Translate this page into:
Effect of apremilast on cardiovascular risk in psoriasis patients in comparison with methotrexate
*Corresponding author: Dr. Sebastian Criton, Department of Dermatology, Amala Institute of Medical Sciences, Thrissur, Kerala, India. criton@thecriton.com
-
Received: ,
Accepted: ,
How to cite this article: Varghese A, Sebastian Criton VJ, George R. Effect of apremilast in cardiovascular risk in psoriasis patients in comparison with methotrexate. J Skin Sex Transm Dis 2024:6:31-6. doi: 10.25259/JSSTD_47_2023
Abstract
Objectives:
To compare the change in cardiovascular risk factors who are taking apremilast and methotrexate.
Materials and Methods:
This hospital-based prospective cohort study included 40 newly diagnosed cases of psoriasis who were divided into two groups – group A (receiving methotrexate) and group B (receiving apremilast) and were assessed at baseline and after 12 weeks. The outcome was assessed on the basis of psoriasis area and severity index score and the biochemical parameters.
Results:
A total of 50 patients diagnosed with chronic plaque psoriasis were enrolled in the study, out of which 40 completed the study. At the end of 12 weeks, patients treated with apremilast showed a 49.39% reduction in mean PASI score, while those on methotrexate showed a 46.19% reduction. Significant elevation of alanine transaminase was seen only in the methotrexate group with P < 0.05. No significant change was observed in blood glucose levels in both groups. hs-CRP levels in the methotrexate group showed a significant decrease as compared to apremilast (P < 0.05).
Limitations:
Absence of blinding, psoriasis patients not stratified according to severity, and a small sample size were the major limitations.
Conclusion:
On comparing the two drugs, methotrexate is considered to have more cardioprotective action.
Keywords
Apremilast
Methotrexate
Psoriasis
INTRODUCTION
Psoriasis is a chronically relapsing inflammatory disorder with cutaneous and rheumatologic manifestations characterized by increased cardiovascular diseases. Chronic inflammation in psoriatic patients predisposes them to diseases with inflammatory components, mostly cardiovascular morbidity. This study was done to compare the change in cardiovascular risk factors who are taking apremilast and methotrexate.
Several meta-analyses[1,2] showed that the spectrum of inflammation is systemic with an elevation of interleukin (IL)-6, tumor necrosis factor (TNF)-alpha, C-reactive protein (CRP), E-selectin, and intercellular adhesion molecule-1 which are predictors of cardiovascular mortality.[3]
CRP, an acute-phase protein, is an emerging marker of cardiovascular inflammation leading to atherosclerosis. It has been shown that high-sensitivity CRP (hs-CRP) predicts cardiovascular risk when traditional risk factors are normal.[4,5]
Studies have shown that hs-CRP did not correlate with cardiovascular risk and was found to be an independent predictor of recurrent cardiovascular events in the Asian population.[6,7] Another study from South India showed that CRP is a sensitive risk factor for cardiovascular disease in psoriasis patients.[8]
ThromboxaneA2 produced by activated platelets is unstable and hydrolyzed within about 30 s to the inactive thromboxaneB2, which is completely excreted by the urine. Hence, thromboxane B2 urinary assay is a non-invasive test to measure platelet activation. It has been shown that urinary thromboxane B2 measurement is a useful indicator of major adverse cardiovascular events.
Apremilast is a Food and Drug Administration-approved medication for the treatment of moderate to severe psoriasis and psoriatic arthritis. It selectively inhibits phosphodiesterase (PDE)-4, which reduces inflammation, leading to a reduction of TNF-alpha, IL-23, and an increase of IL-10.[9]
A large number of epidemiological studies performed in various countries have demonstrated that psoriasis is associated with an increased prevalence of cardiovascular diseases. However, there is a gap in understanding the effect of methotrexate and apremilast on cardiovascular risk, and hence, more studies are needed to establish such a link.[10]
Aims and objectives
The aims of this study were as follows:
To evaluate the effect on biochemical parameters pertaining to cardiovascular risk in psoriasis patients after 12 weeks of treatment with apremilast in comparison with methotrexate
To compare the efficacy of methotrexate with apremilast in treating chronic plaque psoriasis.
MATERIAL AND METHODS
This is a prospective cohort study conducted in a tertiary care center after getting clearance from the Ethical Committee. All consecutive new patients who attended the dermatology department with chronic plaque psoriasis diagnosed clinically in the period between February 1, 2021, and August 1, 2021, were enrolled in the study. The participant will be informed about the study, and written consent was obtained. A total of 50 patients were enrolled in the study. Sample size calculation was done by independent t-test.
