Translate this page into:
Rare co-occurrence of acquired epidermodysplasia verruciformis with eccrine porocarcinoma
*Corresponding author: Veril Vaz, Department of Dermatology, Father Muller Medical College, Mangaluru, Karnataka, India. vrlvaz96@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vaz V, Bhat RM, Fernandes MS. Rare cooccurrence of acquired epidermodysplasia verruciformis with eccrine porocarcinoma. J Skin Sex Transm Dis. doi: 10.25259/JSSTD_63_2024
Abstract
Epidermodysplasia verruciformis (EV), linked to weakened immunity against specific human papillomavirus strains, poses a heightened risk of cutaneous dysplasia and malignancy. EV often leads to malignancies like squamous cell carcinoma. This case details a 25-year-old immunocompromised male presenting furfuraceous lesions and a peculiar scalp nodule. Following wide local excision and biopsies, eccrine porocarcinoma an uncommon malignancy associated with viral induction was diagnosed. Managing such cases poses significant challenges for surgeons and oncologists due to the rarity, morphological distinctiveness, and diagnostic ambiguities, which require adequate interprofessional team effort.
Keywords
Eccrine porocarcinoma
Epidermodysplasia verruciformis
Immunocompromised state
Skin malignancy
INTRODUCTION
Epidermodysplasia verruciformis (EV), or Lewandowsky-Lutz dysplasia, is a rare disorder marked by chronic, widespread human papillomavirus (HPV) infection, impaired cell-mediated immunity, and an increased risk of skin cancers like squamous cell carcinoma.[1] Eccrine porocarcinoma (EPC), a rare malignant sweat gland tumor, may develop spontaneously or from an eccrine poroma.[2] The simultaneous occurrence of both conditions in the same patient is exceedingly rare, with only a few documented cases.
CASE REPORT
A 25-year-old manual laborer presented with persistent, asymptomatic whitish flat-topped and dark raised skin lesions over the body since childhood, initially occurring over the trunk, which were progressive over 20 years. Notably, concerns emerged regarding a significant large lesion on the left side of the scalp that rapidly developed over the preceding 2 months, accompanied by bleeding and oozing. No similar lesions were noted in any other family members. He had a history of Hodgkin’s lymphoma involving cervical, mediastinal, and axillary lymph nodes diagnosed 2 years ago, for which he underwent eight cycles of adriamycin, bleomycin, vinblastine and dacarbazine chemotherapy and field radiation therapy.
On cutaneous examination, hyperpigmented warty papules and plaques were observed alongside hypopigmented flat-topped macules resembling lesions of pityriasis versicolor. On the left side of the scalp, a single 8 × 7 cm ulceroproliferative growth displayed firm to hard consistency, featuring areas of hemorrhage and necrosis [Figure 1]. Laboratory tests returned within-normal-range results. Computed tomography of the brain revealed multiple intracranial granulomas with calcifications. Incisional biopsy of the scalp mass revealed features suggestive of a malignant adnexal tumor.

- (a): Warty seborrheic keratosis-like papules (red circle) and hypopigmented versicolor-such as macules and plaques (black circle); (b): ulceroproliferative growth on the scalp.
Histological examination of both skin lesions showed hyperkeratosis, acanthosis, and hypergranulosis. In the granular and upper spinous layers, keratinocytes exhibited cellular ballooning, enlargement with gray-blue cytoplasmic pallor, coarse cytoplasmic keratohyalin granules, and an occasional perinuclear halo. These findings were suggestive of EV. Histopathological examination of the scalp mass revealed an ulcerated epidermis with tumor arranged in anastomosing cords and sheets. Individual tumor cells displayed cells with atypia with cuboidal morphology, vesicular pleomorphic nuclei, inconspicuous nucleoli, and moderate to scant cytoplasm with brisk mitosis. There was a presence of abortive duct formation with sebaceous and trichilemmal differentiation [Figure 2]. Certain areas had keratin pearl formation as well. All these were suggestive of a malignant adnexal tumour, EPC.
