Translate this page into:
Quiz questions from dermoscopy of infectious dermatoses (Infectiouscopy/Entodermoscopy)
*Corresponding author: Vishal Gaurav, Department of Dermatology and Venereology, Maulana Azad Medical College, New Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Gowda P. Quiz questions from dermoscopy of infectious dermatoses (Infectiouscopy/Entodermoscopy). J Skin Sex Transm Dis. 2024;6:227-33. doi: 10.25259/JSSTD_32_2024
QUESTIONS:
-
Which dermoscopic feature is typically seen in cutaneous myiasis?
Bird’s feet-like structures
Yellowish structure with black spines
Thorn crown-like structures
All the above
-
Dermoscopy of tungiasis shows:
Yellowish crusts with central black dots
Pearly white nodules with a central black punctum
Whitish homogeneous lesion with a central brown pigmented ring
Red papules with central ulceration
-
A male patient presented with generalized itching, which worsened at night. He also reported similar symptoms in family members. On examination, multiple erythematous papules were observed in the finger web spaces and the periumbilical area. Dermoscopy findings are shown in Figure 1. What is the name of this dermoscopic sign?
 Figure 1:
Figure 1:- Dermoscopy (HeineDELTA one) of lesion on the palm (polarized; 10×).
Delta-wing jet with contrail
Setting sun sign
Little red riding hood sign
Jelly sign
-
In cutaneous leishmaniasis, the ‘white starburst-like pattern’ is observed during which stage?
Early lesions
Intermediate lesions
Late stages
Healing stages
-
‘Falooda seeds’ appearance on dermoscopy is seen in:
Palmoplantar warts
Filiform warts
Genital warts
Verruca plana
-
Figure 2 displays the ultraviolet dermoscopic image of a healthy individual’s face. Which organism is responsible for the characteristic fluorescence seen in this figure?
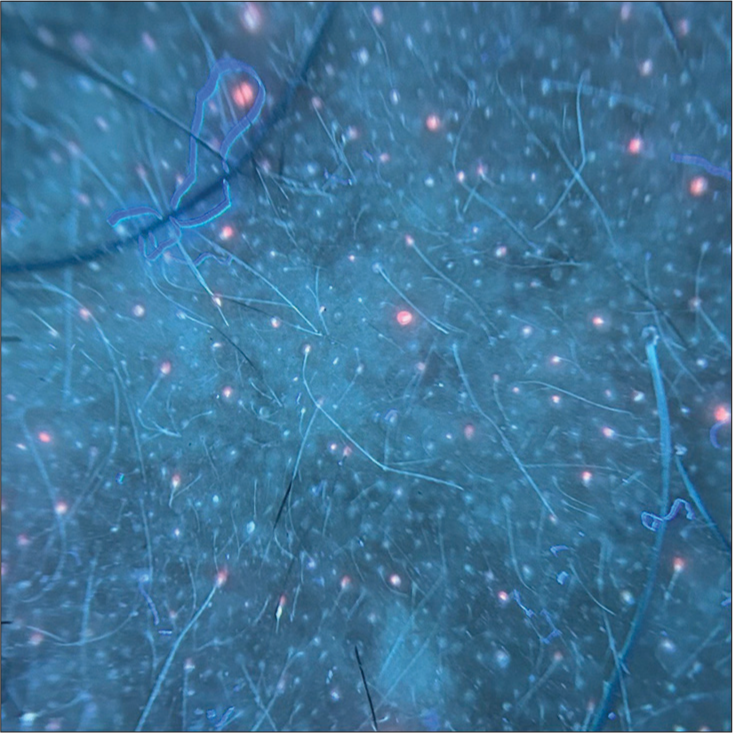 Figure 2:
Figure 2:- Ultraviolet-induced fluorescence dermoscopy (Dermlite DL5) of the face (10×).
-
What is the main dermoscopic feature of cutaneous larva migrans?
Brownish structureless areas in a segmental arrangement
Linear branching vessels
Central ulceration with scales
Yellowish nodules
-
Which pattern is commonly observed in the dermoscopy of molluscum contagiosum?
