Translate this page into:
Diabetic dermopathy (shin spots) and diabetic retinopathy – Are they associated?
*Corresponding author: Joan Felicita Samson, Department of Dermatology, Dr. Somervell Memorial CSI Medical College and Hospital, Karakonam, Trivandrum -695504, Kerala, India. dr.joanfs@gmail.com
-
Received: ,
Accepted: ,
Abstract
Objectives:
Shin spots and diabetic retinopathy are considered as manifestations of diabetic microangiopathy. However, there are only a few studies about this possible association. We undertook this study to confirm a possible association between shin spots and diabetic retinopathy.
Materials and Methods:
A total of 137 patients between the ages of 40 and 70 years having diabetes mellitus of at least 5 years duration were included in the study. These patients were examined for skin and retinal changes. The study period was 6 months.
Results:
Of the 137 diabetic patients included in this study, 123 (89.8%) had shin spots. The mean age of diabetic patients with shin spots was 59.6 years. Diabetic retinopathy was seen in 83 cases (60.6%), of which 79 (95.2%) had shin spots. The mean duration of diabetes mellitus in patients with shin spots was 12.7 years and it was 8.1 years in those without shin spots. The mean duration of diabetes mellitus in patients with diabetic retinopathy was 13.6 years and it was 9.9 years in those without diabetic retinopathy. On doing regression analysis, it was found that it is the duration of diabetes that was associated with shin spots.
Limitations:
Small sample size was the limitation.
Conclusion:
Duration of diabetes mellitus is associated with the presence of dermopathy.
Keywords
Diabetic dermopathy
Shin spots
Diabetic retinopathy
INTRODUCTION
Diabetes mellitus is a metabolic disorder characterized by hyperglycemia and frequent changes in the metabolism of fats and proteins. It is the most common endocrine disorder, affecting approximately 4% of the world population.[1] India has a high prevalence of diabetes mellitus and the incidence is increasing at an alarming rate. In India alone, diabetes has increased from 40.6 million in 2006 and is expected to reach 79.4 million by 2030.[2]
Chronic hyperglycemia leads to changes in microcirculation and glycosylation of proteins, and these result in lesions that are more evident in the kidneys, retina, nerves, and skin.[3] These changes manifest as renal failure, retinopathy, peripheral, and autonomic neuropathy as well as diabetic dermopathy.[4]
Diabetic dermopathy is the most common skin condition that occurs in patients with diabetes mellitus. This was first reported by Melin in 1964, as small, circumscribed, brownish atrophic skin lesions occurring on the lower extremities.[5] The term “diabetic dermopathy” was coined by Binkley in 1965;[6] other names used are “pigmented pretibial patches,”[7] “shin spots,”[8] “spotted leg syndrome,”[9] and “diabetic dermangiopathy.”[10] A minimum number of four shin spots is characteristic of diabetes.[11]
Many studies have examined the association between dermopathy, retinopathy, neuropathy, and nephropathy in diabetes patients. Some studies have reported an association while others did not find a statistically significant association.[12-17]
The purpose of this study was to investigate (i) the association of shin spots and diabetic retinopathy and (ii) to investigate diabetic dermopathy-associated demographic characteristics.
MATERIALS AND METHODS
It is a cross-sectional study of 137 patients having diabetes mellitus of at least 5 years duration, aged between 40 and 70 years, attending the departments of dermatology and ophthalmology in a tertiary center of Kerala, for a period of 6 months, September 2017–February 2018. Patients suffering from other skin diseases such as psoriasis and lichen planus that may affect the cutaneous findings and from ophthalmological conditions such as hypertensive retinopathy, vascular occlusion, and advanced cataract that may affect the findings were excluded from the study.
A semi-structured questionnaire was used to collect the data. The dermatological examination was done by a dermatologist under proper day light and using hand lens, when needed. Examination of the retina was done by an ophthalmologist using indirect ophthalmoscopy of dilated fundus and fundus fluorescein angiography.
The sociodemographic details included were name, age, sex, educational status and occupation, duration of diabetes, medications, and associated conditions.
The collected data were entered into MS Excel software and were analyzed using SPSS version 16. Institutional ethics committee approved the study. Individual study participant gave written informed consent.