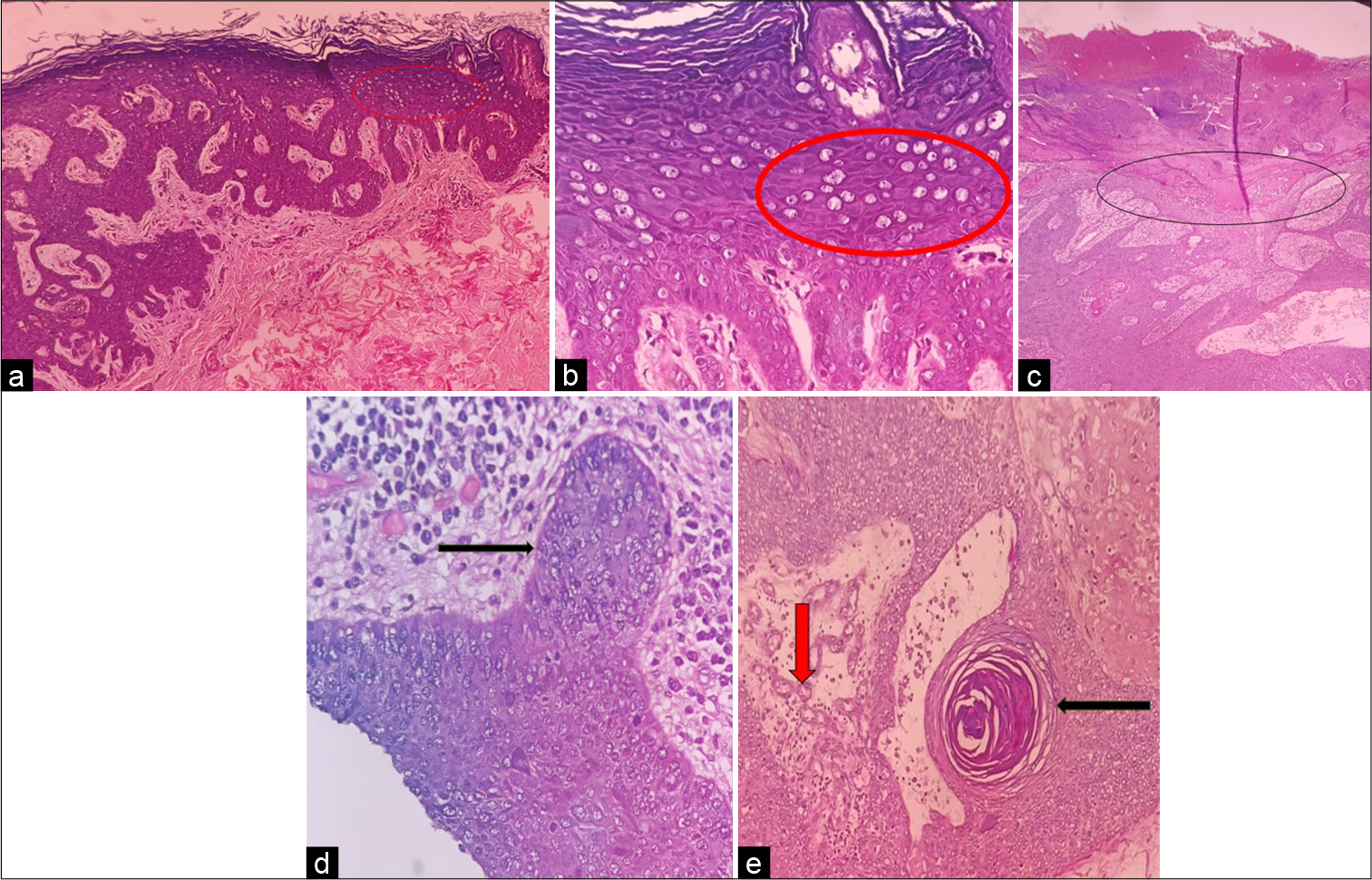
- (a): Histopathological examination under hematoxylin and eosin (H&E) staining of the skin lesion showing hyperkeratosis and hypergranulosis with cellular ballooning with gray-blue cytoplasm and occasional perinuclear halo marked in red circle under low power (x10); (b): cellular ballooning with gray-blue cytoplasm and occasional perinuclear halo marked in red circle under high power; (c): H&E staining of the ulcerative mass of scalp shows ulcerated epidermis with dermal invasion under ×10; (d): individual cuboidal tumor cells with anaplasia and brisk mitosis with arrangement in cords and sheets under ×40; and (e): abortive duct formation (red arrow) and sebaceous and trichilemmal differentiation (black arrow) with formation of keratin pearls under ×10.