The sample size was calculated by independent t-test.
Based on the mean and standard deviation of psoriasis area and severity index (PASI) score observed in an earlier publication[11] with a 95% confidence level and 90% power minimum sample size comes to 20 in each group, expecting 20% loss for follow-up, we have taken 25 in each group. Since we got only 25 in each group, our sample size was 50.
The patients who received antipsoriatic treatment with methotrexate and apremilast were followed up.
Group A-Oral methotrexate 7.5 mg once per week was given.
Group B-A starter pack of apremilast was given in the following regime: Days 1–4: 10 mg once daily; Days 5–8: 20 mg once daily; and Day 9 onward: 30 mg daily.
Clinical (PASI score) and biochemical (Fasting blood glucose, lipid profile blood counts, liver enzymes, high-sensitivity C-reactive protein [hsCRP], and urinary thromboxane B2) assessments were done at baseline and after 12 weeks, and the results were compared between two groups.
The data were analyzed by the Statistical Package for the Social Sciences version 25. The chi-square test was used to describe a statistically significant correlation with the severity of skin involvement. An Independent t-test was used to analyze the cardiovascular risk improvement with treatments. P < 0.05 was considered significant.
Inclusion criteria
The following criteria were included in the study:
Patients with chronic plaque psoriasis
Patients above 18-years.
Exclusion criteria
Pregnant and lactating patients, those with a history of cardiovascular diseases, on aspirin, statins, and other cardiovascular drugs were excluded from the study.
RESULTS
A total of 50 patients diagnosed with chronic plaque psoriasis were enrolled in the study, out of which 40 completed the study [Figure 1]. Patients who received methotrexate and apremilast were followed up. (In the methotrexate group, five patients were lost to follow-up due to unknown reasons during the 1st month itself, four in the apremilast group stopped the drug due to abdominal pain, and one in the apremilast group had the serious adverse effect – an episode of myocardial infarction after 1 month of treatment). The baseline data are given in Table 1. Figure 1 shows a flowchart representation of the study.
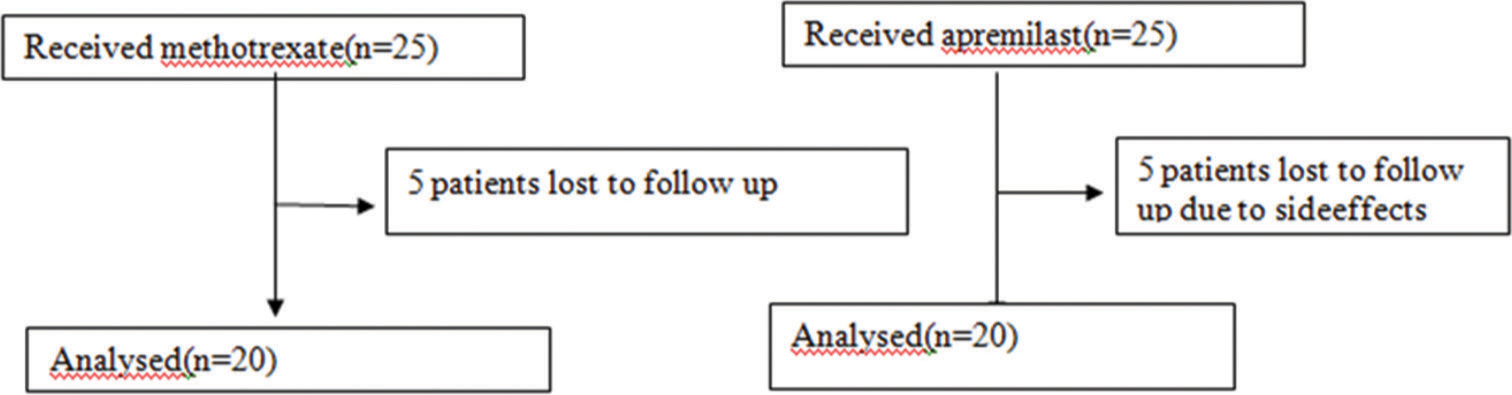
- Schematic figure showing the number patients included in the study and followed up.