RESULTS
A total of 137 patients were recruited for the study. The age ranged from 42 years to 70 years. The mean age was 59.4 (standard deviation 6.98 years) years. The duration of diabetes mellitus in this group was 5–40 years with a mean duration of 12.3 years (standard deviation 6 years).
There were 56 males (40.9%) and 81 females (59.1%).
Out of the 137 patients, 127 had a minimum of primary education. Majority of females (69, 85.2%) were housewives.
Fifty-five patients (40.1%) were on oral hypoglycemic agents, 30 patients (21.9%) on insulin, and 52 (38%) were on both insulin and tablets. One patient though aware of diabetes was not taking any medication.
Seventy-two females (88.9%) had shin spots and 51 males (91.1%) had shin spots. P = 0.68 proving that there is no association between gender and the occurrence of shin spots [Figures 1 and 2].

- Shin spots.

- Another patient manifesting shin spots.
The mean age of patients with shin spots was 59.6 years (standard deviation 6.6 years) and without shin spots was 57.2 years (SD 9.94 years). This was also statistically not significant.
Of the 137 diabetic patients included in this study, 123 (89.8%) had shin spots. Diabetic retinopathy was seen in 83 cases (60.6%) of the study group [Figure 3].

- Fundus finding: Severe non-proliferative diabetic retinopathy with clinically significant macular edema.
Of the 83 diabetic retinopathy patients, 79 (95.2%) had shin spots, but 44 (81.5%) out of the 54 patients without diabetic retinopathy also had shin spots. This difference was statistically significant (P = 0.01). While doing logistic regression with duration of diabetes mellitus and diabetic retinopathy as covariates; and shin spots as dependent variable, it was found that it is only the duration of diabetes mellitus that is associated with shin spots. Adjusted odds ratio for the duration of diabetes is 1.2 (95% CI 1.009–1.449; P = 0.039%).
The mean duration of diabetes mellitus in patients with shin spots was 12.7 years (SD 5.9 years) and median was 12 years. Mean duration was 8.1 years (standard deviation 4.9 years) and median was 6.5 years, in those without shin spots.
This difference was statistically significant; t-test was done and P value was found to be 0.007 [Figure 4].*
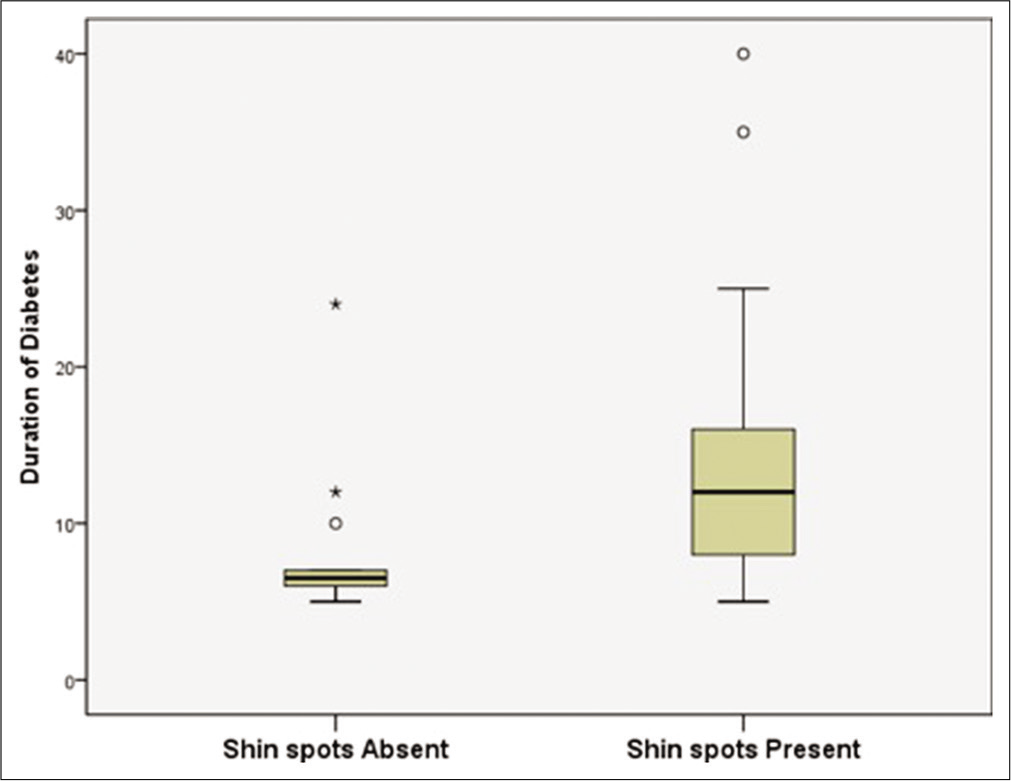
- Box plot showing distribution of duration of diabetes among patients with and without shin spots.