Blue-gray dots
Central yellowish-white polylobular amorphous structure
Brownish reticular pattern
Starburst pattern
-
A 25-year-old male patient presented with an unpleasant odor and yellowish discoloration of hair in both axillae. Dermoscopy was performed, and the findings are depicted in Figure 3. What dermoscopic signs are observed in this condition?
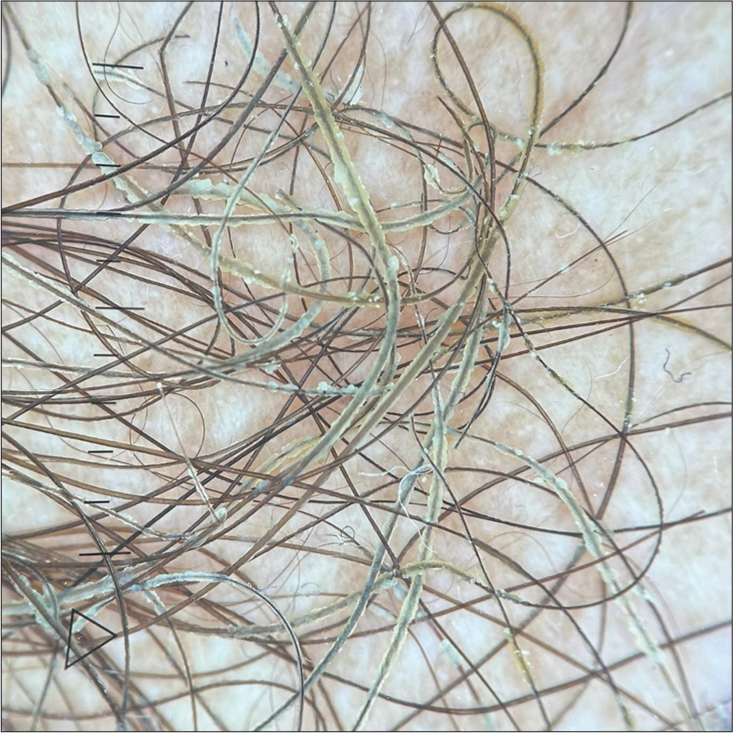 Figure 3:
Figure 3:- Trichoscopy (Dermlite DL5) of axillary hair (polarized; 10×).
-
Which of the following is a dermoscopic feature of lupus vulgaris?
Orange to golden background pigmentation
Linear telangiectasias
White structureless areas
All the above
-
Which of the following dermoscopic findings is indicative of white piedra?
Easily detachable white, bizarrely shaped, amorphous structures
Elongated tubular structures encircling the hair shaft and easily movable along it
Localized whitish areas along the hair shafts, resulting from fractured and frayed hair
White amorphous material locally encasing the hair
-
A 13-year-old girl presented with severe scalp itching for the past 3 months and has a history of similar complaints in her younger sister. Dermoscopy findings are shown in Figure 4. Which structures are seen?
 Figure 4:
Figure 4:- Trichoscopy (HeineDELTA one) of the scalp (non-polarized; 10×).
-
Whitish scales along plantar creases are seen on dermoscopy of:
Plantar warts
Plantar corn
Tinea pedis
Pitted keratolysis
-
In dermoscopy of Demodex folliculorum, what do whitish creamy threads suggest?
Tails
Body
Legs
Mouth parts
-
Which trichoscopic finding has the highest predictive value for diagnosing tinea capitis?
Black dots
Broken hairs
Comma hairs
Perifollicular scaling
-
Which trichoscopic feature is more commonly detected in Trichophyton tinea capitis compared to Microsporum tinea capitis?
Morse code-like hairs
Zigzag hairs
Bent hairs
Corkscrew hairs
-
What treatment should be recommended for a child with the dermoscopic findings depicted in Figure 5?