| Apremilast | Methotrexate | P-value | |
|---|---|---|---|
| Age in years* | 44.4±15.4 | 43.4±11.1 | 0.815 |
| Male: Female ratio | 14:6 | 15:5 | 0.723 |
| Duration in years* | 4.2±2.4 | 6.8±3.9 | 0.016 |
| PASI baseline | 13.26±2.6 | 16.05±4.5 | 0.001 |
| PASI at 12 weeks | 6.71±2.8 | 8.6375±4.2 | 0.001 |
PASI score
At the end of 12 weeks, patients treated with apremilast showed a 49.39% reduction in mean PASI score, while those on methotrexate showed a 46.19% reduction. The change in PASI score did not differ significantly between the two groups [Table 2].
| Independent sample t-test | ||||
|---|---|---|---|---|
| Group | Mean | Std. Deviation | t-statistic | P-value |
| Difference in FBS | ||||
| Apremilast | −3.75 | 30.91223 | −1.616 | 0.114 |
| methotrexate | 11 | 26.67149 | ||
| Difference in cholesterol level | ||||
| Apremilast | −2.9 | 31.85312 | −1.68 | 0.101 |
| methotrexate | 13.95 | 31.5836 | ||
| Difference in triglyceride | ||||
| Apremilast | 6.25 | 26.0038 | −1.958 | 0.058 |
| methotrexate | 22.6 | 26.8022 | ||
| Difference in HDL | ||||
| Apremilast | 3.9 | 5.27057 | 1.22 | 0.23 |
| methotrexate | 1.45 | 7.2727 | ||
| Difference in LDL | ||||
| Apremilast | 4.2815 | 16.9475 | −2.35 | 0.024* |
| methotrexate | 15.98 | 14.43109 | ||
| Difference in hsCRP | ||||
| Apremilast | 0.3396 | 2.57683 | −2.31 | 0.026* |
| methotrexate | 1.774 | 1.03514 | ||
| Difference in PASI | ||||
| apremilast | 6.5515 | 3.20077 | −0.893 | 0.378 |
| methotrexate | 7.4155 | 2.9128 | ||
| Difference in neutrophil | ||||
| apremilast | 1.115 | 7.51204 | −0.865 | 0.392 |
| methotrexate | 3.15 | 7.36475 | ||
| Difference in platelet | ||||
| apremilast | −9630 | 90318.6004 | −1.569 | 0.125 |
| methotrexate | 26985 | 52285.99767 | ||
| Difference in Hb level | ||||
| apremilast | −0.115 | 1.46225 | −0.699 | 0.489 |
| methotrexate | 0.175 | 1.14012 | ||
| Difference in WBC | ||||
| apremilast | −94 | 1329.36629 | −1.946 | 0.059 |
| methotrexate | 659 | 1108.07514 | ||
| Difference in ALT | ||||
| apremilast | −0.905 | 7.43048 | 3.51 | 0.001* |
| methotrexate | −15.95 | 17.67089 | ||
| Difference in AST | ||||
| apremilast | 2.195 | 7.49544 | 2.36 | 0.024* |
| methotrexate | −6.55 | 14.78077 | ||
| Difference in lymph | ||||
| apremilast | −0.31 | 8.42277 | −1.371 | 0.178 |
| methotrexate | 2.65 | 4.71587 | ||
Lipid profile
There was a statistically significant reduction in serum triglycerides and low-density lipoprotein (LDL) cholesterol in the methotrexate group and a reduction of high-density lipoprotein (HDL) in the apremilast group with P < 0.05 [Table 2].
Blood counts
There were no significant reductions in cell counts with both methotrexate and apremilast [Table 2].
Liver enzymes
Among liver enzymes, significant elevation of alanine transaminase was seen only in the methotrexate group with P < 0.05 [Table 2].
Fasting blood sugar (FBS)
No significant change was observed in blood glucose levels in both groups [Table 2].
hsCRP
hs-CRP levels in the methotrexate group showed a significant decrease as compared to apremilast with P < 0.05 [Table 2].
Thromboxane B2
Only five patients had raised levels of thromboxane b2 levels among 20 patients, and four of these five patients showed decreased levels after 3 months of treatment with methotrexate. Apremilast decreased the thromboxane b2 level of one patient.