Similarly, the mean duration of diabetes mellitus in patients with diabetic retinopathy was 13.8 years (standard deviation 5.5 years) with a median of 13 years while it was 9.9 years (standard deviation 5.98 years) with a median of 8 years in patients without diabetic retinopathy. This difference was also statistically significant; t-test was done and P value was found to be <0.001.
It was observed that diabetic dermopathy was seen earlier (12.7 years) than diabetic retinopathy (13.8 years) during the course of diabetes mellitus [Figure 5].

- Box plot showing distribution of duration of diabetes among patients with and without retinopathy.
By doing ROC curve analysis [Figure 6], it was found that more than 7 years duration of diabetes can be considered as an indicator of shin spots with 79.5% sensitivity (71.3–86.3%) and 73.3% specificity (44.9–92.2%).

- ROC curve showing duration of diabetes and shin spots.
The ROC curve analysis showed that diabetes mellitus of more than 12 years duration can be an indicator of diabetic retinopathy with 54.2% sensitivity (42.9%-65.2%) and 83.3% specificity (70.7%-92.1%). A screening of diabetic retinopathy for all diabetic patients above 5 years duration will be able to pick up retinopathy with 96.4% (89.8–99.2%) sensitivity but with a very poor specificity of 13% (5.42–24.9%); this 5 years, as the best cutoffs were selected by Youden’s index.**
We concluded that diabetic dermopathy in patients with more than 12 years duration of diabetes was associated with retinopathy with a specificity of 83.3% (70.7–92.1%) and sensitivity of 54.2% (42.9–65.2%). Whereas the Youden’s index showed a sensitivity of 96.4% (89.8–99.2%) but a poor specificity of 13% (5.42–24.9%) when the duration of diabetes was 5 years.
Hypertension was present with diabetes mellitus in 76 (55.5%) patients of this study population. No association of hypertension with shin spots was found in these cases (Chi-square 0.189; df-1; P = 0.664).
The other cutaneous findings were ichthyosis in 34 cases (24.8%), xerosis (without ichthyosis) in 47 patients (34.3%), and chronic paronychia in 7 patients (4.9%). Five cases (3.5%) had candida intertrigo. Tinea versicolor was present in 6 cases (4.4%), tinea corporis in a single person (0.7%), and tinea unguium in 6 cases (4.4%). Twenty-seven patients (19.4%) had idiopathic guttate hypomelanosis. Surprisingly, a very low incidence of fissure feet 2 (1.5%), pyoderma 1 (0.7%), and eczema 4 (2.9%) was seen.
DISCUSSION
In the current study, a total of 137 patients were recruited, all of them suffered from type 2 diabetes mellitus for at least 5 years. They were screened for the presence of shin spots (diabetic dermopathy) by a dermatologist and diabetic retinopathy by an ophthalmologist. There are only a few reports about this subject in the literature.