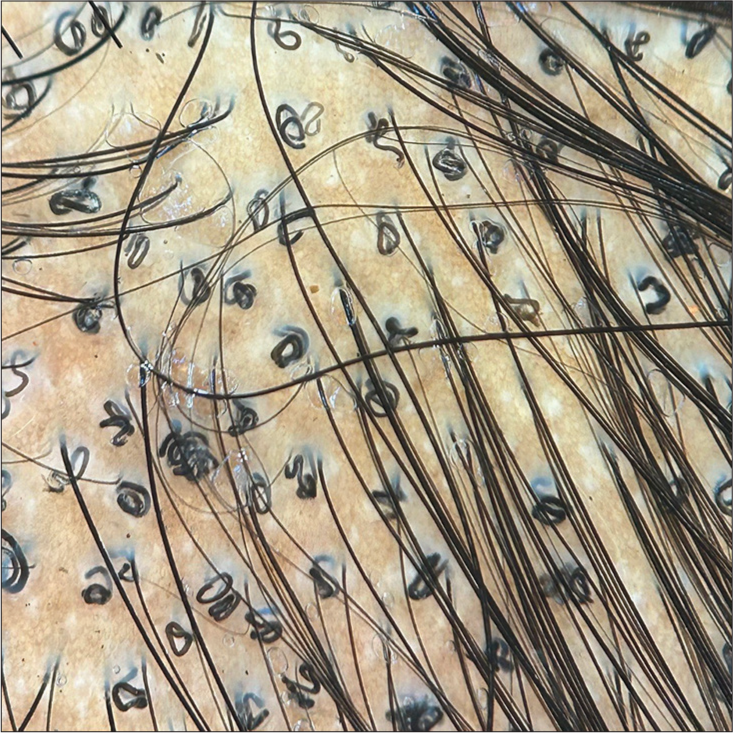 Figure 5:
Figure 5:- Trichoscopy (HeineDELTA one) of the scalp (polarized; 10×).
Griseofulvin
Itraconazole
Fluconazole
Terbinafine
-
Dermoscopy of pitted keratolysis typically shows:
Irregular whitish structures
Heterogeneous architecture at the periphery of the craters
Scales along ridges
Yellowish areas
-
The dermoscopic features of Cydnidae pigmentation are:
Clusters of numerous oval to shiny brown globules and granules
Bizarre-shaped pigmented structures
Accentuated pigmentation along skin furrows and eccrine openings
All the above
-
A 56-year-old woman presented with asymptomatic discoloration of her left thumb nail for the past year. Despite treatment with oral antifungals, there was no improvement. Onychoscopy is shown in Figure 6. What is the diagnosis and the name of the dermoscopic sign depicted in Figure 6?
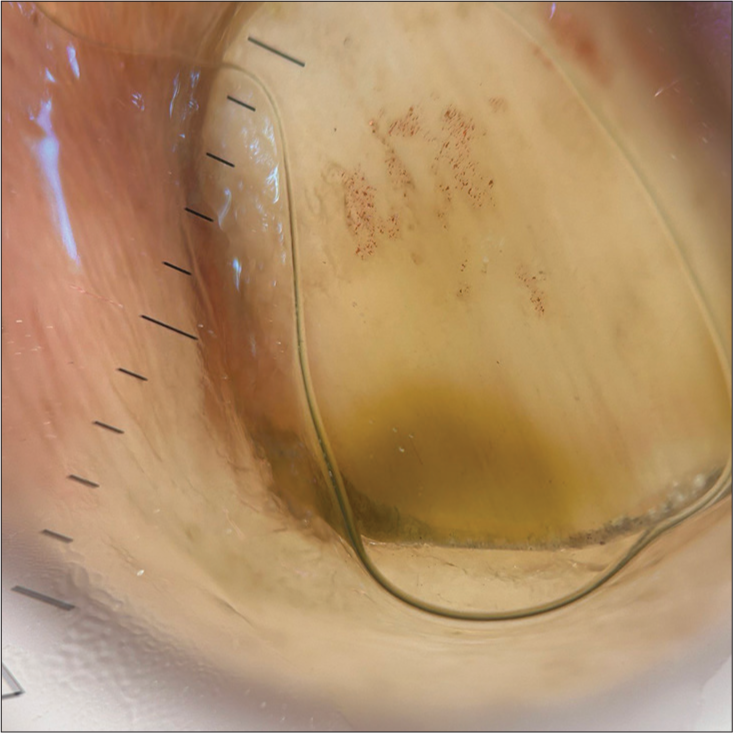 Figure 6:
Figure 6:- Onychoscopy (HeineDELTA one) of right ring fingernail (polarized; 10×).