DISCUSSION
Psoriasis and cardiovascular disease share similar pathogenic mechanisms, such as vascular endothelial cell dysfunction, oxidative stress, and metabolic syndrome.[12] The mean per cent reduction of PASI score after 12 weeks of treatment was found to be 49.39% for methotrexate and for apremilast 46.19% compared with baseline. Similar studies comparing the relative efficacy of methotrexate and apremilast in chronic plaque psoriasis and psoriatic arthritis found no significant difference in PASI scores between the two groups.[13,14] Similarly, another study comparing the efficacy of both drugs in palmoplantar psoriasis showed that apremilast had a comparable efficacy and safety profile to methotrexate in the management of palmoplantar psoriasis.[15]
In our study, we observed an insignificant rise in the level of total cholesterol (TC) and a modest reduction in triglyceride and LDL after 3 months of treatment with apremilast. However, the level of HDL showed a significant fall. These changes appear contradictory to the previously noted beneficial effect of PDE inhibition on lipid profile. Gualtierotti and De Lucia observed a reduction in TC, TC/HDL ratio after 1 month of treatment with apremilast with further reduction in TC (5%), LDL (25%), and triglyceride (17%) and a 20% increase in HDL after 12 months of treatment.[16]
Gisondi et al. showed no significant difference in triglyceride mean levels in psoriasis patients taking methotrexate.[12] Dehpourietal reported a non-significant increase in TC and LDL with a significant increase in HDL in psoriatic arthritis patients receiving methotrexate.[17] In contrast to all this, we observed a significant decrease in LDL triglyceride and a non-significant decrease in TC and HDL in those taking methotrexate.
We also analyzed the level of urinary thromboxane b2. Still, we observed elevated thromboxane b2 only in five patients, of which four received methotrexate. All of them showed decreased levels after 12 weeks of treatment, and only one received apremilast showed decreased levels after 12 weeks of treatment. Since increased thromboxane levels are associated with vascular inflammation and, hence, adverse cardiovascular outcomes, methotrexate can be considered as cardioprotective.
We observed negligible changes in blood counts. Kolios et al. reported lymphopenia following apremilast treatment for 3 months.[18] Studies among animal models showed negligible lymphopenia and neutropenia.
There was no significant change in the level of transaminase in patients treated with apremilast, as observed in our study. This was in accordance with a large scale randomized, controlled trial of apremilast in psoriatic patients where serum enzyme elevation was not different from the placebo group. Salliot and van der Heijde, in 2009, showed that elevated transaminase levels were found in 20% of patients treated with 5 mg methotrexate for 1 year, with levels more than twice the upper limit in 13%.[19] This is in accordance with our findings.
In contrast to previously reported studies where PDE inhibitors exert a beneficial glycemic effect through glucagon-like peptide release, we did not observe any significant change; on the contrary, an insignificant increase in FBS levels was noted among 11 out of 20 patients in the apremilast group. This discrepancy may be due to inherent differences between study populations.
Gisondi et al. surveyed psoriasis patients who were newly treated with methotrexate and demonstrated that there was no detected change in FBS levels.[12] Cuchacovich and Espinoza examined 37 patients with rheumatoid arthritis treated with methotrexate for 24 months and found no significant change in FBS.[20] Our study population showed an insignificant decrease in FBS levels after 3 months of treatment with methotrexate.
Since one of the risk factors in cardiovascular risk is systemic inflammation, hsCRP can be used as a tool to identify people at risk.
There was an insignificant decrease in hs-CRP levels following 3 months of apremilast treatment in our study population. In a study by Danese et al., apremilast was shown to decrease levels of CRP in ulcerative colitis patients after 12 weeks of treatment.[21]
The previous studies reported decreased hs-CRP after methotrexate treatment for psoriasis.[22] Similar to other investigators, we observed a significant decrease after 3 months of therapy.
Methotrexate’s traditional role as a first-line agent for moderate to severe psoriasis is being challenged by the rapid and growing use of biological therapies.
Although many studies point out its unpredictable response and toxicity, it remains admirable in regions with limited resources even after the introduction of newer and more effective biological treatments. It may also, through its antiproliferative, immunosuppressive, and anti-inflammatory effects, improve endothelial function and decrease cardiovascular events.
In a single patient, we observed a positive correlation of hsCRP with disease severity based on PASI score who was admitted following a cardiovascular event after 1 month of treatment with apremilast.
Limitations
The study was carried out in the outpatient clinic of the dermatology department of a tertiary referral center, lack of blinding, psoriasis patients not stratified according to severity, and a small sample size were the major limitations.
CONCLUSION
The results of our study show that methotrexate is superior to apremilast in PASI reduction. In this study, 3-month treatment with methotrexate was found useful in decreasing the risk factors such as LDL, hsCRP, and triglyceride for the development of cardiovascular disease among patients with moderate to severe psoriasis. Apremilast seemed to have a lesser effect on the above risk factors.