Seventy-two females out of 81 (88.9%) had shin spots and 51 out of 56 males (91.1%) had shin spots. No association between gender and the occurrence of shin spots was found in this study. A few other studies also showed similar findings, some others showed an increased occurrence in males.[5,14,17] The mean age of those with shin spots in the present study was 59.6 years (standard deviation 6.6 years) and without shin spots was 57.2 years (SD 9.94), but this was not statistically significant. In other studies also, diabetic dermopathy has been reported most prevalent in the age group of 45–70 years; but as against our finding, they found a significant association with age.[12,17-20]
In this study, 89.8% had shin spots; diabetic retinopathy was seen in 60.6%. Of the 83 diabetic retinopathy patients, 95.2% had shin spots. On doing logistic regression with duration of diabetes mellitus and diabetic retinopathy as covariates; and shin spots as dependent variable, it was found that it is the duration of diabetes mellitus that is associated with shin spots and not diabetic retinopathy. This is in accordance with similar earlier studies which also agreed on the fact that the dermopathy lesions were significantly associated with the duration of illness.[14,18,13,21] A few studies showed a statistically significant association of diabetic dermopathy with diabetic retinopathy also. However, this association could not be demonstrated in our study.[17,18,22]
Limitations
Small sample size was the limitation.
CONCLUSION
Our study clearly shows that diabetic retinopathy and dermopathy are not associated with each other, but both are independently associated with the duration of diabetes mellitus, that is, longer the duration of diabetes mellitus, there is a greater chance of having diabetic dermopathy and retinopathy. It was observed that diabetic dermopathy was seen earlier than diabetic retinopathy during the course of diabetes mellitus.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Joan Felicita Samson is on the Editorial Board of the Journal.
References
- Global burden of diabetes 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414-31.
- [CrossRef] [Google Scholar]
- Rising prevalence of NIDDM in an urban population in India. Diabetologia. 1997;40:232-7.
- [CrossRef] [Google Scholar]
- Diabetes mellitus and hypoglycemia In: McPhee SJ, Papadakis MA, eds. Current Medical Diagnosis and Treatment (46th ed). New York: McGraw-Hill; 2007. p. :1219-65.
- [Google Scholar]
- An atrophic circumscribed skin lesion in the lower extremities of diabetics. Acta Med Scand. 1964;176(Suppl 423):1-75.
- [Google Scholar]
- Pigmented pretibial patches. A cutaneous manifestation of diabetes mellitus. Arch Dermatol. 1966;93:282-6.
- [CrossRef] [Google Scholar]
- Skin lesions in diabetic patients: The spotted-leg syndrome. Lahey Clin Found Bull. 1965;14:10-4.
- [Google Scholar]
- Diabetic dermangiopathy. A spectrum including pigmented pretibial patches and necrobiosis lipoidica diabeticorum. Br J Dermatol. 1970;83:528-35.
- [CrossRef] [Google Scholar]
- Manifestations of cutaneous diabetic microangiopathy. Am J Clin Dermatol. 2005;6:225-37.
- [CrossRef] [Google Scholar]
- Skin health and metabolic complications. In: Watson R, Zibadi S, eds. Bioactive Dietary Factors and Plant Extracts in Dermatology. Nutrition and Health. Totowa, New Jersey: Humana Press; 2013.
- [CrossRef] [Google Scholar]
- Association of HbA1c levels with vascular complications and death in patients with Type 2 diabetes: Evidence of glycaemic thresholds. Diabetologia. 2012;55:636-43.
- [CrossRef] [Google Scholar]
- Diabetic dermopathy and internal complications in diabetes mellitus. Int J Dermatol. 1998;37:113-5.
- [CrossRef] [Google Scholar]
- Relationship between skin diseases and extracutaneous complications of diabetes mellitus: Clinical analysis of 750 patients. Am J Clin Dermatol. 2014;15:65-70.
- [CrossRef] [Google Scholar]
- The correlation between skin lesions, microalbuminuria and other microvascular complications in Type 2 diabetic patients. Nephrourol Mon. 2010;2:553-60.
- [Google Scholar]
- Dermopathy and retinopathy in diabetes: Is there an association? Dermatology. 2007;214:133-6.
- [CrossRef] [Google Scholar]
- A study on the association of diabetic dermopathy with nephropathy and retinopathy in patients with Type 2 diabetes mellitus. J Nephropathol. 2016;5:139-43.
- [CrossRef] [Google Scholar]
- An observational study of cutaneous manifestations in diabetes mellitus in a tertiary care hospital of Eastern India. Indian J Endocrinol Metab. 2014;18:217-20.
- [CrossRef] [Google Scholar]
- Skin blood flow abnormalities in diabetic dermopathy. J Am Acad Dermatol. 2011;65:559-63.
- [CrossRef] [Google Scholar]