-
Chick-pea flour pattern is seen on onychoscopy of:
White superficial onychomycosis
Endonyx
Distal lateral subungual onychomycosis
Proximal subungual onychomycosis
-
Which of the following onychoscopic signs has the highest sensitivity and specificity for the diagnosis of onychomycosis?
Ruin appearance
Longitudinal striae
Spikes on the proximal margin of onycholytic areas
Aurora borealis sign
-
Dendritic pattern on onychoscopy is seen in:
Distal lateral subungual onychomycosis
Proximal subungual onychomycosis
Superficial onychomycosis
Endonyx onychomycosis
-
Identify the onychoscopic sign shown in Figure 7 and specify the condition.
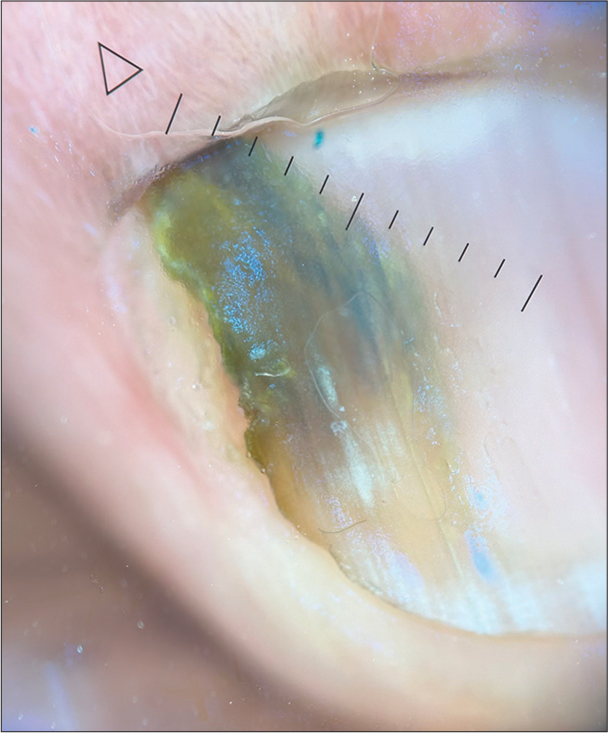 Figure 7:
Figure 7:- Onychoscopy (HeineDELTA one) of left ring fingernail (polarized; 10×).
-
Which of the following findings is specific to pityriasis versicolor as identified in dermoscopic studies?
White scales over a dull diffuse white or brown background
Folliculocentricity (perifollicular white halo)
Contrast halo sign (ring of alternate pigmentation surrounding the primary lesion)
All of the above
-
Which of the following dermoscopic features is commonly observed in leprosy across all its subtypes?
White structureless areas
Hyperpigmentation with irregular borders
Yellow/yellowish-orange areas
Peripheral hyperpigmentation
-
‘White jade coin pendant sign’ is a dermoscopic sign of:
Cutaneous histoplasmosis
Chromomycosis
Cutaneous talaromycosis
Basidiobolomycosis
-
A 12-year-old boy presented with multiple asymptomatic, skin-colored to hyperpigmented papules on his right hand. Dermoscopic examination is shown in Figure 8. What is the diagnosis?
 Figure 8:
Figure 8:- Dermoscopy (AM7115MZT Dino-Lite Edge 3.0 digital microscope) of lesions on the right hand (polarized; 10×).
-
Which of the following diseases shows a ‘noodle pattern’ on dermoscopy?
Crusted scabies
Myiasis
Tungiasis
Phthiriasis
-
A 45-year-old female presented with acute onset painful grouped vesicular eruption of the right side of her abdomen extending to the back. Dermoscopy findings are shown in Figure 9. What is the name of this dermoscopic sign and what is the diagnosis?