Ethical approval
The ethical approval for this study was obtained from the institutional review board. Ethical committee number-17/EC/22/AIMS-78 dated-31-10-2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Glenmark Pharmaceuticals sponsored an ELISA kit for urinary thromboxane B2 assay.
References
- Psoriasis and cardiovascular diseases: A literature review to determine the causal relationship. Cureus. 2018;10:e2195.
- [CrossRef] [Google Scholar]
- Meta-analysis of psoriasis, cardiovascular disease, and associated risk factors. J Am Acad Dermatol. 2013;69:1014-24.
- [CrossRef] [PubMed] [Google Scholar]
- Markers of systemic inflammation inpsoriasis: A systematic review and meta-analysis. Br J Dermatol. 2013;169:266-82.
- [CrossRef] [PubMed] [Google Scholar]
- High-sensitivity C-reactive protein and cardiovascular risk: Rationale for screening and primary prevention. Am J Cardiol. 2003;92:17K-22.
- [CrossRef] [PubMed] [Google Scholar]
- High-sensitivity C-reactive protein, inflammation, and cardiovascular risk: From concept to clinical practice to clinical benefit. Am Heart J. 2004;148:S19-26.
- [CrossRef] [PubMed] [Google Scholar]
- Cumulative exposure to high-sensitivity C-reactive protein predicts the risk of cardiovascular disease. J Am Heart Assoc. 2017;6:e00561.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of C-reactiveprotein as a marker for prediction of future coronary events in the Asian Indian population: Indian atherosclerosis research study. Int J Vasc Med. 2010;2010:389235.
- [CrossRef] [PubMed] [Google Scholar]
- Role of C-reactive protein as a marker of disease severity and cardiovascular risk in patients with psoriasis. Indian Dermatol Online J. 2015;6:322.
- [CrossRef] [PubMed] [Google Scholar]
- Apremilast in psoriasis and beyond: Big hopes on a small molecule. Indian Dermatol Online J. 2019;10:1-12.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and cardiovascular comorbidities: Focusing on severe vascular events, cardiovascular risk factors and implications for treatment. Int J Mol Sci. 2017;18:2211.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of the efficacy of methotrexate with apremilast in moderate to severe chronic plaque psoriasis. Indian J Dermatol. 2023;68:393-8.
- [CrossRef] [PubMed] [Google Scholar]
- Methotrexate vs secukinumab safety in psoriasis patients with metabolic syndrome. Dermatol Ther. 2020;33:e14281.
- [CrossRef] [Google Scholar]
- Comparison between methotrexate and apremilast in psoriatic arthritis-a single blind randomized controlled trial (APREMEPsA study) Rheumatol Int. 2023;43:841-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative efficacy of methotrexate versus apremilast for methotrexate-naive psoriasis patients: An indirect comparison. Int J Am Acad Dermatol. 2015;72:229.
- [CrossRef] [Google Scholar]
- Comparison of the efficacy and safety of apremilast and methotrexate in patients with palmoplantar psoriasis: A randomized controlled trial. Am J Clin Dermatol. 2021;22:415-23.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and metabolic effect on serum lipids of apremilast in psoriatic arthritis: A case report. J Clin Med. 2019;8:398.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the glycemic effect of methotrexate in psoriatic arthritis patients with metabolic syndrome: A pilot study. Dermatol Rep. 2019;11:7965.
- [CrossRef] [PubMed] [Google Scholar]
- Worsening of lymphopenia during apremilast treatment. Case Rep Dermatol. 2017;8:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term safety of methotrexate monotherapy in patients with rheumatoid arthritis: A systematic literature research. Ann Rheum Dis. 2009;68:1100-4.
- [CrossRef] [PubMed] [Google Scholar]
- Does TNF-alpha blockade play any role in cardiovascular risk among rheumatoid arthritis (RA) patients? Clin Rheumatol. 2009;28:1217-20.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of apremilast, an oral inhibitor of phosphodiesterase 4, in a randomised trail of patients with active ulcerative colitis. Clin Gastroenterol Hepatol. 2020;18:2526-34.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of systemic psoriasis therapies on the C-reactive protein and the neutrophil-lymphocyte ratio. Ann Dermatol. 2019;31:601-10.
- [CrossRef] [PubMed] [Google Scholar]