Immunohistochemistry of the growth on the scalp demonstrated positive staining for cytokeratin (CK) 5/6, epithelial membrane antigen (EMA), BER EP4, p40, and a Ki67 positivity exceeding 70%, indicative of a malignancy with squamous differentiation [Figure 3]. HPV serotyping could not be performed due to the lack of such facilities.
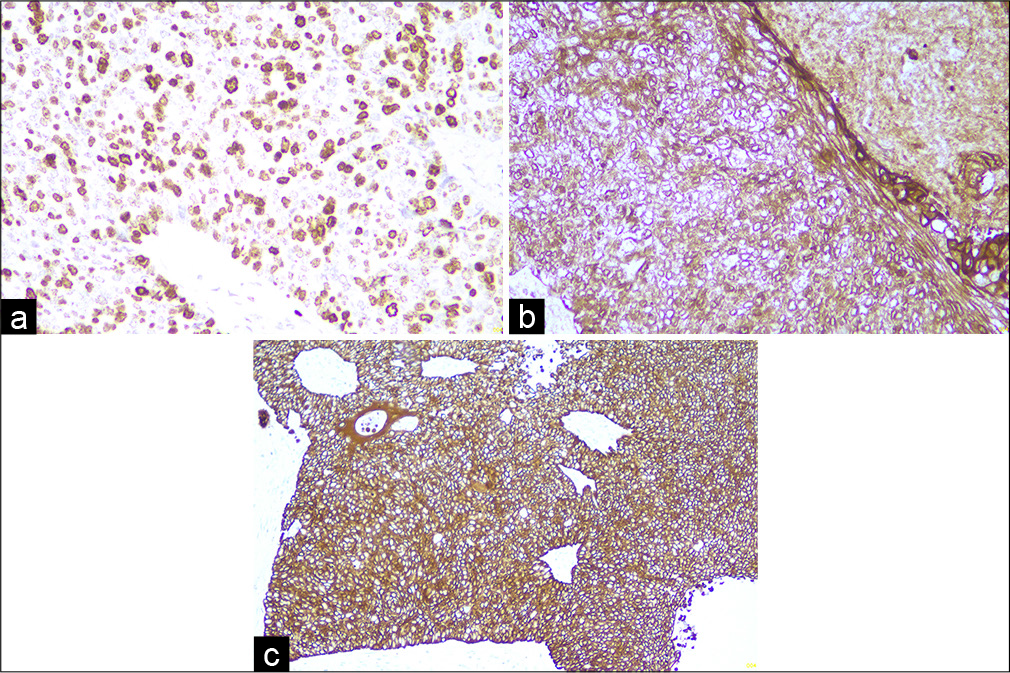
- (a): Immunohistochemistry shows ki67 positive (more than 70%) 40x; (b): epithelial membrane antigen positive under 40x; and (c) cytokeratin-5/6 positive under 40x.
The patient was diagnosed with an acquired form of EV with EPC.