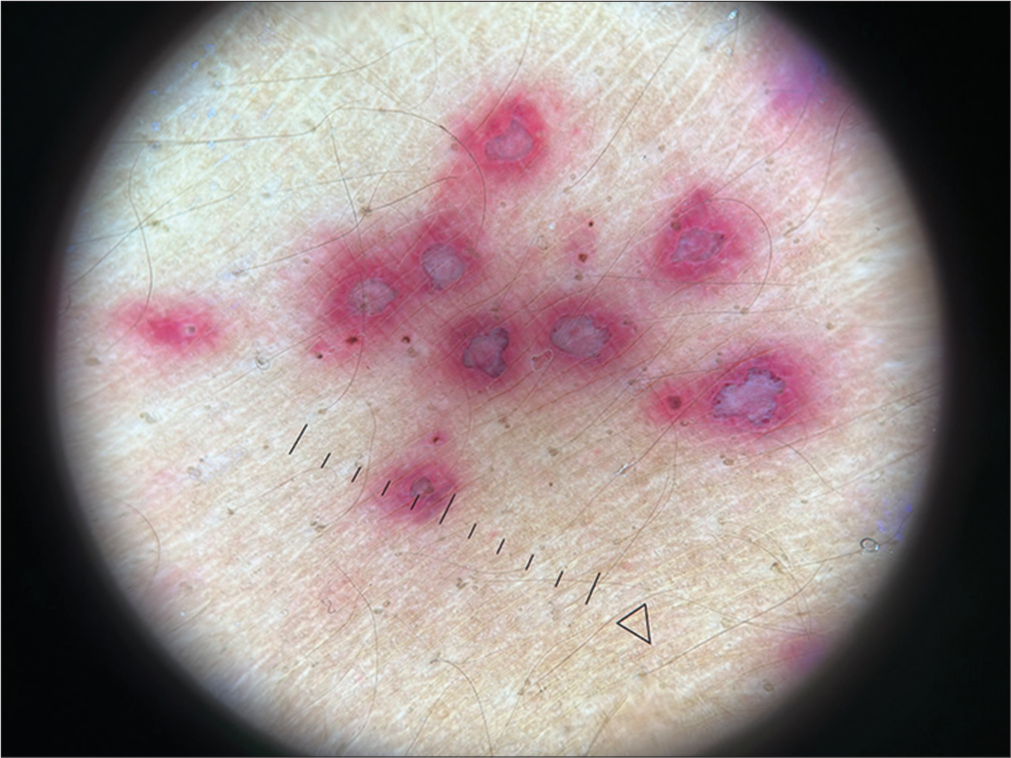 Figure 9:
Figure 9:- Dermoscopy (HeineDELTA one) of lesions on the abdomen (polarized; 10×).
ANSWERS:
(d). Cutaneous myiasis is caused by the larval stage of different botflies. Dermoscopy of furuncular myiasis reveals bird feet-like structures corresponding to respiratory spiracles, yellowish structures with black barb-like spines extruding from the periphery, and a thorn-crown appearance due to black dots on the outer edge of the larva.[1]
(c). A whitish homogeneous lesion with a central brown pigmented ring is characteristic of tungiasis, which is caused by the female sand flea (Tunga penetrans and Tunga trimamillata). The white areas correspond to the parasite’s dilated abdomen containing eggs, while the central light brown structure corresponds to the posterior segment of the parasite.[2]
(a). Delta-wing jet with contrail (jet with trail) sign. It represents the burrow with the mite at the end, appearing as a dark triangle (mite; black arrow) followed by a thin, wavy line (burrow; blue arrow).[3,4]
(c). Dermoscopic examination of early lesions of cutaneous leishmaniasis reveals yellow tear-shaped structures and vessels, whereas late lesions display a starburst pattern with peripheral vascular structures.[4,5]
(a). Dermoscopy of palmoplantar warts reveals hemorrhagic and thrombosed black dots and globules, surrounded by a white halo, resembling wet basil seeds in falooda.
