Translate this page into:
Asymptomatic skin lesions as a diagnostic clue in multiple myeloma – A case report
*Corresponding author: Anjana Jayaprakash, Department of Dermatology, Pushpagiri Institute of Medical Sciences, Thiruvalla, Pathanamthitta, India. arjunjith@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jayaprakash A, Pappen TT, Sebastian R, Kunjukunju BP, Joseph A, Mathew L. Asymptomatic skin lesions as a diagnostic clue in multiple myeloma – A case report. J Skin Sex Transm Dis 2024:6:50-3. doi: 10.25259/JSSTD_3_2024
Abstract
Multiple myeloma (MM) is a rare cancer of plasma cells in the bone marrow. Cutaneous plasmacytoma is an uncommon but specific skin lesion in MM with an incidence of 2%. Cutaneous plasma cell infiltration in pre-existing MM is a very rare phenomenon, with approximately 100 cases described in the literature. Here, we report a case of a 61-year-old male who presented with asymptomatic skin nodules and plaques over the chest, abdomen, and back of the trunk for five months. Histopathological examination showed mononuclear cells with moderate cytoplasm and round to ovoid nuclei. Immunohistochemistry showed CD138 and kappa positivity and lambda and CD20 negativity, confirming the diagnosis of cutaneous plasmacytoma. Bone marrow biopsy and immunohistochemistry revealed bone marrow plasmacytosis with kappa light chain restriction. Serum free light chain ratio was 106.61 and fluorescence in situ hybridization showed del 13q. The clinical features and investigations fulfilled the diagnostic criteria for MM, and the patient was started on chemotherapy, following which the skin lesions improved. Development of skin lesions is seen in the advanced stages of MM and is considered a bad prognostic sign. However, they can also be seen as initial manifestations of the disease, as in this case. Hence, meticulous investigations and early diagnosis are of paramount importance.
Keywords
Asymptomatic skin nodules
Cutaneous plasmacytoma
Multiple myeloma
INTRODUCTION
Multiple myeloma (MM) is a hematologic malignancy characterized by the presence of abnormal clonal plasma cells in the bone marrow, with the potential for uncontrolled growth, causing destructive bone lesions, kidney injury, anemia, and hypercalcemia.[1] The disease is often confined to the bone and bone marrow, but other organ also can be involved. MM occurring in organs besides the bone or the bone marrow is called the extramedullary plasmacytoma.[2] Cutaneous plasmacytoplasma can occur from hematogenous spread or infiltration of plasma cells from adjacent structures such as bones. It usually occurs in patients with aggressive or highly progressive forms of MM.[2] Cutaneous plasma cell infiltration in pre-existing MM is a very rare phenomenon, with approximately 100 cases described in the literature.[3]
Here, we present a patient who presented to our outpatient department with asymptomatic plaques and nodules, which were found to be cutaneous plasmacytoma and, on further evaluation, revealed underlying MM.
CASE REPORT
A 61-year-old gentleman, who is a farmer by profession and with no known comorbidities, presented to our outpatient department with complaints of multiple asymptomatic reddish and skin-colored raised lesions over the chest, abdomen, and back of trunk for five months. The lesions were gradually increasing in size and number.
General and system examinations were normal. Dermatological examination showed multiple discrete erythematous and skin-colored plaques and nodules with sizes ranging from 1 cm to 2.5 cm in greatest dimensions, smooth surface, and firm consistency over the chest abdomen and back of trunk [Figures 1 and 2].

- Erythematous plaques and nodules over chest and abdomen.

- Erythematous and skin colored plaques and nodules over the back of the trunk.
From the history and examinations, differential diagnoses of histiocytoma, pseudolymphoma, B cell lymphoma, sarcoidosis, and metastatic nodules were considered.
His hemoglobin was 13.8 g/dL, total leukocytes count 4.7 × 109/L, platelet count: 132,000/micro L, liver function tests were within normal limits, urea: 13.3 mmoL/L, creatinine: 0.9 mg/DL, creatinine clearance: 88.9 mL/min/BSA, serum calcium: 9.6 mg/dL, and chest X-ray and electrocardiography were normal.
Section from the skin showed a dense mononuclear cell infiltrate arranged in sheets in the dermis and surrounding appendages. The mononuclear cells had moderate cytoplasm and round to ovoid nuclei, with some showing prominent nucleoli. The overlying epidermis is orthokeratotic and intact [Figure 3].