DISCUSSION
EV is a rare autosomal recessive immune disorder marked by increased susceptibility to cutaneous HPV infections, typically beginning in early childhood. Mutations in the EVER1 or EVER2 genes on chromosome 17q25 leave individuals highly vulnerable to specific EV-related HPV types. This defect in cell-mediated immunity raises the oncogenic potential of HPV types 5 and 8, and less commonly 14, 17, 20, and 47. In both inherited and acquired forms, EV presents as flat, verruca plana like, often scaly, lesions primarily affecting the trunk, neck, or face, and sometimes resembling pityriasis versicolor.[3]
EPC is a rare malignant adnexal tumor originating from terminal cells of the eccrine duct, primarily affecting older adults, with a peak incidence in the sixth to eighth decades. Risk factors include radiation exposure and immunosuppression. EPC may arise spontaneously or from benign lesions such as poromas, nevus sebaceous, or actinic lesions and is typically found on the lower extremities and head, though other areas are also affected. Clinically, EPC appears as an asymptomatic erythematous or violaceous nodule, occasionally ulcerative and painful, often misdiagnosed as squamous cell carcinoma due to its similarity of presentation.[4]
A high mitotic index, presence of lymphovascular invasion, and tumor depth exceeding 7 mm are histopathological markers linked to a poor prognosis. Immunohistochemistry is a valuable diagnostic tool, although no specific marker exists for eccrine cells. EPCs commonly exhibit positive staining for keratin, EMA, carcinoembryonic antigen, CK, p53, and p63.[5]
The simultaneous occurrence of both rare conditions in the same patient is extremely rare, with only a handful of cases reported in the literature. In our patient, the possible trigger for the occurrence and progression of malignancy is the presence of immunosuppression caused due to prior history of lymphoma and the treatment for the same. Table 1 highlights the comparison between our case report and case reports by Singh et al.[6] and Souza et al.[7]
| Parameters | Our case report | Singh et al. | Souza et al. |
|---|---|---|---|
| Age and gender | 25-year old male | 35-year old female | 33-year old male |
| Consanguinity in parents | Non-consanguinous | Non consanguinous | Consanguinous |
| Previous history of Malignancy in the patient or relatives | Hodgkin's lymphoma in the patient | Squamous cell carcinoma in the patient's maternal uncle | Squamous cell carcinoma in the patient |
| Duration of the tumor | 2 months | 6 months | 8 months |
| Presentation of the adnexal tumor | An ulceroproliferative growth over the left side of the scalp | Multiple polypoidal nodules associated with foul-smelling discharge over the lower back. | Infiltrated and keratotic plaque measuring approximately 1 cm along its longest axis on the upper lip |
| Histopathology of the tumor | Tumor arranged in anastomosing cords and sheets. Individual tumor cells displayed cells with atypia with brisk mitosis. There is a presence of abortive duct formation | The individual tumor cells were cuboidal with pleomorphic vesicular nuclei and prominent nucleoli, arranged in cords and sheets. Abnormal mitoses and duct formation were also seen | A malignant epithelial neoplasm involving the epidermis and dermis consisting of numerous clear cells with nuclear atypia. Areas with ductal differentiation were seen, mainly in the dermal component. |
| Immunohistochemistry | Positive staining for cytokeratin 5/6, epithelial membrane antigen (EMA), BER EP4, p40, and a Ki67 positivity exceeding 70% | Not mentioned | Focally positive for EMA and carcinoembryonic antigen |
| HPV Subtyping | Was not done | Not mentioned | HPV- 14d via nested polymerase chain reaction. |
| Treatment of the tumor | Wide local excision with skin grafting | Not mentioned | Tumor excision ofthe lip plaque |
HPV: Human papillomavirus
CONCLUSION
This case highlights the acquired form of EV in an immunocompromised patient, likely due to prior chemotherapy. It emphasizes the development of a rare cutaneous malignancy, possibly triggered by chemotherapy. The rarity, unique morphology, and resemblance to other carcinomas make diagnosis and treatment particularly challenging. The concurrent occurrence of both rare conditions is extremely rare, with only a few reported cases. A high level of clinical suspicion is crucial for early intervention to prevent bad prognosis.
Ethical approval
The research/study approved by the Institutional Review Board at Father Muller Institutional Ethics Committee, number FMIEC/CCM/036/2024, dated January 24, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Lewandowsky and lutz dysplasia: Report of two cases in a family. Indian J Dermatol. 2011;56:190-3.
- [CrossRef] [PubMed] [Google Scholar]
- Eccrine porocarcinoma: A review of the literature. Diagnostics (Basel). 2023;13:1431.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermodysplasia verruciformis: An early and unusual presentation. Can J Plast Surg. 2010;18:21-4.
- [CrossRef] [PubMed] [Google Scholar]
- Eccrine porocarcinoma: A challenging diagnostic and therapeutic tumoral entity. Case Rep Oncol. 2021;14:700-5.
- [CrossRef] [PubMed] [Google Scholar]
- Eccrine porocarcinoma (malignant eccrine poroma): A clinicopathologic study of 69 cases. Am J Surg Pathol. 2001;25:710-20.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermodysplasia verruciformis-report of familial occurrence and a rare association with eccrine porocarcinoma. Indian J Dermatol. 2022;67:418-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clear cell porocarcinoma arising in an epidermodysplasia verruciformis patient. Indian J Dermatol. 2021;66:330.
- [CrossRef] [PubMed] [Google Scholar]