Answer: Cutibacterium acnes. Sebaceous gland openings exhibit fluorescence under ultraviolet light, which ranges in color from bright blue/green to yellow, orange, or red. This characteristic fluorescence can be particularly useful in diagnosing and monitoring acne vulgaris. Notably, orange fluorescence is due to the presence of porphyrins produced by C. acnes (formerly Propionibacterium acnes).[8,9]
(a). Dermoscopy of cutaneous larva migrans reveals translucent, brownish, structureless areas arranged segmentally, corresponding to the body of the larva. In addition, dotted vessels representing empty burrows can also be observed.[10]
(b). Dermoscopy of molluscum contagiosum typically reveals a central white-yellowish polylobular amorphous structure, surrounded by a crown of vessels.[11,12]
Skewer sign and plume sign. Trichoscopy reveals golden-yellow, cotton-like deposits sticking to the affected hair shafts. A detailed view may show nodules and deposits with a flame-like appearance. Some hair shafts display waxy, yellowish nodules and deposits along their entire length, a feature referred to as the skewer sign. In addition, a localized pale-yellowish nodule can produce what is known as the plume sign.[13,14]
(d). Dermoscopy of lupus vulgaris reveals a yellow background pigmentation with linear telangiectasias, which corresponds to the clinically observed apple jelly sign. This sign can also be seen in other granulomatous conditions. Lupus vulgaris additionally presents with white structureless areas, follicular plugs, yellow-white scales, dilated follicles, and erythema.[4,15]
(d). White piedra presents as white amorphous material locally encasing the hair Dermoscopy of seborrheic dermatitis reveals easily detachable white, bizarrely shaped, amorphous structures. Elongated tubular structures that encircle the hair shaft and are easily movable along it, known as hair casts, can be seen in traction alopecia, folliculitis decalvans or idiopathically. Trichobacteriosis is identified by waxy and yellowish/whitish adherent aggregates forming a sheath around the axillary hair shaft. Trichorrhexis nodosa is characterized by localized whitish areas along the hair shafts, resulting from fractured and frayed hair.[13,14,16]
In vivo dermoscopy can identify three stages of nits: active viable nits are ovoid, whitish-brown structures containing eggs or viable embryos, located close to the scalp; abortive nits are translucent with a condensed non-viable embryo and a dehiscing operculum, found about 5 mm or farther from the scalp; and empty nits are translucent whitish crystalline structures without an operculum, typically more than 1 cm away from the scalp.[4,17]
(c). Dermoscopy of tinea pedis and manuum shows whitish scales along creases and brownish scales corresponding to dried vesicles.[18]
(a). Dermoscopy of demodicosis reveals two distinct features: whitish, creamy, gelatinous threads known as Demodex tails, and dilated follicular openings containing gray or brown amorphous round plugs, which are surrounded by an erythematous halo, referred to as Demodex follicular openings.[19]
(c). The most indicative trichoscopic findings of tinea capitis, known for their high predictive value, include comma hairs (51%), corkscrew hairs (32%), Morse code-like hairs (22%), zigzag hairs (21%), bent hairs (27%), block hairs (10%), and i-hairs (10%). In addition, other frequently observed but less characteristic trichoscopic features are broken hairs (57%), black dots (34%), perifollicular scaling (59%), and diffuse scaling (89%).[20,21]
(d). Morse code-like hairs, zigzag hairs, bent hairs, and diffuse scaling are exclusively found in cases of Microsporum tinea capitis, occurring in 28%, 21%, 14%, and 14% of cases, respectively. In contrast, corkscrew hairs are more frequently observed in Trichophyton tinea capitis, with a prevalence of 55% compared to 10% in Microsporum tinea capitis.[20,21]
(d). In Trichophyton tinea capitis, corkscrew hairs were more commonly detected compared to Microsporum tinea capitis (21/38, 55% vs 3/29, 10%).[20] Given that corkscrew hairs are the main finding in the image, the likely causative organism is Trichophyton, so terbinafine should be used for treatment.[22]
(b). Dermoscopy of pitted keratolysis shows pits and heterogenous architecture at the periphery of craters.[23]
