossRef] [Google Scholar]
- Epidemiology and diagnosis of viral and bacterial central nervous system infections in Sri Lanka: A narrative review. Sri Lankan J Infect Dis. 2023;13:33.
- [CrossRef] [Google Scholar]
- Case-control study of risk factors for meningococcal disease in Chile. Emerg Infect Dis. 2017;23:1070-8.
- [CrossRef] [PubMed] [Google Scholar]
- Antimicrobial susceptibility and serotypes of Neisseria meningitidis and Streptococcus pneumoniae in Sri Lanka: Experience from the National reference laboratory. Asian Pac J Trop Med. 2022;15:114-4.
- [CrossRef] [Google Scholar]
- Pathogenesis of meningococcal purpura fulminans. Pathog Dis. 2017;75:3.
- [CrossRef] [PubMed] [Google Scholar]