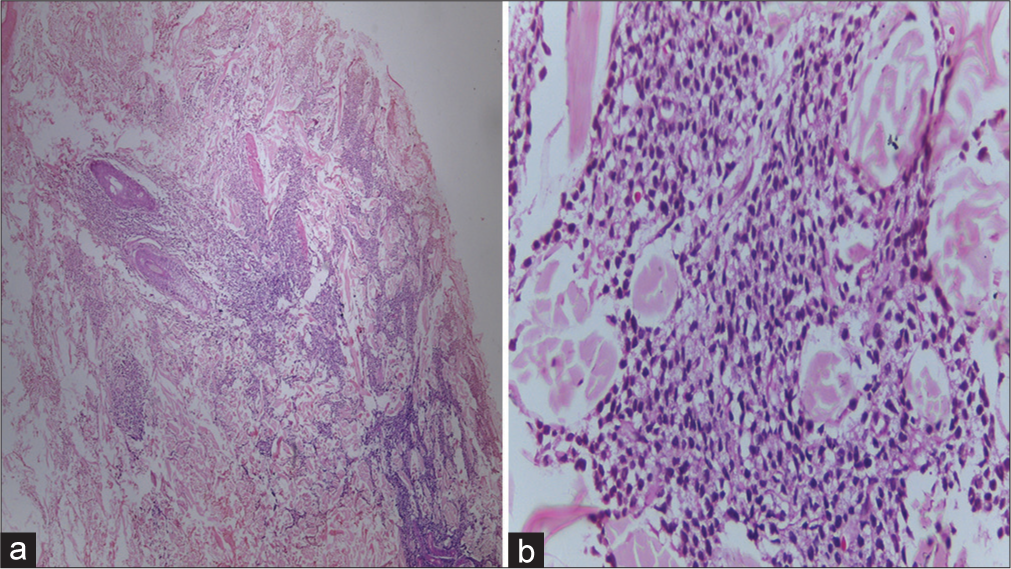
- (a): Section from skin shows a dense mononuclear cell infiltrate in the dermis arranged in sheets and surrounding the appendages (H&E ×100); (b): Mononuclear cells have moderate cytoplasm and round to oval nuclei, with some showing prominent nucleoli (H&E ×400).
Immunohistochemistry demonstrated CD138 and Kappa Positivity. There were scattered CD 45 cells. Markers for Lambda, CD20, CD34, CD68, CD117, CD1a, Tdt, CK, CD3, and CD5 were negative, Ki67 was 36%, favoring the diagnosis of cutaneous plasmacytoma [Figure 4].
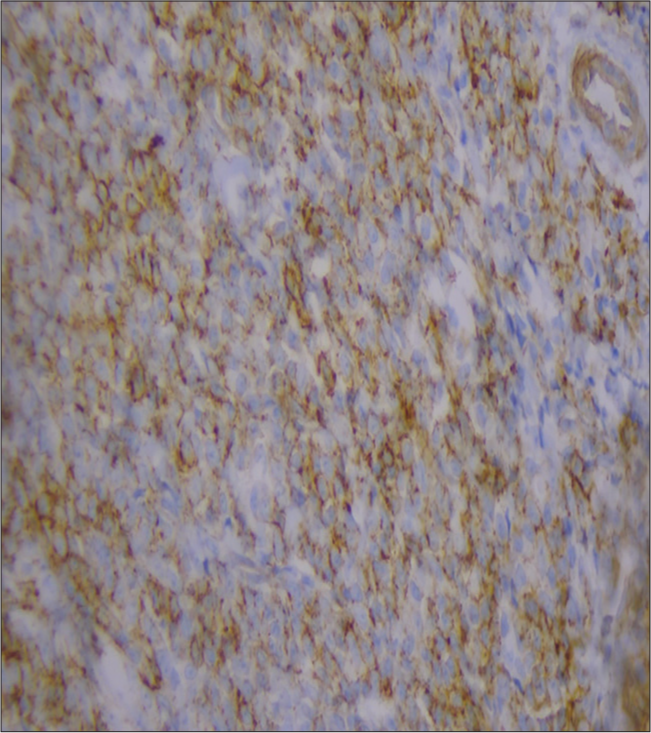
- Immunohistochemistry showing CD138 positivity.
The patient was referred to oncology for further evaluation, and the serum protein capillary electrophoresis showed hypogamma globulinemia with normal total protein. M spike was not seen.