(d). Cydnidae pigmentation is caused by burrowing bugs. Their odorous secretions stain the skin. Dermoscopy shows brown globules and granules, bizzare-shaped pigmented structures, and accentuation of pigmentation along skin furrows and eccrine openings.[24]
Green nail syndrome and green aurora sign. It is caused by Pseudomonas aeruginosa and the greenish discoloration occurs due to pyocyanin pigment. On onychoscopy, ‘green aurora’ sign is visualized.[25]
(a). The ‘chick-pea flour pattern’ in white superficial onychomycosis refers to yellowish-white, opaque, and friable debris on the nail plate, predominantly near the proximal nail fold.[26]
(d). The primary dermoscopic indicators of onychomycosis include the ‘ruin appearance,’ ‘longitudinal striae,’ and ‘spikes’ located at the proximal edge of onycholytic areas, with specificities of 99.38%, 83.78%, and 85.64%, respectively. The ‘aurora borealis’ sign demonstrated the greatest sensitivity and specificity.[27]
(d). Dendritic pattern is seen in endonyx onychomycosis.[28]
Aurora borealis sign, seen in distal lateral subungual onychomycosis. Aurora borealis represents areas of various colors ranging from whitish yellow to greenish-blue to bluish-gray to black in onycholytic areas.[27]
(d). In both hypo- and hyperpigmented variants of pityriasis versicolor, white scales in skin furrows over a dull white or brown background are key dermoscopic characteristics. In addition, perifollicular white scaling, ‘contrast halo sign,’ a ring of alternating pigmentation around the main lesion, and folliculocentricity are also described.[29,30]
(c). Yellow or yellowish-orange areas are among the most common dermoscopic findings observed in all subtypes of leprosy, making it a reliable marker for the disease in dermoscopic examinations.[30,31]
(c). The ‘white jade coin pendant sign’ in Talaromyces marneffei infection is characterized by a circular or nearly circular whitish amorphous structure with a central keratin plug or hemorrhage.[32,33]
Verruca vulgaris. The dermoscopic characteristics of common warts include brown dots, dotted vessels, and black dots or globules (indicative of thrombosed vessels) against a white background.[4,30]
(a). Noodle pattern is seen on dermoscopy of crusted scabies due to congregation of multiple burrows at one site.[34]
‘Halo sign’ of herpes zoster. The ‘halo sign’ results from the contrast between the yellowish-brown crusted center of the vesicular lesions and the red hue of the erythematous background, forming an annular pattern around each vesicle.[35-37]
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermoscopy features for the diagnosis of furuncular myiasis. An Bras Dermatol. 2011;86:160-2.
- [CrossRef] [Google Scholar]
- Tungiasis under dermoscopy: In vivo and ex vivo examination of the cutaneous infestation due to Tunga penetrans. An Bras Dermatol. 2013;88:649-51.
- [CrossRef] [Google Scholar]
- Ungual scabies: A case report and review of literature. Skin Appendage Disord. 2024;10:60-8.
- [CrossRef] [Google Scholar]
- Entodermoscopy update: A contemporary review on dermoscopy of cutaneous infections and infestations. Indian Dermatol Online J. 2021;12:220-36.
- [CrossRef] [Google Scholar]
- Dermoscopy in the diagnosis of cutaneous leishmaniasis. Dermatol Pract Concept. 2019;9:111-8.
- [CrossRef] [Google Scholar]
- Dermatoscopy of palmar wart with falooda seed appearance. Australas J Dermatol. 2018;59:155-6.
- [CrossRef] [Google Scholar]
- Advancements in dermatological imaging modalities. Indian Dermatol Online J. 2024;15:278-92.
- [CrossRef] [Google Scholar]
- Ultraviolet reflectance dermoscopy. Indian J Dermatol Venereol Leprol 2024:10.25259/IJDVL_1308_2023. https://ijdvl.com/ultraviolet-reflectance-dermoscopy/
- [CrossRef] [Google Scholar]
- Hallazgos dermatoscópicos en larva migrans [Dermoscopic findings in cutaneous larva migrans] Dermatol Rev Mex. 2015;59:98-101.
- [Google Scholar]
- Dermoscopy of molluscum contagiosum: A useful tool for clinical diagnosis in adulthood. J Eur Acad Dermatol Venereol. 2006;20:482-3.
- [CrossRef] [Google Scholar]
- Dermoscopy of molluscum contagiosum with orifice-single lesion in an adult. CosmoDerma. 2024;4:91.
- [CrossRef] [Google Scholar]
- Trichobacteriosis pubis presenting as genital bromhidrosis. Indian Dermatol Online J 2024 https://journals.lww.com/idoj/fulltext/9900/trichobacteriosis_pubis_presenting_as_genital.208.aspx [Last accessed on 2024 July 24]
- [CrossRef] [Google Scholar]
- Ultraviolet-induced fluorescence trichoscopy of trichobacteriosis axillaris. J Skin Sex Transm Dis. 2024;6:217-8.
- [CrossRef] [Google Scholar]
- Lupus vulgaris in darker skin: Dermoscopic and histopathologic incongruity. Indian Dermatol Online J. 2020;11:948-52.
- [CrossRef] [Google Scholar]
- White piedra: An uncommon superficial fungal infection of hair. Skin Appendage Disord. 2022;8:34-7.
- [CrossRef] [Google Scholar]
- Dermoscopy for diagnosis and treatment monitoring of pediculosis capitis. J Am Acad Dermatol. 2006;54:909-11.
- [CrossRef] [Google Scholar]
- Can dermoscopy serve as a diagnostic tool in dermatophytosis? A pilot study. Indian Dermatol Online J. 2019;10:530-5.
- [CrossRef] [Google Scholar]
- Dermoscopy as a diagnostic tool in demodicidosis. Int J Dermatol. 2010;49:1018-23.
- [CrossRef] [Google Scholar]
- Trichoscopy of tinea capitis: A systematic review. Dermatol Ther (Heidelb). 2020;10:43-52.
- [CrossRef] [Google Scholar]
- Kerion celsi caused by Trichophyton mentagrophytes Clinical, trichoscopic, and microscopic features. CosmoDerma. 2024;4:70.
- [CrossRef] [Google Scholar]
- Meta-analysis of randomized, controlled trials comparing griseofulvin and terbinafine in the treatment of tinea capitis. J Am Acad Dermatol. 2011;64:663-70.
- [CrossRef] [Google Scholar]
- Demystifying the stinking reddish brown stains through the dermoscope: Cydnidae pigmentation. Indian Dermatol Online J. 2019;10:757-8.
- [CrossRef] [Google Scholar]
- Dermoscopy of green nail syndrome-The “green aurora sign”. Dermatol Pract Concept. 2021;11:e2021093.
- [CrossRef] [Google Scholar]
- The grid pattern of white superficial onychomycosis. Indian J Dermatol Venereol Leprol. 2020;86:568-70.
- [CrossRef] [Google Scholar]
- Dermoscopy of onychomycosis: A systematic review. Dermatol Pract Concept. 2023;13:e2023072.
- [CrossRef] [Google Scholar]
- Dendritic pattern: Unique onychoscopic feature in endonyx. J Am Acad Dermatol. 2019;81:e89-90.
- [CrossRef] [Google Scholar]
- Dermoscopic pattern of pityriasis versicolor. Clin Cosmet Investig Dermatol. 2019;12:303-9.
- [CrossRef] [Google Scholar]
- Dermoscopy of infectious dermatoses (infectiouscopy) in skin of color-a systematic review by the International Dermoscopy Society “Imaging in Skin of Color” Task Force. Dermatol Pract Concept. 2023;13(4 S1):e2023309S.
- [CrossRef] [Google Scholar]
- Dermoscopy in leprosy: A clinical and histopathological correlation study. Dermatol Pract Concept. 2021;11:e2021032.
- [CrossRef] [Google Scholar]
- AIDS-associated disseminated talaromycosis (penicilliosis) marneffei. J Dtsch Dermatol Ges. 2018;16:1256-9.
- [CrossRef] [Google Scholar]
- Dermatoscopy for the rapid diagnosis of Talaromyces marneffei infection: A case report. BMC Infect Dis. 2019;19:707.
- [CrossRef] [Google Scholar]
- Noodle pattern: A new dermoscopic pattern for crusted scabies (Norwegian scabies) J Eur Acad Dermatol Venereol. 2018;32:e46-7.
- [CrossRef] [Google Scholar]
- Dermoscopic features of herpes zoster: Case series and review of the literature. Dermatol Pract Concept. 2023;13:e2023149.
- [CrossRef] [Google Scholar]
- Herpes zoster maxillaris: Clinical, dermoscopic, and microscopic features. J Skin Sex Transm Dis. 2024;6:215-6.
- [CrossRef] [Google Scholar]
- Acute localised exanthematous pustulosis: A rare cause of localised sterile pustules. Indian J Dermatol. 2022;67:428-31.
- [CrossRef] [Google Scholar]