Bone marrow biopsy showed cellular marrow with normal trilineage hematopoiesis and a mild increase in plasma cells (18% plasma cells). Immunohistochemistry showed CD138 positivity with a cluster of 8–10 plasma cells overall forming around 30% cellularity, kappa positivity, and lambda negativity, suggestive of bone marrow plasmacytosis with kappa light chain restriction.
Positron emission tomography and computed tomography was normal except for cutaneous soft-tissue density lesions in the chest and abdominal wall (corresponding to the skin lesions).
There was no elevation of calcium, renal insufficiency, anemia or bone anomalities.
Serum free light chain ratio was 106.61.
Fluorescence in situ hybridization showed del 13q positive.
These investigations confirmed the diagnosis of MM with extramedullary plasmacytomas.
The patient was started on cyclophosphamide, bortezomib, and dexamethasone (CyBorD) chemotherapy, and skin lesions disappeared after four weeks of chemotherapy.
DISCUSSION
MM is a clonal proliferation of malignant plasma cells producing monoclonal immunoglobulin. The most common clinical manifestations of MM, (which indicate organ damage, are known as the CRAB features, an acronym which includes elevated serum calcium, renal function impairment, anemia, and/or bone involvement),[4] were absent in this case.
The International Myeloma Working Group (IMWG) definition of active MM is clonal bone marrow plasma cells >10% or biopsy-proven bony or extramedullary plasmacytoma (both were present in this case) and any one or more of the CRAB features (mentioned above) or one or more of the following myeloma defining events (MDEs), which are biomarkers of malignancy that is (1) 60% or greater clonal plasma cells on bone marrow examination, (2) serum involved/uninvolved free light chain ratio of 100 or greater, provided the absolute level of the involved light chain is at least 100 mg/L (Which was satisfied in our case. [805/7.56= 106.61]), and (3) more than one focal lesion on magnetic resonance imaging that is at least 5 mm or greater in size.[5]
Three classes of drugs that are approved for newly diagnosed MM are immunomodulatory agents, proteasome inhibitors, and targeted antibodies. A combination of bortezomib, cyclophosphamide, and dexamethasone achieves more than 90% response rate.[6]
Cutaneous plasmacytoma is a monoclonal proliferation of plasma cells. It can be primary (with no other concomitant bony or extramedullary disease) or secondary (associated with MM, extramedullary plasmacytoma or plasma cell leukemia.[7] They present with firm violaceous papules and nodules over the trunk, scalp, and face. Histopathology shows diffuse or nodular aggregates of lymphoplasmacytic cells, which are CD138 and CD79a positive. Cutaneous plasmacytoma is an uncommon but specific skin lesion in MM with an incidence of 2%.[3] They result from the lymphatic, hematological, or metastatic spread. They are more commonly seen in advanced stages of the disease and are considered a bad prognostic sign. However, they can also be seen as the initial manifestation of the disease, as in this case, where the asymptomatic skin lesions were the only clinical presentation.
CONCLUSION
Skin lesions can sometimes be the only initial presentation of a rare and fatal internal malignancy. A high index of suspicion, proper evaluation, and timely diagnosis can help in the early detection and treatment of such cases.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Diagnosis and management of multiple myeloma: A review. JAMA. 2022;327:464-77.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous plasmacytoma: Metastasis of multiple myeloma at the fracture site. Ann Dermatol. 2017;29:483-6.
- [CrossRef] [PubMed] [Google Scholar]
- The skin disorders of the haematopoetic and immune systems; Malignant infiltration of the skin in plasma cell disorders In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook's textbook of dermatology (9th ed). Oxford: Wiley-Black; 2016.
- [Google Scholar]
- An unusual presentation of multiple myeloma. BMJ Case Rep. 2018;11:e226412.
- [CrossRef] [PubMed] [Google Scholar]
- Updated diagnostic criteria and staging system for multiple myeloma. Am Soc Clin Oncol Educ Book. 2016;35:418-23.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell disorders;Multiple myeloma In: Loscalzo J, Kasper DL, Longo DL, Fauci AS, Hauser SL, Jameson JL, eds. Harrison's principles of internal medicine (21st ed). United States of America: Mc Graw Hill; 2022.
- [Google Scholar]
- Cutaneous nodules as a diagnostic clue in multiple myeloma. Am J Dermatopathol. 2013;35:377-80.
- [CrossRef] [PubMed] [Google Scholar]






